Introduction:
- In the first 24-28 hours of life, blood glucose can fall to as low as 30-40mg/dL; a cutoff of <47-50mg/dL is often used to determine hypoglycemia.
- Early recognition and management of neonatal hypoglycemia can prevent both short-term consequences, such as seizure, and long-term consequences such as poor neurodevelopmental outcomes.
Etiology:
- Non-pathologic mechanisms of hypoglycemia in newborns include low hepatic glycogen stores, inadequate gluconeogenesis resulting from inadequate muscle stores of amino acids, and insufficient fatty acid availability.
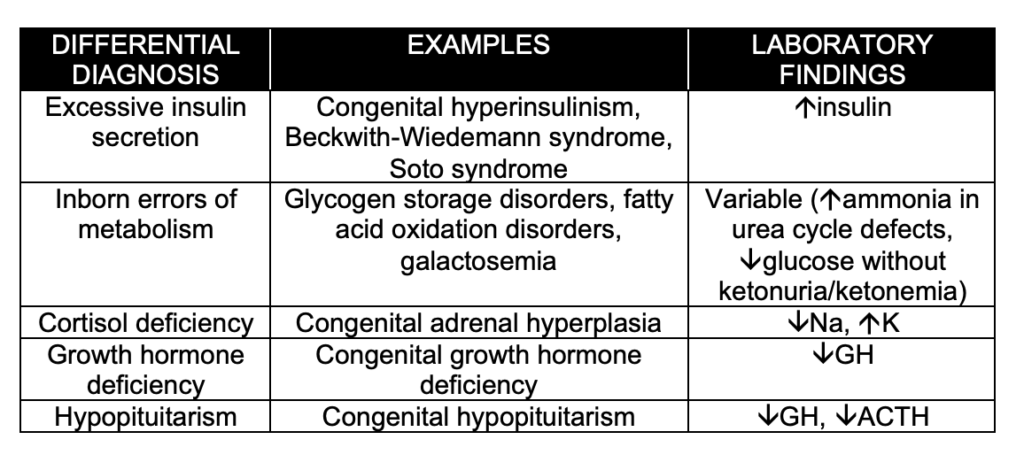
- Pathologic causes of hypoglycemia include excessive insulin secretion, inborn errors of metabolism, hormone deficiencies, and sepsis (see below).
- Both patients who are small for gestational age (SGA) and patients who are large for gestational age (LGA) can experience hypoglycemia, as can infants of diabetic mothers.
Clinical Manifestations:
- Clinical manifestations are classified as neurogenic (caused by compensatory activation of the sympathetic nervous system) and neuroglycopenic (caused by inadequate glucose delivery to the CNS).
- Neurogenic: sweating, pallor, temperature instability, irritability, hunger, tremulousness, tachycardia, vomiting
- Neuroglycopenic: apnea, hypotonia, seizure, coma, death
- Providers should check a blood glucose value in neonates who exhibit any of the above symptoms, any infant with significant vomiting and inability to take PO, and in any ill-appearing neonate.
Management:
- The “Rule of 50s” should be used to calculate the amount and concentration of glucose to be administered.
- Dextrose concentration x volume (per kg) = 50
- Provides 0.5g/kg of glucose
- Dextrose concentration x volume (per kg) = 50
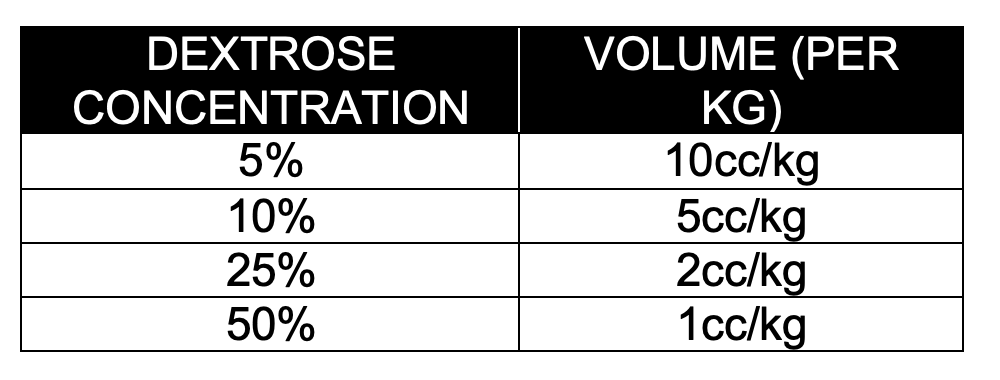
-
- NB: Dextrose concentrations higher than 10% should be avoided in infants and young children because of the risk of venous injury.
- Other treatment options exist, including glucocorticoids, glucagon, octreotide, and nifedipine; however, these should be given in consultation with pediatric endocrinology (with the exception of hydrocortisone for suspected congenital adrenal hyperplasia, CAH).
Disposition:
- Patients who are unable to maintain their blood glucose levels with frequent feedings should be admitted for further management.
- Patients who are ill-appearing or require further workup for other causes should also be admitted.
References:
1. Abramowski A, Ward R, Hamdan AH. Neonatal Hypoglycemia. [Updated 2020 Sep 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537105/Adamkin, David. Neonatal hypoglycemia. Curr Opin Pediatr. 2016;28(2):150-155. doi:10.1097/MOP.0000000000000319.
2. Alsaleem M, Saadeh L, Kamat D. Neonatal Hypoglycemia: A Review. Clin Pediatr (Phila). 2019 Nov;58(13):1381-1386. doi: 10.1177/0009922819875540. Epub 2019 Sep 26. PMID: 31556318.
3. Thompson-Branch A, Havranek T. Neonatal Hypoglycemia. Pediatr Rev. 2017 Apr;38(4):147-157. doi: 10.1542/pir.2016-0063. PMID: 28364046
Note: Please see our CoreEM post on The Critically Ill Infant for more information regarding THE MISFITS
