Definition: Acute inflammatory process of the pancreas; a retroperitoneal organ with endocrine and exocrine function.
Epidemiology (Rosen’s 2018)
- US Incidence: 5 – 40/100,000
- Mortality: 4-7%
- Progression to severe disease: 10-15% of cases (mortality in this subset 20-50%)

Pancreas Anatomy (Rosen’s)
Etiology
- Alcohol (~ 35% of cases)
- Gallstones (~ 45% of cases)
- Medications/toxins
- Hypertriglyceridemia
- Non-gallstone Obstruction (i.e. strictures, masses)
- Trauma
- Infectious (Mumps, HIV, Salmonella)
Pathophysiology
- Mild Pancreatitis
- Results from obstruction of the pancreatic or bile ducts or direct toxicity to pancreatic cells
- Inflammation results in pancreatic enzyme activation within the pancreas and ducts
- Premature enzyme activation leads to pancreatic autodigestion
- Moderate Pancreatitis
- Enzyme digestion leads to necrosis of the pancreas
- Erosion into vascular structures can occur as well leading to hemorrhage
- Severe Pancreatitis
- Release of systemic inflammatory mediators
- systemic immune response syndrome and multisystem organ dysfunction (i.e. acute renal failure, cardiac dysfunction, ARDS, disseminated intravascular coagulation)
Presentation
- History + Symptoms
- Abdominal pain
- Typically epigastric but may be RUQ or LUQ
- Will become more diffuse as inflammation progresses
- Rapid onset of pain over a few hours
- Pain is constant, often severe and often radiates to the back (>50%)
- Nausea and vomiting (90%) (Banks 2006)
- Patients often have a history of prior similar episodes
- Dyspnea: Severe pancreatitis can present with dyspnea from diaphragmatic irritation or ARDS
- Abdominal pain
-

Cullen’s Sign
Signs
- Vital sign abnormalities dependent on stage of disease
- Early on may be normal or with slight tachycardia in response to pain
- Later in disease, hypotension, tachycardia and frank shock may develop
- Low grade fever common
- Epigastric tenderness with or without peritoneal signs
- Jaundice: indicates obstruction of common bile duct as etiology
- Hemorrhagic pancreatitis
- Rare complication
- Ecchymosis/discoloration around the umbilicus (Cullen’s sign)
- Ecchymosis/discoloration of the flank(s) (Grey Turner’s sign)
- Vital sign abnormalities dependent on stage of disease
Differential Diagnosis
- Abdominal Pathology
- Perforated viscus
- Peptic ulcer
- Biliary colic
- Cholecystitis
- Cholangitis
- Bowel obstruction
- Abdominal aortic aneurysm
- Ectopic pregnancy
- Cardiopulmonary Pathology
- Acute myocardial infarction
- ARDS
- Pericarditis
Diagnostics
- Basic Diagnostic Criteria (must have at least 2 out of 3)
- Signs/symptoms consistent with pancreatitis
- Lipase elevation: > 3X normal reference range (value depends on lab)
- Imaging (CT scan) consistent with pancreatitis
-
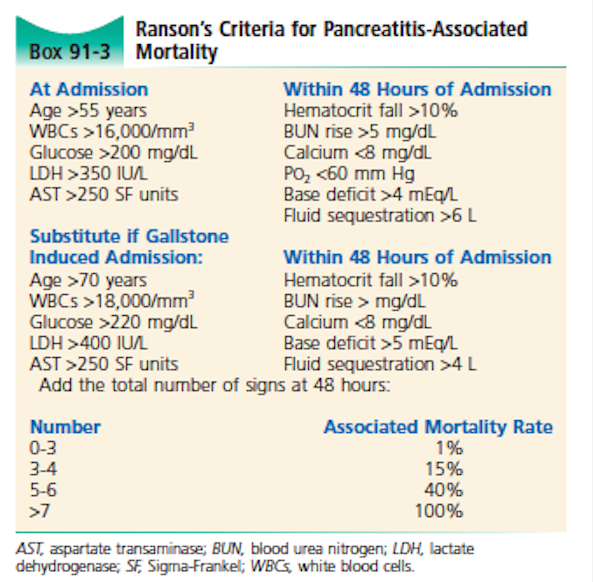
Ranson’s Criteria for Pancreatitis-Associated Mortality (Rosen’s)
Diagnostic Laboratory Tests
- Amylase
- Enzyme produced by pancreas, salivary glands, muscle, intestines and other organs
- Nonspecific marker of pancreatitis as can be elevated as result of various disease processes (Matsull 2006)
- May not be elevated in alcohol pancreatitis (>20%)
- May not be elevated if late presentation (>24h) of pancreatitis (amylase levels return to normal quickly)
- Lipase
- Enzyme more specific to pancreas than amylase
- Specificity: 80-99% depending on where cutoff set (Matsull 2006)
- False negatives may occur early in disease (levels increase in 4-8 hours of onset of inflammation)
- Degree of elevation is not a marker of disease severity
- Triglyceride Level
- Should be obtained in the absence of gallstone or alcohol as the likely etiology
- A level > 1000 mg/dl is suggestive that hypertriglyceridemia may be the cause (Tenner 2013)
- Amylase
- Ranson’s Criteria
