Background
In 2016 the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), redefined sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection. This group postulated that sepsis can be identified through an increase in Sequential Organ Failure Assessment (SOFA) score of at least 2 points. The quick SOFA (qSOFA) score is a simplified tool that includes respiratory rate >21 breaths/min, altered mental status, or systolic arterial blood pressure <100 mm Hg. Retrospectively derived, it has been considered a possible replacement for the Systemic Inflammatory Response Syndrome (SIRS) criteria and as a surrogate for the SOFA score in identifying sepsis. To date, there have not been any prospective studies evaluating the performance of qSOFA in comparison to either SOFA or SIRS in the Emergency Department (ED).
Clinical Question
Does the qSOFA score more accurately predict in-hospital mortality than the SIRS criteria or severe sepsis criteria among ED patients with suspected infection?
Population
All consecutive adult patients with clinical suspicion for infection who presented to one of 30 EDs in Europe over a four week period.
Intervention
Data was prospectively collected to assess the qSOFA and SIRS scores and severe sepsis criteria (SIRS + lactate) in the ED based on the patients worst level.
Outcomes
Primary: In-hospital mortality within 28 days of initial encounter.
Secondary: Admission to ICU, length of stay in ICU >72 hours, and composite of death or ICU stay of more than 72 hours.
Design
International, multicenter prospective cohort study in which patients deemed to have an infection by the treating emergency physician were followed throughout their hospital course. Two experts determined in each case if the initial ED presentation was due to an infection.
Excluded
Patients who were deemed to not have an infection by two experts reviewing each case, as well as patients who refused to participate, pregnant women, prisoners, low acuity patients, patients in custody.
Primary Results
- 1088 patients assessed for eligibility and 879 patients enrolled
- Median patient age = 67 years
- 43% of patients had a respiratory tract infection
- Primary outcome (in hospital mortality):
- Overall: 8%
- qSOFA Performance
- qSOFA ≥2: 24% mortality
- qSOFA <2: 3% mortality
- Severe sepsis performance
- SIRS ≥2 and lactate >2: 20% mortality
- SIRS Performance
- SIRS ≥ 2: 11% mortality
- SIRS <2: 2.2% mortality
Critical Results
| qSOFA | SIRS | Severe Sepsis | SOFA | |
| Sensitivity (%) | 70 | 93 | 47 | 73 |
| Specificity (%) | 79 | 27 | 82 | 70 |
| (+) LR | 3.40 | 1.29 | 2.70 | 2.40 |
| (-) LR | 0.37 | 0.25 | 0.64 | 0.39 |
| AUROC (95% CI) | 0.80 (0.74-0.85) | 0.65 (0.59-0.70) | 0.65 (0.59-0.70) | 0.77 (0.71-0.82) |
| Hazard Ratio (95% CI) | 6.2 (3.8 – 10.3) | 3.5 (2.2-5.5) |
- qSOFA outperformed SIRS, severe sepsis and SOFA in terms of the receiver operating curve (AUROC)
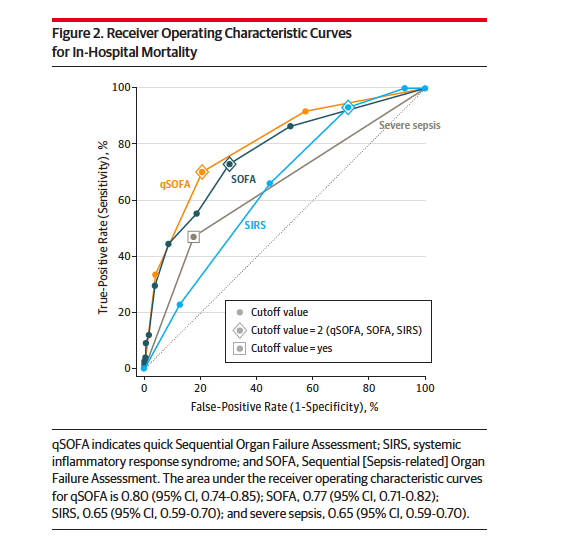
ROC Curve for In-Hospital Mortality
Strengths
- First multicenter prospective cohort study comparing the Sepsis-3 criteria SIRS, severe sepsis and SOFA in terms of predicting mortality
- Addresses two major issues with the Sepsis-3 task force work: absence of prospective validation and lack of ED involvement
Limitations
- Although the study was international, 27 out of 30 centers that enrolled patients were in a single country
- Used the highest qSOFA score while in the ED thereby reducing its role as an initial screening tool
- Discharged patients were not followed or incorporated in the analysis
- Experts who identified patients in sepsis had incorporation bias as the definition for sepsis is actually used to make the final diagnosis
- Though qSOFA performed better than it’s counterparts, sensitivity was just 70%; an unacceptably low number for a screening test
Author's Conclusions
“Among patients presenting to the emergency department with suspected infection, the use of qSOFA resulted in greater prognostic accuracy for in-hospital mortality than did either SIRS or severe sepsis. These findings provide support for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) criteria in the emergency department setting.”
Our Conclusions
In this prospective validation study, qSOFA performed better than both SIRS and severe sepsis in predicting in-hospital mortality from sepsis. However, with a sensitivity of just 70%, use of qSOFA alone would lead to an unacceptable miss rate. These results underscore the fact that sepsis is a complicated process and identification is unlikely to be simplified down to 3-4 criteria.
Potential Impact To Current Practice
The use of qSOFA alone should not replace the use of good clinical judgment for determining patients with sepsis in the ED. However, qSOFA > 2 is an excellent marker of severity of illness and should be used as such.
Bottom Line
Patients who present to the ED with an infection and have 2 or more qSOFA criteria while in the ED have a high inpatient mortality rate, yet qSOFA alone cannot be used as a rule out or used as a screening tool for sepsis due to the poor sensitivity.
Read More
EM Nerd: The Case of the Cryptic Truth
EMCrit: Practical Evidence Podcast 015
PulmCrit: Six Myths Promoted by the Surviving Sepsis Guidelines