A look at this deadly mucocutaneous reaction and how to best manage these patients in the ED
Episode 162.0 – Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
Show Notes
Episode Produced by Audrey Bree Tse, MD
- Rash with dysuria should raise concern for SJS with associated urethritis
- Dysuria present in a majority of cases
- SJS is a mucocutaneous reaction caused by Type IV hypersensitivity
- Cytotoxic t-lymphocytes apoptose keratinocytes → blistering, bullae formation, and sloughing of the detached skin
- Disease spectrum
- SJS = <10% TBSA
- TEN = >30% TBSA
- SJS/ TEN Overlap = 10-30% TBSA
- Incidence is estimated at around 9 per 1 million people in the US
- Mortality is 10% for SJS and 30-50% for TEN
- Mainly 2/2 sepsis and end organ dysfunction.
- SJS can occur even without a precipitating medication
- Infection can set it off especially in patients with risk factors including HIV, lupus, underlying malignancy, and genetic factors
- SATAN for the most common drugs
- Sulfa, Allopurinol, Tetracyclines, Anticonvulsants, and NSAIDS
- Anti-epileptics include carbamazepine, lamictal, phenobarb, and phenytoin
- Can have a curious course
- Hypersensitivity reaction can develop while taking medication, or even one to four weeks after exposure
- In pediatric population, mycoplasma pneumonia and herpes simplex have been identified as precipitating infections
- Patients often have a prodrome 1-3 days prior to the skin lesions appearing
- May complain of fever, myalgias, headaches, URI symptoms, and malaise
- Rash may be the sole complaint
- Starts as dark purple or erythematous lesions with purpuric centers that progress to bullae
- Skin surrounding the lesions detaches from the dermis with just light pressure (Nikolsky Sign)
- Up to 95% of patients will have mucous membrane lesions
- ~85% will have conjunctival lesions
- Symptoms: Burning or itching eyes, a cough or sore throat, pain with eating, pain with urinating or defecating
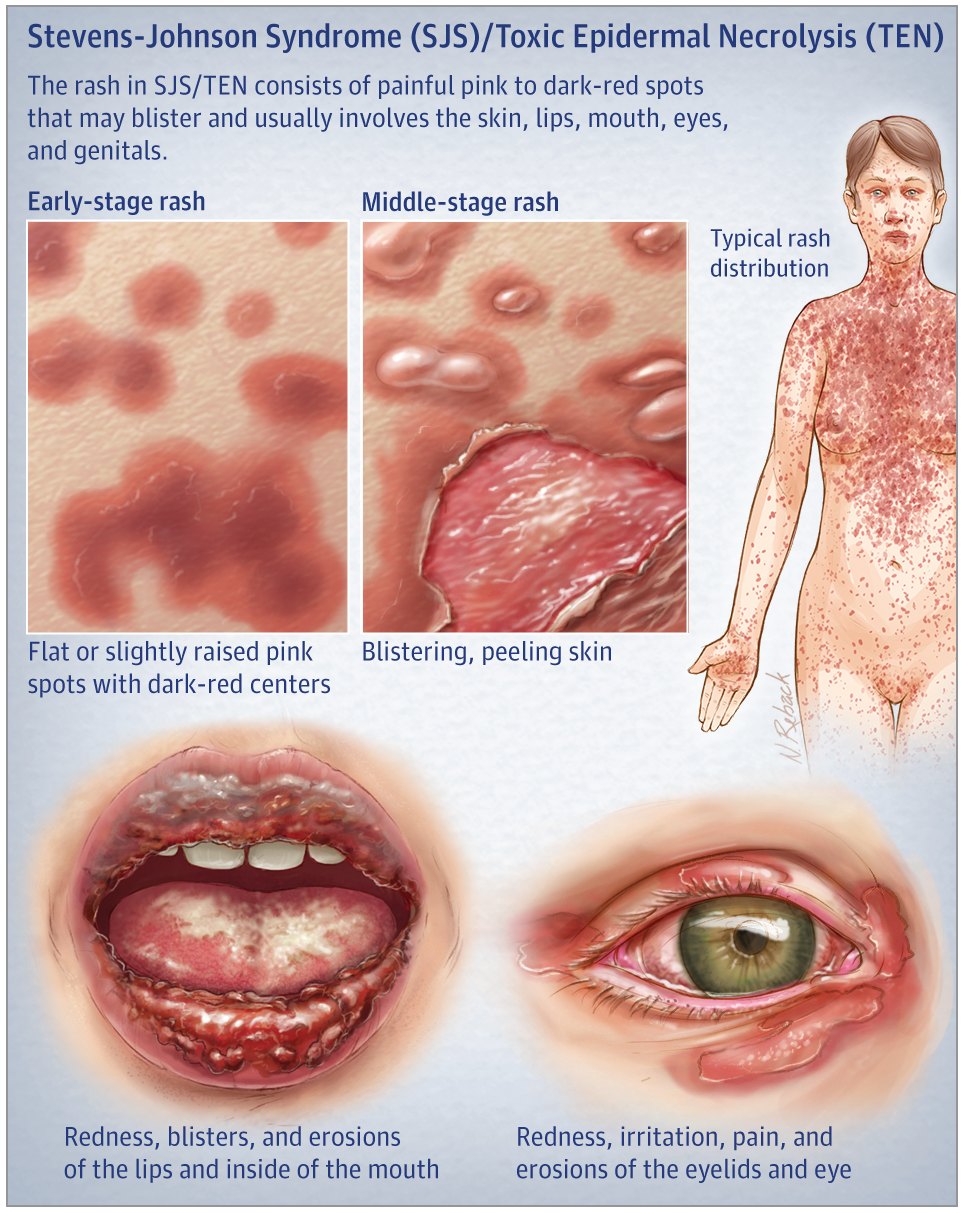
Source: JAMA Dermatol. 2017
- Differential Diagnosis: SSSS, autoimmune bullous diseases, bullous fixed drug eruption, erythema multiforme, thermal burns, phototoxic reactions, and TSS
- SJS is a clinical diagnosis
- Basic workup: CBC, chemistry panel, LFTs, and a UA
- Treatment
- Supportive care
