Definition: bleeding from the gastrointestinal tract that is proximal to the ligament of Treitz
 Presentation
Presentation
- Hematemesis
- Coffee-ground emesis
- Melena
- Hematochezia (14% cases from UGIB)
- Anemia
- Hypovolemic shock
Important Historical Features
- History of GI bleeds (rebleed at same site is common)
- Peptic ulcer disease most common cause (Overton 2011)
- Esophageal or Gastric Variceal Bleed
- Heavy alcohol use (consider diagnosis of esophageal/gastric variceal bleeding)
- Cirrhosis and known varices
- Aspirin or NSAID use: consider esophagitis/gastritis/duodenitis
- Extreme valsalva maneuvers: consider Mallory-Weiss Syndrome
- Aortic or GI tract surgeries: consider aortoenteric fistulas vs. post-surgical anastomotic ulcers
- GI neoplasms
Physical Examination:
- Review vital signs looking for hemodynamic compromise (tachycardia, hypotension, tachypnea)
- Look for evidence of shock: confusion, peripheral vasoconstriction
- Hematemesis
- Evidence of liver disease
- Jaundice, ascites, spider angiomas, caput medusae
- Increases risk of variceal bleeding
ED Management
- Initial Resuscitation
- Evaluate for evidence of hemodynamic instability
- Clinical signs most useful
- Hemoglobin inaccurate in acutely bleeding patient
- Obtain large bore IV access
- 18 gauge IV or larger at/above antecubital fossae
- Consider placement of introducer central line
- Replace blood loss with blood products
- Can start with crystalloid fluids if blood not immediately available
- Consider massive transfusion protocol as needed
- Airway
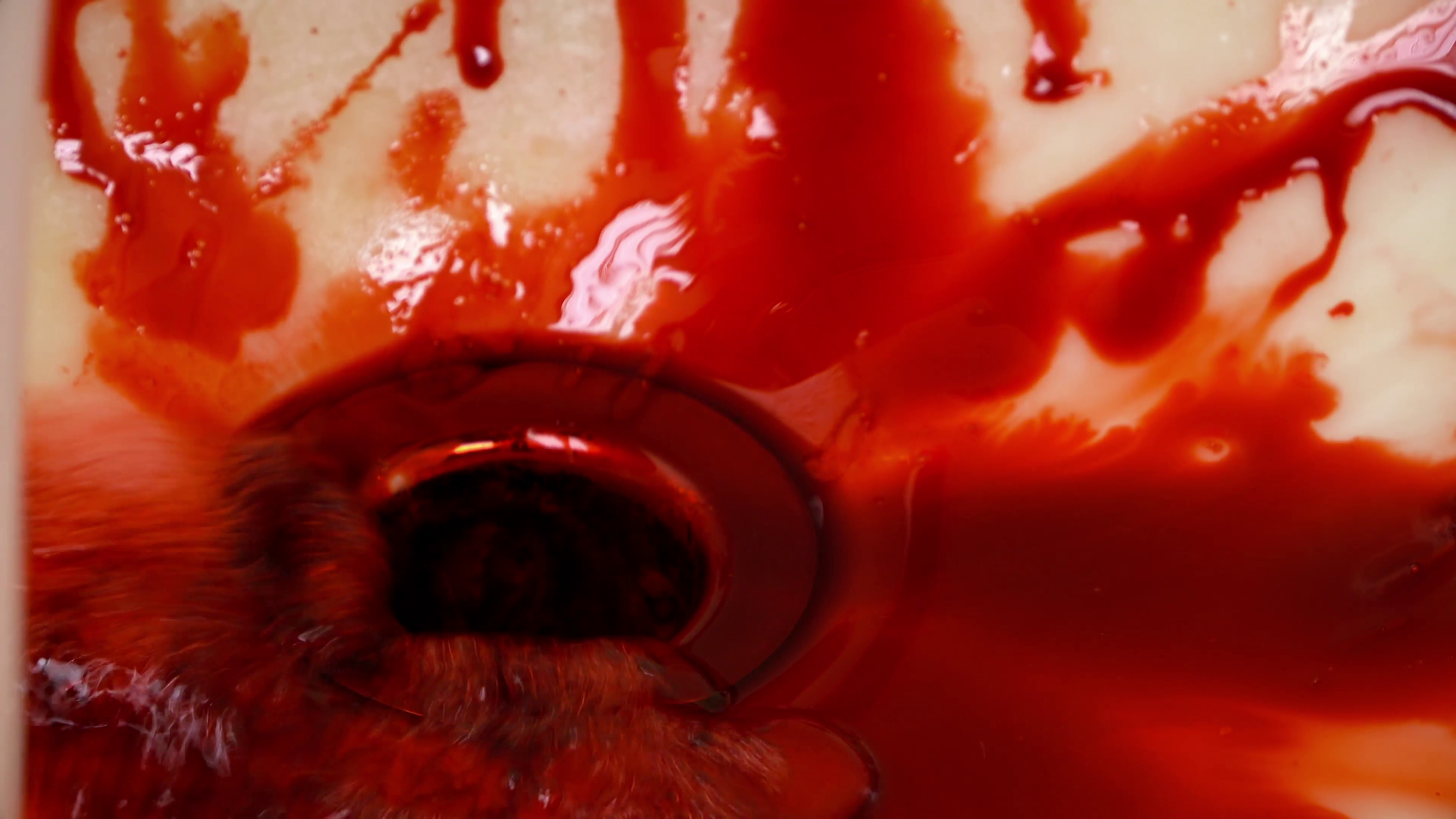
- Actively bleeding patients may require intubation to facilitate endoscopy or balloon tamponade
- Patients often confused at increased aspiration risk
- Intubation often complicated by blood airway and tenuous hemodynamics
- Airway Considerations
- Aggressively resuscitate prior to intubation as induction agents can cause worsening hemodynamics and apnea can cause worsening hypoxia
- Personal protection equipment including facemask, gown, gloves
- Pre-oxygenation
- Positioning: Head of bed >45 degrees to increase oxygenation and decrease vomiting risk
- Consider ketamine (1-2mg/kg IV) to facilitate cooperation with pre-oxygenation
- Avoid BiPAP or CPAP if actively vomiting or high-risk for vomiting
- RSI medication considerations
- Lower dose of induction agent if patient in shock
- Increase dose of paralytic if patient in shock (increased circulation time)
