Definition: Acute inflammation of the gallbladder
Variant Forms
- Acalculous cholecystitis (10% of cases): Inflammation of the gallbladder in the absence of gallstones or cystic duct obstruction that is more common in older patients and after non-biliary tract surgery
- Emphysematous cholecystitis (1% of cases): Inflammation of the gallbladder along with the presence of gas in the gallbladder wall. It is more commonly seen in diabetic patients.
Pathophysiology
- Cystic duct obstruction is the proximate cause of cholecystitis
- Obstruction leads to gallbladder distension
- An inflammatory reaction occurs due to either mucosal ischemia from increased hydrostatic pressure or cytotoxic effects of bile degradation
- Causes
- Gallstones (95% of patients with cholecystitis)
- Fibrosis
- Parasitic infection
- Tumor
- Lymphadenopathy
Differential Diagnosis
- Biliary colic
- Choledocholithiasis
- Mirizzi syndrome (gallstone impaction in the cystic duct or gallbladder neck causing common bile duct (CBD) or common hepatic duct compression)
- Acute Hepatitis
- Hepatic abscess
- Right lower lobe pneumonia
- Cholangitis
- Pancreatitis
- Pyelonephritis
Presentation
- History
- Right upper quadrant (RUQ) pain
- History of similar, self-limited pain (biliary colic)
- Nausea/Vomiting
- Radiation of pain to the tip of the right scapula (referred pain)
- Physical Examination
- RUQ/epigastric tenderness to palpation
- Variable presence of rebound/guarding
- Tenderness with an inspiratory pause during palpation of the RUQ during a deep breath (Murphy’s sign)
- Best test for diagnosis of acute cholecystitis (Jain 2017)
- (+) LR = 15.64
- (-) LR = 0.40
- Fever is poorly sensitive (35%) and nonspecific (80%) (Towbridge 2003)
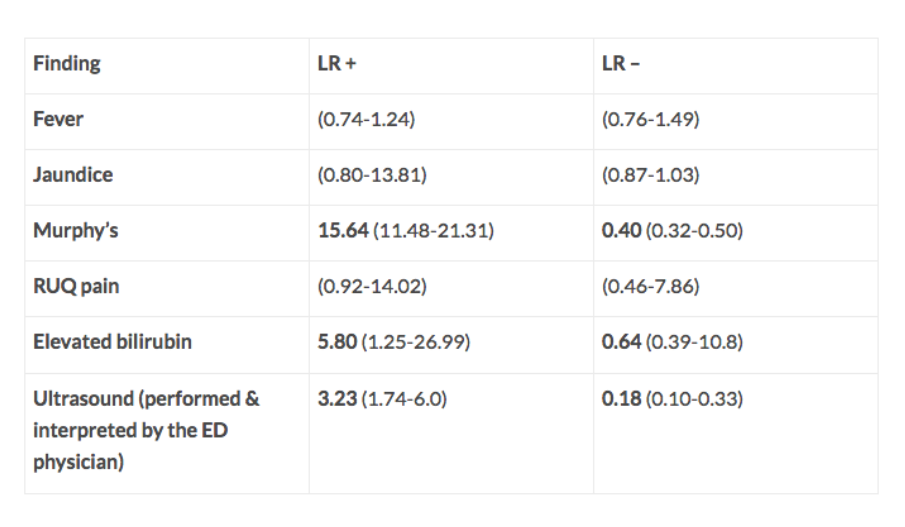
Diagnostic Test Performance in Acute Cholecystitis (The Resus Room)
Diagnostics
- Laboratory Tests
- Overall, laboratory tests are insensitive and non-specific. They can neither rule in nor out the disease
- WBC count: Elevation with a left shift is common but may be absent in up to 40% of patients (Gruber 1996)
- AST/ALT: May be mildly elevated but are poorly sensitive (38%) and specific (62%)
- Total/Direct Bilirubin: If elevated, it raises suspicion for choledocholithiasis, cholangitis, or Mirizzi syndrome

Acute Cholecystitis (Long Axis US) Case courtesy of Dr Hani Al Salam, Radiopaedia.org. From the case rID: 16067
- Ultrasound (US)
- Common findings
- Presence of gallstones (absence of stones has a high negative predictive value for cholecystitis)