- IV fluid repletion guided by TBSA affected, as well as electrolyte, protein, and energy supplementation
- Consider protecting airway if significant oral mucosal involvement
- Stop the offending agent (if there is one)
- Advanced wound care and pain control
- Consults: Derm to do a biopsy, +/- ophthalmology, gyn / urology to prevent strictures or contractures
- Consider transferring to a burn center
- Supportive care
- Dispo:
- Low threshold for ICU admission
- SCORTEN ( max of 7 points)
- 1 point each for
- Age over 40
- Current cancer
- >30% body surface area affected
- HR >120
- BUN >28
- Glucose >240
- Bicarb <20
- Score of 2 points or higher should -> ICU
- 1 point each for
Take Home Points
- SJS may begin like the flu, with lesions appearing 1-3 days after the prodrome starts
- Have to have a high suspicion for SJS because it is deadly. It’s a clinical diagnosis — derm biopsy is supportive
- A thorough history and physical exam are key. Remember the characteristic rash and bullae, and always look in the mouth and eyes. Ask about dysuria, sore throat, and eye irritation, as well as preceding medications or infections. Think SATAN!
- Prompt supportive care focused on ABCs and IVF repletion are critical. These patients can get sick really fast, so consider an ICU or burn unit.
References:
Barrett W. Quick Consult: Symptoms: Rash, Dysuria, and Mouth Sores. Emergency Medicine News. 41(4): 15-16, April 2019.
Bivins H, Comes J. Stevens-Johnson Syndrome. Rosen and Barkin’s 5-Minute Emergency Medicine Consult. 2015; 1076-1077.
Ergen EN, Hughey LC. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. JAMA Dermatol.2017;153(12):1344. doi:10.1001/jamadermatol.2017.3957
Gerull R, Nelle M, Schaible T. Toxic epidermal necrolysis and Stevens-Johnson syndrome: A review. Crit Care Med. 2011; 39:1521-1532.
Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Rev Allergy Immunol. 2018;54(1):147-76.
McNeil, D. (2019). Measles Cases Surpass 700 as Outbreak Continues Unabated. [online] Nytimes.com. Available at: https://www.nytimes.com/2019/04/29/health/measles-outbreak-cdc.html [Accessed 6 May 2019].
Mustafa SS, Ostrov D, Yerly D. Severe Cutaneous Adverse Drug Reactions: Presentation, Risk Factors, and Management. Curr Allergy Asthma Rep. 2018;18(4):26.