- Have push-dose (i.e. epinephrine) and infusion vasopressors (norepinephrine) available
- Redundant large bore suction to clear blood (see SALAD technique)
- Consider gastric emptying
- Nasogastric tube
- Metoclopramide 10-20 mg IV (delayed onset)
- Mentally prepare and low threshold for surgical airway
- Evaluate and consider marking landmarks
- Reverse coagulopathy + thrombocytopenia
- Reverse coagulopathy + thrombocytopenia
- FFP or PCCs for INR >1.6
- Platelet goal is >50,000 if actively bleeding
- Maintain normal body temperature to prevent worsening coagulopathy
- If HD stable, transfuse to Hb of 7 or higher depending of evidence of end-organ dysfunction; do not over transfuse (Villaneuva, 2013)
- Reverse coagulopathy + thrombocytopenia
- Evaluate for evidence of hemodynamic instability
- Specific considerations
- Peptic ulcer bleeding
- Call consultants early for definitive treatment
- Gastroenterology – endoscopy with epinephrine injection, sclerotherapy, or clipping
- General Surgery – surgical resection and vessel ligation
- Interventional Radiology – transarterial embolization
- Proton Pump Inhibitor (PPI)
- Omeprazole or esomeprazole 40 mg IV twice daily
- Use BID doses as no added utility in infusion (Sachar 2014)
- No effect mortality benefit but reduce stigmata of PUD during initial endoscopy
- Call consultants early for definitive treatment
- Variceal bleeding
- Call consultants early for definitive treatment
- Gastroenterology – endoscopy with banding/clipping
- Interventional Radiology – TIPS procedure (see below)
- Reduces portal systemic pressures shunting blood away from varices
- Effective but often results in hepatic encephalopathy
- General Surgery – surgical shunts, i.e. Warren distal splenorenal shunt
- Prophylactic antibiotics:
- 1g Ceftriazone or a fluoroquinolone (I.e. Cipro 400mg BID if cephalosporin allergy)
- Reduces bacterial infections, mortality, and hospitalization length (Chavez-Tapia, 2011)
- NNT = 4 for bacterial infections
- NNT = 22 for mortality
- Octreotide
- 50mcg IV bolus and then drip at 50mcg/hr
- Shunts blood away from varices by reducing splanic blood flow
- If intubated with persistent bleeding and no immediate definitive treatment available, can try ballon tamponade (see videos for placement of Blakemore and Minnesota tubes)
- Call consultants early for definitive treatment
- Peptic ulcer bleeding