- Aids in determining risk of mortality from pancreatitis
- Higher score = greater risk of mortality
- Labs required: CBC, BMP, Hepatic Panel, LDH
-
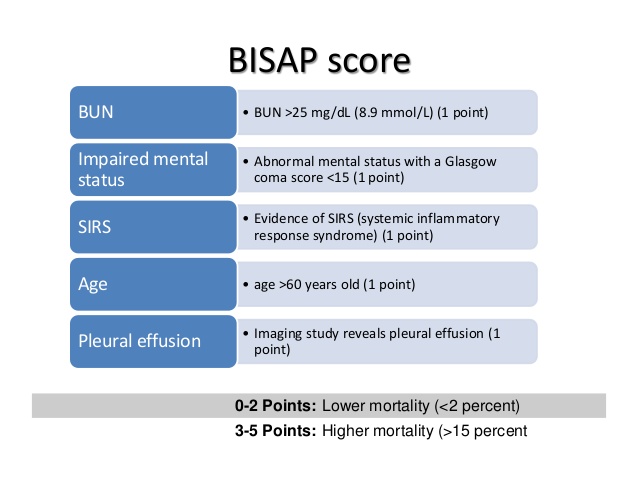
BISAP Score
BISAP Score (Wu 2008, Papachristou 2010)
- Clinical score used to predict mortality from pancreatitis
- Requires less tests than Ranson’s criteria but performs equally well
- Additional Laboratory Tests
- Basic Metabolic Panel (BMP)
- Hepatic Panel
- Lactate Dehydrogenase (LDH)
- Complete Blood Count (CBC)
- Imaging
- Plain Radiographs
- Numerous non-specific findings
- CXR may show pleural effusions, atelectasis or ARDS
- AXR may show an ileus, gallstones, calcified areas of pancreas
- Ultrasound
- Suboptimal imaging modality to diagnose pancreatitis but useful in establishing the presence or absence of a biliary cause
- US superior to CT for finding gallstones and common bile duct dilation (Harvey 1999, Reitz 2011)
- Obtain US as soon as possible
- One study found that US changed management in 55% (6/11) cases (Harvey 1999)
- Converts a medically managed disease to a surgically/interventionally managed one
- High suspicion for biliary disease with negative US should prompt Magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangio-pancreatography (ERCP)
- Computed Tomography
- Should not be obtained in all patients with pancreatitis during ED evaluation
- Useful in evaluation of other causes of abdominal pain and for the presence of complications (pseudocyst, abscess, hemorrhagic pancreatitis)
- Which ED pancreatitis patients should get an immediate CT
- Diagnosis of pancreatitis is uncertain
- Presence of severe pancreatitis
- Hemodynamic instability
- Organ failure (Hypotension, ARDS, GI bleed, AKI)
- Ranson score > 3, BISAP > 3 or APACHE > 8
- Concern for early complications
- Plain Radiographs
Management
- Supportive Care
- Intravenous fluids
- Pancreatitis causes 3rd spacing of fluid from the vasculature mainly via increased capillary permeability
- Traditional recommendations for large volume crystalloids (250-500 cc/hr X 12-24 hours) appears flawed (Farkas 2014)
- More conservative resuscitation approaches recommend 2 – 4L of balanced solution over 24 hours
- Give IV fluid boluses as needed for hypotension and volume depletion
- Consider early administration of vasoactive substances if necessary to support blood pressure
- Antiemetics
- Analgesia
- Pain often refractory to traditional analgesics and patients are likely to require opiates
- If patient tolerating oral intake, oral administration of analgesia is appropriate
- Intravenous fluids
- Oral Intake
- Traditional approach discouraged any oral intake and recommended nasogastric tube (NGT) placement
- Recent evidence supports early enteral nutrition (Kahl 2003)
- Recommendations
- If patient tolerates oral intake, start immediately
- If patient does not tolerate oral intake and has continuous emesis, NGT may be useful along with parenteral nutrition
- Antibiotics
- There is no evidence for the use of prophylactic antibiotics in pancreatitis (Tenner 2013)
- Necrotizing pancreatitis without signs of infection does not benefit from antibiotics (Isenmann 2004, Dellinger 2007)
- Antibiotics should be administered to patients with infectious complications from pancreatitis or infectious cause of their pancreatitis (i.e. cholangitis from gallstones)
- Evaluation for Complications
- Pancreatitis is a common cause of alcohol withdrawal. Carefully evaluate patient for signs of withdrawal if they have a history of alcohol use (tongue , tachycardia, hypertension, anxiety etc)
- Cholangitis
- Broad spectrum antibiotics
- Surgical and interventional radiology consultation for drainage
- ARDS
- Gallstone Pancreatitis
- All patients with pancreatitis should have an assessment for biliary pathology
