 Definition
Definition
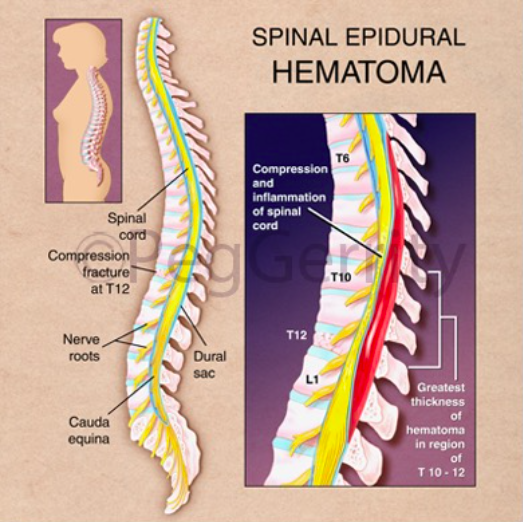
Spinal epidural hematoma is a collection of blood in the potential space between the dura and the bone, along the spinal canal. Significant bleeding can lead to spinal cord damage, causing neurological injury and deficit. This is a neurosurgical emergency.
Epidemiology
- Overall incidence approximately 1 per 1,000,000 people annually (Perron 2013)
- The source of bleeding is usually venous (Aminoff 2016)
- Traumatic spinal epidural hematoma
- Frequency unclear
- Typically will have concomitant spine fracture
- Spontaneous spinal epidural hematoma
- Associated with anticoagulation, coagulopathies, thrombocytopenia, neoplasms, or vascular malformations
- Spinal epidural hematomas, however, may also occur rarely in patients with no history of coagulopathy and use of anticoagulation (Aminoff 2016)
- Iatrogenic spinal epidural hematoma
- The risk of bleeding after procedures increases with anatomical factors such as vertebral abnormalities, multiple attempts at needle placement, and use of anticoagulation or antiplatelet therapy (Yi 2006)
Clinical Presentation
- Symptoms
- Patients typically complain of sudden onset of severe back pain, or radicular pain, depending on the location of the bleeding
- Pain may be exacerbated by percussion of the spine or by movements that increase intraspinal pressure, such as coughing or sneezing (Perron 2013)
- Neurological symptoms may not develop until hours to days after the onset of back pain, making this a difficult early diagnosis to make
- Signs
- There may be tenderness to palpation of the spine
- Motor and sensory deficits depend on the level and size of the hematoma
- Clinical presentation can range from focal weakness to paraplegia or quadraplegia, and from paresthesias to complete loss of sensation below a certain level (Myers 2015)
Diagnostic Modalities
- Hematomas may extend over many segments. The total spine should always be imaged, even in patients with well localized clinical signs (Post 1982)
-

T1 + T2 MRI Imaging
Magnetic resonance imaging (MRI)
- Gold standard imaging modality
- Superior to CT as it helps define the extent, volume, and precise location of the hematoma
- Should be performed with and without contrast
- Findings:
- In the first 24 hours, the hematoma is usually isointense or slightly hyperintense on T1-weighted imaged and hyperintense on T2-weighted images (Sklar 1999)
- After 24 hours, the hematoma becomes mostly hyperintense on both T1- and T2-weighted images
-
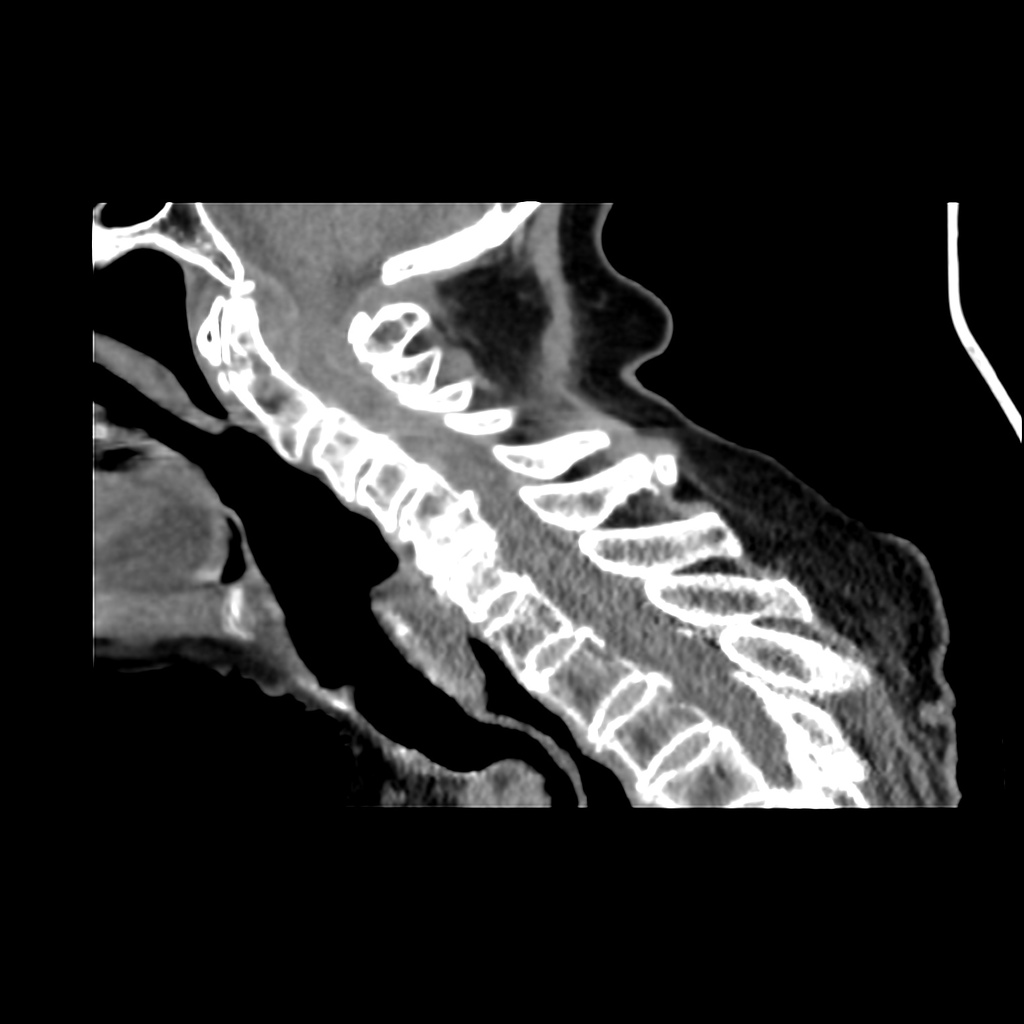
Non-Contrast CT with Dens Fracture + Epidural Hematoma (Case courtesy of Dr Andrew Dixon, Radiopaedia.org. From the case rID: 31764)
