 Background:
Background:
- Lower pain back is one of the most common complaints in the Emergency Department (ED), comprising 2.6 million ED visits in the US in 2006. (Friedman 2010)
- The prevalence of chronic lower back pain is about 23%, and the lifetime prevalence of lower back pain is estimated to be around 60-70%. (Balague 2012)
- We will explore the differential diagnosis of non-traumatic lower back pain, with an emphasis on emergent etiologies.
Basic approach:
The majority of ED low back pain presentations represent benign processes (i.e. musculoskeletal). These patients should be advised to resume normal activity, as prompt return to normal activity provides better outcomes than bed rest. Despite the predominance of benign causes, some patients will present with more serious pathologies that can cause neurologic disability, and non-spine causes of back pain (i.e. abdominal or retroperitoneal etiologies). A thorough history and physical is paramount in discriminating benign versus serious versus non-spine causes of lower back pain.
Patients with nonspecific back pain for less than 6 weeks with no red flags do not need imaging and can be discharged with analgesics and outpatient follow-up. Similarly, patients presenting with radiculopathy at L4-L5 or L5-S1 most often have disc herniation and often do not require emergent imaging either (Lin 2014). Patients with radiculopathy presenting with red flags suggesting serious pathology should receive emergent imaging. Note that plain film is neither sensitive nor specific for the workup of lower back pain. Additionally, the use of opiates is discouraged, and alternative modalities of pain treatment should be pursued first.

Red Flags:
- New onset of back pain at extremes of age (< 20 years or > 50 years)
- History of cancer
- Constant, non-mechanical back pain, or pain worse when lying down
- Presence of neurologic symptoms including weakness and numbness
- Bilateral symptoms
- Immunosuppression (i.e. HIV/AIDS, corticosteroids, immunomodulating drugs)
- IVDU
- Change in bowel/bladder function (increased or decreased function) or erectile dysfunction
- Fever or night sweats
- Anticoagulant use
Patients with red flags along with their back pain should be considered for imaging (MRI) in the ED.
Physical Exam:
- Focal neurologic signs and symptoms are specific but not sensitive (i.e. if present, they suggest serious pathology but their absence does not rule out disease) (Edlow 2015)
- Concerning physical exam findings
- Motor – weakness in legs or arms
- Sensory – saddle anesthesia
- Reflexes – diminished or abnormal reflexes including positive Babinski sign
- Sphincter dysfunction – decreased rectal tone or post-void residual >100 ml (Edlow 2015)
- Midline tenderness to palpation or percussion
Emergent Differential Causes of Low Back Pain
- Non-Spine Related Causes
- Vascular
- Abdominal aortic aneurysm (AAA)
- Aortic dissection
- Renal artery dissection or thrombosis
- Pyelonephritis
- Retroperitoneal hemorrhage
- GI Causes (i.e. pancreatitis, peptic ulcer, cholecystitis)
- Vascular
-
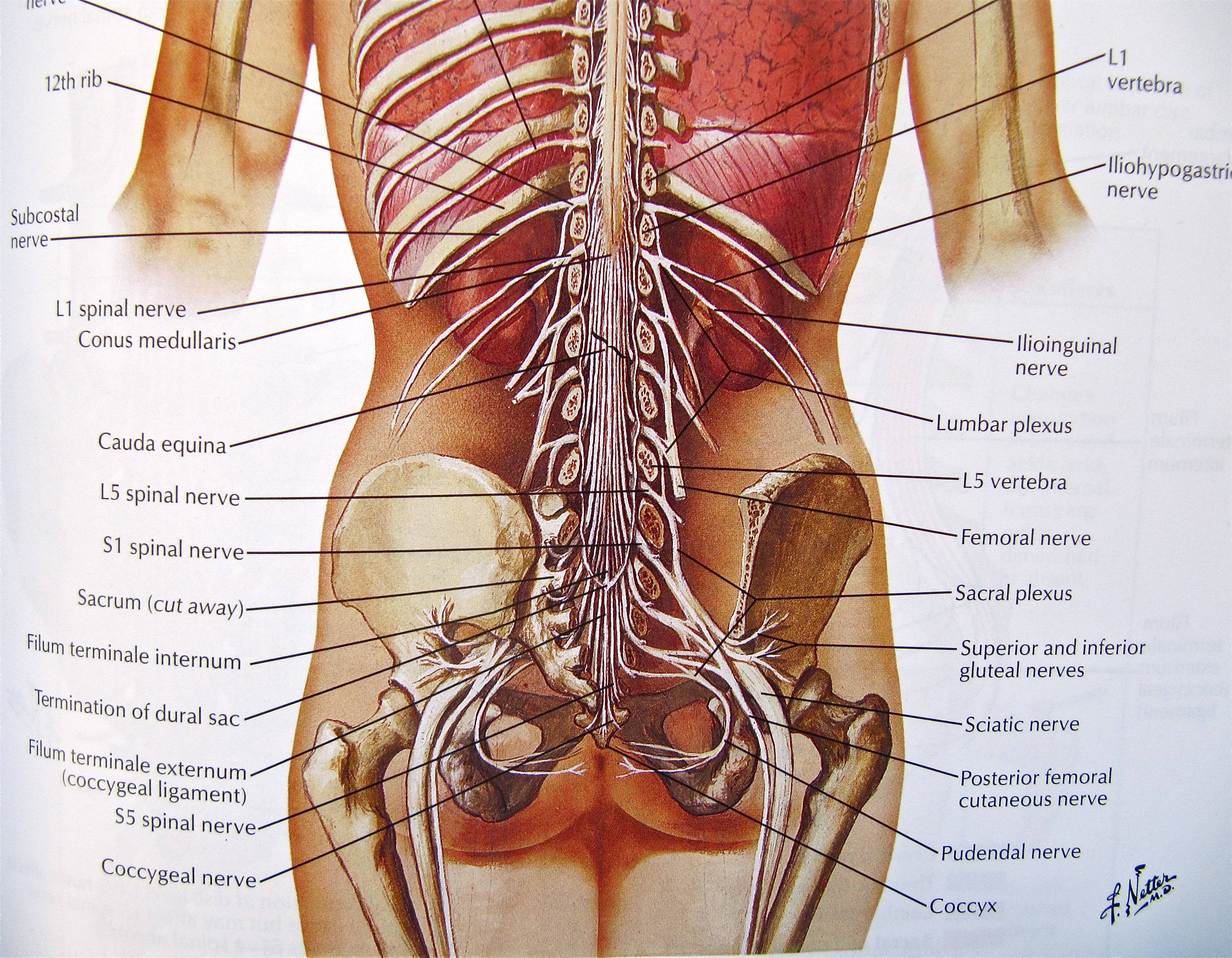
Spine Anatomy (Netter)
Oncologic
- Epidural metastatic disease
- Intradural metastatic disease
- Intramedullary tumor
- Infectious
- Spinal epidural abscess
- Vertebral osteomyelitis
- Infectious discitis
- Spinal epidural hematoma
- Cauda equina syndrome (from disc herniation)
Note: low back pain in the pediatric population is a separate topic with a different differential diagnosis to consider.