- Presence of gallstones should be treated as gallstone pancreatitis until proven otherwise
- Look for concomitant cholangitis (fever, SIRS, lab abnormalities)
- Consultation
- Consult surgery for possible surgical intervention
- Consult gastroenterology for possible ERCP if biliary obstruction suspected (elevated bilirubin > 5.0 mg/dl) (Tenner 2013)
- Hypertriglyceridemic pancreatitis
- Addition of gemfibrozil 600 mg (lipid lowering medication)
- Plasmapheresis (plasma exchange)
- Allows for removal of triglycerides from circulation
- Requires hemodialysis catheter placement
- Insulin therapy
- Reduces triglyceride levels by reducing synthesis and accelerating metabolism
- Dose: 0.25 units/kg/hr (along with a dextrose infusion)
- Plasmapheresis vs. Insulin therapy
- Studies comparing plasmapheresis to insulin therapy are limited (Farkas 2017)
- Plasmapheresis is invasive, more expensive, requires anticoagulation, and requires hematology thus making performance more difficult
- Consider insulin therapy in conjunction with your ICU team
Disposition
- Admission to Hospital
- Any patient with signs or symptoms of severe pancreatitis should be placed in a high-monitored area (ICU) as decompensation is common
- Patients with inability to tolerate oral intake
- Patients with pain refractory to oral medications
- Patients without reliable follow up (i.e. those without insurance, homeless patients, chronic alcoholics etc)
- Patients with gallstone pancreatitis
- Patients who are stable, tolerating oral intake, have their pain controlled with oral medications and are able to follow up or return to the ED may be discharged home on a low fat diet
Take Home Points
- Pancreatitis is diagnosed by a combination of clinical features (epigastric pain with radiation to back, nausea/vomiting etc) and diagnostic tests (lipase 3x normal, CT scan)
- A RUQ US should be performed looking for gallstones as this finding significantly alters management
- The focus of management is on supportive care. IV fluids, while central to therapy, should be given judiciously and titrated to end organ perfusion
- Patients will mild pancreatitis who are tolerating oral intake and can reliably follow up, can be discharged home
Read More
Hemphill RR, Santen SA: Disorders of the Pancreas; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 91: p 1205-1226
PulmCrit: The Myth of Large-Volume Resuscitation in Acute Pancreatitis
PulmCrit: Hypertriglyceridemic Pancreatitis: Can We Defuse the Bomb?
References
Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology Am J Gastroenterol. 2006;101(10): 2379-400. PMID: 17032204
Matsull WR et al. Biochemical markers of acute pancreatitis. J Clin Pathol 2006; 59:340. PMID: 16567468
Harvey RT, Niller WT. Acute biliary disease: Initial CT and follow-up US vs. initial US and follow-up CT. Radiology 1999; 213(3): 831-6. PMID: 10580962
Reitz S et al. Biliary, pancreatic, and hepatic imaging for the general surgeon. Surg Clin North Am 2011; 91(1): 59-92. PMID: 21184901
Tenner S et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 2013; 108(9): 1400-15. PMID: 23896955
Wu BU et al. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut 2008; 57: 1698-1703. PMID: 18519429
Papachristou GI et al. Comparison of BISAP, Ranson’s, APACHE-II, and CTSI scores in predicting organ failure, complications and mortality in acute pancreatitis. Am J Gastroenterol 2010; 105: 435-51. PMID: 19861954
Kahl S et al. Acute pancreatitis: Treatment strategies. Dig Dis 2003; 21:30. PMID: 12837998
Isenmann R et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: A placebo-controlled, double-blind trial. Gastroenterology 2004; 126(4): 997-1004. PMID: 15057739
Dellinger EP et al. Early antibiotic treatment for severe acute necrotizing pancreatitis. Ann Surg 2007; 245(5): 674-683. PMID: 17457158