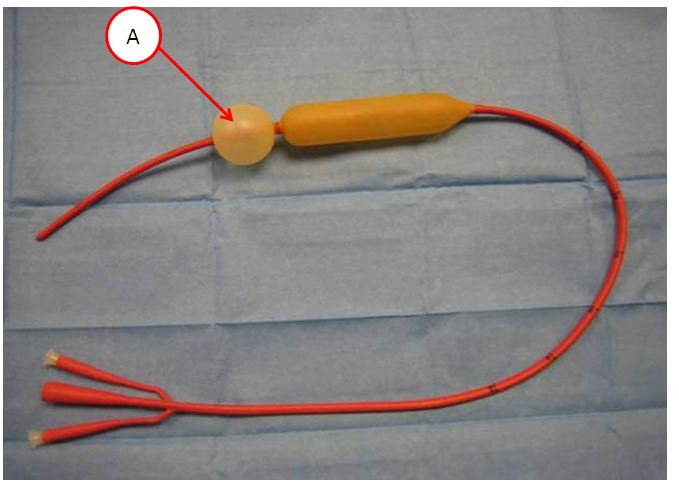
Sengstaken-Blakemore Tube (www.derangedphysiology.com)
Take Home Points
- Resuscitate early with blood and blood products to address hemodynamic instability. Remember hemoglobin will not reflect actual blood volume in acutely bleeding patient.
- Intubate early with back-up and lots of suction after first resuscitating. Have push-dose or infusion vasopressors nearby for peri- or intra-intubation hypotension
- Contact your consults early for definitive diagnosis and treatment as it will take time to prepare. Consultants provide definitive therapy after adequate ED resuscitation.
- Give antibiotics to patients with confirmed or suspected cirrhosis with UGIB. Prophylactic antibiotics shown to reduce risk of SBP and mortality.
Read More
ALiEM: Upper Gastrointestinal Bleeding: Evidence-Based Treatment
Life in the Fastlane: Gastrointestinal haemorrhage
Life in the Fastlane: Intubation in Upper Gastrointestinal Haemorrhage
Emergency Medicine Cases: Episode 101 GI Bleed Emergencies Part 1
Emergency Medicine Cases: Episode 101 GI Bleed Emergencies Part 2
EMRAP HD: Placement of a Blakemore Tube for Bleeding Varices
References
Chavez-Tapia NC, Barrientos-gutierrez T, Tellez-avila F, et al. Meta-analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding – an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509-18. PMID: 21707680
Overton DT: Upper Gastrointestinal Bleeding in Tintinalli JE, Stapczynski JS, Ma OJ, Cline DM, Cydulka RK, Meckler GD, et al (eds): Tintinalli’s Emergency Medicine: A Comprehensive Guide, ed 7. McGraw Hill Companies, Inc., 2011, (Ch) 78: p 543-545.
Sachar H et al. Intermittent vs Continuous Proton Pump Inhibitor Therapy for High-Risk Bleeding Ulcers: A systematic Review and Meta-Analysis. JAMA Intern Med 2014; 174(11): 1755 – 62. PMID: 25201154
Villanueva C, et al. Transfusion Strategies for Acute Upper Gastrointestinal Bleeding. NEJM. 368 (1): 11-21. 2013. PMID: 23281973
I like your content. You have written on the required measures to be taken after Gastrointestinal Bleeding. I believe your content will be very helpful for us. Thanks for such an awesome content.
There’s a little typo in this blog under Airway and Personal protection equipment, says use of Face Mark, vs Face mask. Funny. I envision ED staff with painted faces taking care of patients and protecting themselves that way. Forgive my humor.
Great post, thanks, Dr Taylor, Southern California.