Take Home Points:
- The vast majority of non-traumatic low back pain is benign (mechanical/musculoskeletal in origin)
- Ask about red flags! These help identify patients with more serious pathology
- “Back pain” does not always mean the pathological process is occurring in the back. Consider abdominal causes of back pain as well
- Plain films are unhelpful – they are neither sensitive nor specific for discriminating etiology of lower back pain
- If you are concerned for a dangerous pathology as the cause of back pain, obtain an MRI as both plain films and CT will commonly miss serious pathology
Read more
EM: RAP: C3 – Back Pain
St. Emlyn’s: Back to Basics – Back Pain in the ED
Radiopaedia: Cauda Equina Syndrome
Emergency Medicine Cases: Best Case Ever 11: Cauda Equina Syndrome
emDocs: Cauda Equina Syndrome
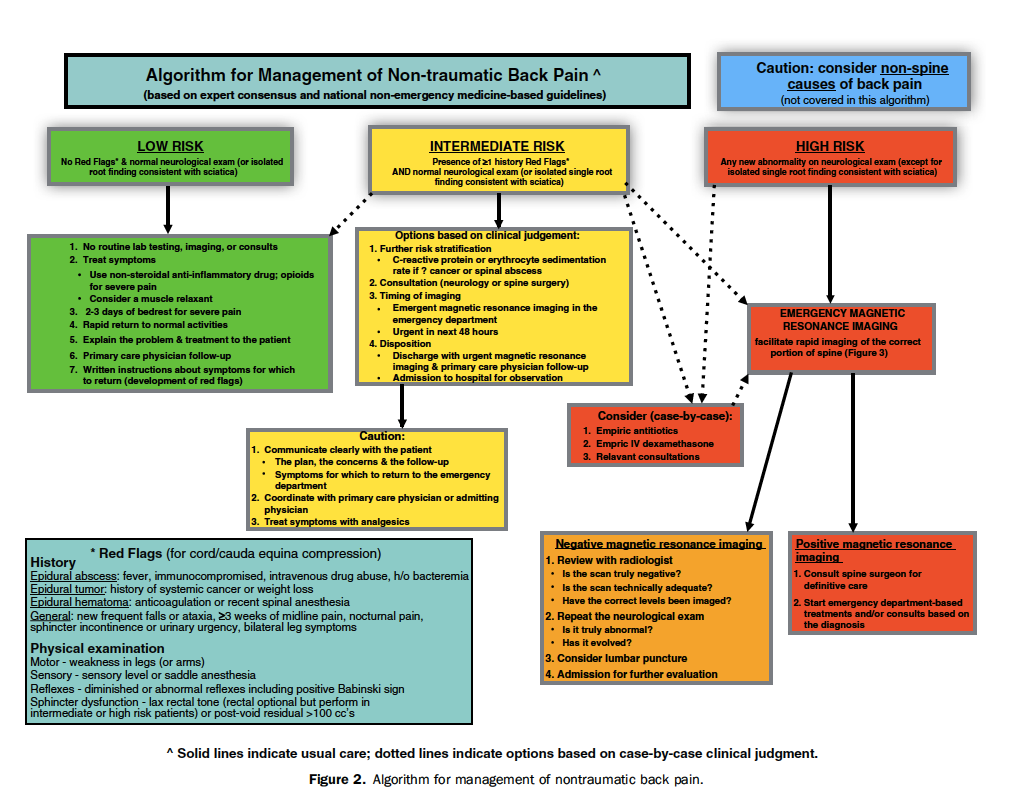
Non-traumatic Back Pain Algorithm (Edlow 2015)
References:
Friedman, BW et al. Diagnostic Testing and Treatment of Low Back Pain in US Emergency Departments. A National Perspective. Spine 2010; 35 (24) E1406–11. PMID: 21030902
Balague, F et al. Non-specific low back pain. The Lancet 2011; 379 (9814): 482-491. PMID: 21982256
Lin, Michelle, and Jeremiah D. Schuur. A High-Value Diagnostic Approach to Low-Back Pain. ACEP Now 2014; 33 (3).
Edlow, JA. Managing Nontraumatic Acute Back Pain. Annals of Emergency Medicine 2015; 66 (2): 148-53. PMID: 25578887