- Thickened gallbladder wall (> 3 mm)
- Pericholecystic fluid
- Maximal tenderness elicited over the visualized gallbladder by the US probe (Sonographic Murphy’s sign)
- Test characteristics
- Impacted gallstones (in the neck or cystic duct) + sonographic Murphy’s sign have a positive predictive value of 70% (Rosen 2001) to 92% (Ralls 1985)
- Overall sensitivity 88%, specificity 80% (Shea 1994)
- Common findings
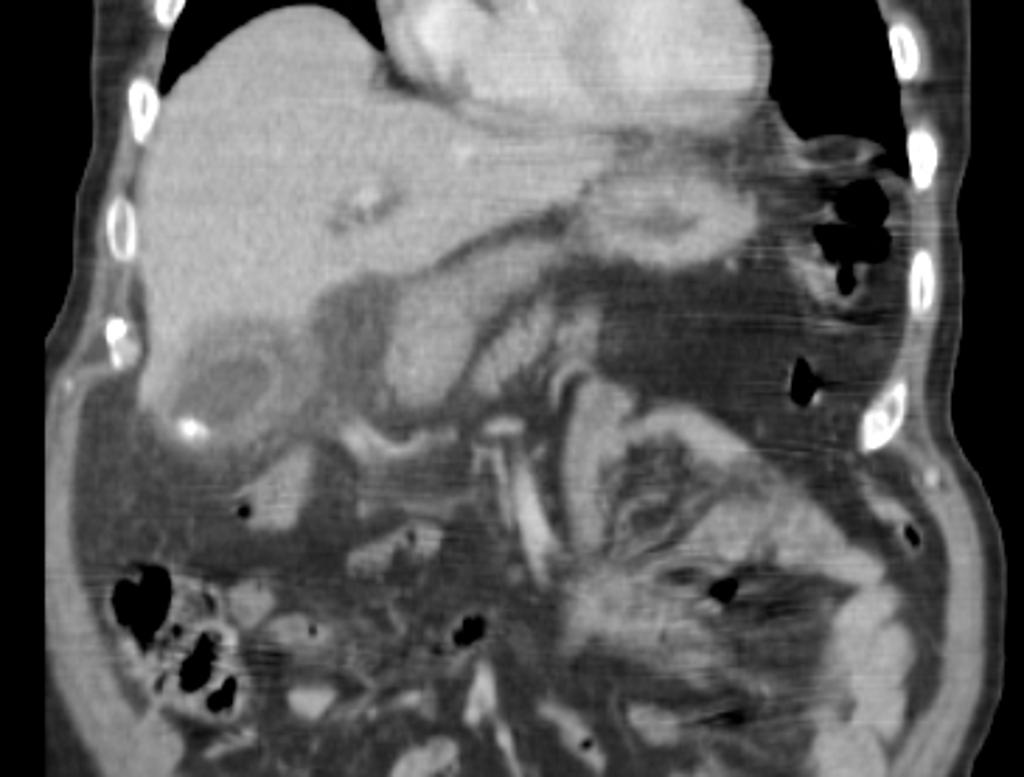
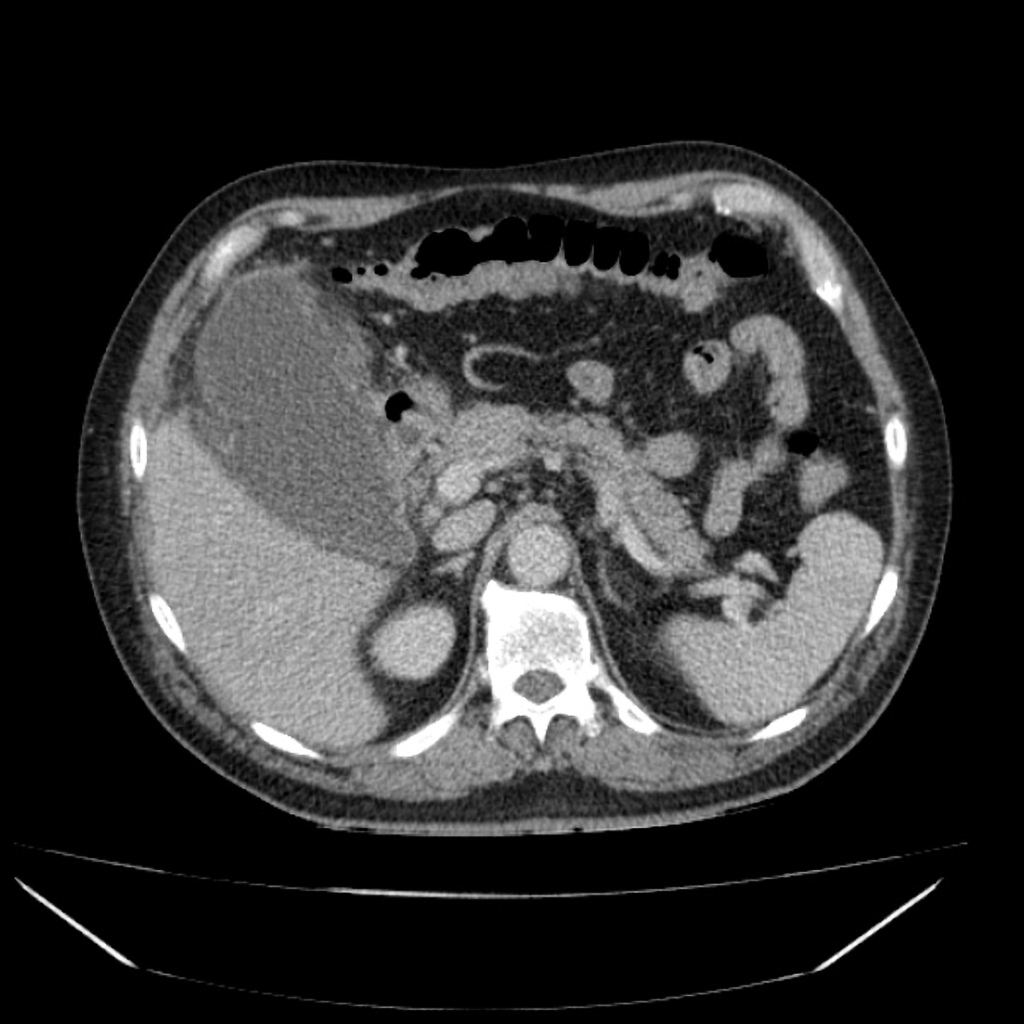
Acute Cholecystitis (CT Scan Sagittal Images) Case courtesy of Dr Hani Al Salam, Radiopaedia.org. From the case rID: 16067
- CT
- Higher accuracy than US for defining complications related to cholecystitis (gangrene, emphysematous cholecystitis)
- Common findings (Fidler 1996)
- Thickened gallbladder wall (> 3 mm)
- Increased attenuation of the gallbladder bile
- Subserosal edema
- Nuclear Scintigraphy with Technetium-99m-labeled hepatobiliary iminodiacetic acid (HIDA)
- Gold standard for diagnosis with high sensitivity and specificity
- Positive study: Failure of HIDA to outline the gallbladder within 1 hour of administration
Acute Cholecystitis Images

Acute Cholecystitis (US Short Axis) Case courtesy of Dr Hani Al Salam, Radiopaedia.org. From the case rID: 16067

Distended gall bladder shows edematous wall, calculi and sludge with pericholecystic collection Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 20542

Gangrenous Cholecystitis Case courtesy of Dr David Cuete, Radiopaedia.org. From the case rID: 38882
Management:
- Basic Supportive Care
- IV crystalloids: optimize volume status
- Check + replete electrolytes as needed (may be significant losses from vomiting)
- Antiemetics
- Pain control
- Antibiotics
- The role of bacterial infection in the pathogenesis of cholecystitis is not completely understood
- If the patient exhibits signs of sepsis, administer broad-spectrum antibiotics covering gram negative/positive pathogens as well as anaerobes
- Vancomycin AND an advanced generation penicillin (i.e. piperacillin/tazobactam)
- Vancomycin AND a 3rd/4th generation cephalosporin (i.e. cefepime) AND metronidazole
Gangrenous Cholecystitis Case courtesy of Dr David Cuete, Radiopaedia.org. From the case rID: 38882
- In the absence of sepsis, consider administration of a 2nd/3rd generation cephalosporin
- Emphysematous cholecystitis
- Likely caused by invasion of gas-producing pathogens (E. coli, Klebsiella, Clostridium perfringens)