Computed Tomography (CT)
- Non-contrast CT or CT myelography preferred imaging if MRI not available or if the patient cannot get an MRI (Zilkha 1983)
- Findings:
- The hematoma is usually visualized as a biconvex-shaped hyperdense lesion within the spinal canal, lying adjacent to the vertebral body (Post 1982)
- The lesion will be sharply demarcated and is separated from the less dense spinal canal
Management
- Immediate consultation with neurosurgery
- Spinal epidural hematoma is a neurosurgical emergency that requires rapid surgical decompression (Myers 2015)
- Post-operative neurologic function is related to preoperative neurologic function and the time interval to decompression
- Delays in surgical management can lead to permanent neurological sequelae (Yi 2006)
- Full recovery after 72 hours of symptoms is rare (Perron 2013)
- Patients with mild symptoms may be managed conservatively after consultation with a neurosurgeon. Patients managed non-operatively may receive dexamethasone.
- There have been rare cases of spontaneous recovery of spinal epidural hematomas.
Take Home Points
- Consider the diagnosis of spinal epidural hematoma in all patients with acute onset of back pain who have recently undergone spinal procedures, have coagulopathies or are on anticoagulation
- MRI is currently the best diagnostic modality for evaluating suspected spinal epidural hematoma. A CT can be obtained if MRI is not readily available but a negative CT in a high-risk patient should be followed with an MRI.
- Time to diagnosis and time to surgical decompression are key as delays can lead to permanent neurological sequelae
Read More
Radiopaedia: Spinal Epidural Haemtoma
emDocs: Spinal Epidural Hematoma
Perron AD and Huff JS. Spinal Cord Disorders. In: Marx JA et al. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 8th ed. Philadelphia: Saunders, 2013. 1419-1427. Link
References
Aminoff, MJ. Lumbar Puncture: Technique, Indications, Contraindications, and Complications in Adults. Topic 4832, Version 14.0. In: Aminoff, MJ (Section Ed.) UpToDate. Link
Myers M et al. Extensive Subarachnoid and Epidural Hematoma After Lumbar Puncture. Am J Emerg Med. 2015:33(4):603.e3-4. PMID: 25445864
Post MJ et al. CT Diagnosis of Spinal Epidural Hematoma. Am J Neuroradiol. 1982:3:190-192. PMID: 6803553
Yi S et al. Postoperative Spinal Epidural Hematoma: Risk Factor and Clinical Outcome. Yonsei Med J. 2006:47(3):326-332. PMID: 16807981
Sklar EM et al. MRI of Acute Spinal Epidural Hematoma. J Comput Assist Tomogr. 1999:23(2):238-43. PMID: 10096331
Zilkha A et al. Computed Tomography of Spinal Epidural Hematoma. Am J Neuroradiol. 1983:4:1073-76. PMID: 6414267