- Advanced generation penicillin (i.e. piperacillin/tazobactam) +/- metronidazole
- Surgical Consultation for cholecystectomy
- Complications
- Gangrene leading to necrosis and perforation
- Emphysematous cholecystitis
- Pericholecystic abscess
- Sepsis
Disposition:
- Admission for IV antibiotics and pain control
- Cholecystectomy is typically performed during the initial hospitalization as early cholecystectomy appears to have improved outcomes
- Patients with gangrene or perforation may undergo immediate cholecystectomy or cholecystostomy and drainage
Take Home Points
- Acute cholecystitis is an inflammation of the gallbladder that is most readily diagnosed by US
- Treatment focuses on fluid resuscitation when indicated, supportive care, antibiotics and surgical consultation for cholecystectomy
- Although uncommon, be aware that patients can develop gangrene, necrosis and perforation as well as frank sepsis and require aggressive resuscitation
The Resus Room: Acute Cholecystitis
Oyama LC: Disorders of the liver and biliary tract, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 90: p 1186-1205.
Leschka S et al. Chapter 5.1: Acute abdominal pain: diagnostic strategies In: Schwartz DT: Emergency Radiology: Case Studies. New York, NY: McGraw-Hill, 2008.
Menu Y, Vuillerme MP. Chapter 5.5: Non-traumatic Abdominal Emergencies: Imaging and Intervention in Acute Biliary Conditions In: Schwartz DT: Emergency Radiology: Case Studies. New York, NY: McGraw-Hill, 2008.
References
Fidler J et al. CT evaluation of acute cholecystitis: findings and usefulness in diagnosis. Am J Roentgenol. 1996; 166:1085–1088. PMID: 8615248
Gruber PJ et al. Presence of fever and leukocytosis in acute cholecystitis. Ann Emerg Med 1996; 28: 273. PMID: 8780469
Jain A et al. History, physical examination, laboratory testing and emergency department ultrasonography for the diagnosis of acute cholecystitis. Acad Emerg Med 2017; 24(3):281-297. PMID: 27862628
Ralls PW et al. Real-time sonography in suspected acute cholecystitis.Prospective evaluation of primary and secondary signs. Radiology 1985; 155:767–771. PMID: 3890007
Rosen CL et al. Ultrasonography by emergency physicians in patients with suspected cholecystitis. Am J Emerg Med. 2001; 19(1):32-36. PMID: 11146014
Shea JA, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med. 1994; 154(22):2273. PMID: 7979854
Towbridge RL et al. Does this patient have acute cholecystitis? JAMA 2003; 289(1);80-6. PMID: 12503981
