Background
Sepsis remains a condition with a high mortality rate, and prompt recognition of the condition is essential. The presence and severity of fever raises suspicion for infection and is frequently a significant factor in medical decision making in the Emergency Department (ED). However, many septic patients are not febrile, which can impede prompt identification of critically ill patients.
Clinical Question
What is the prognostic value of the presence of fever in ED patients admitted to the intensive care unit (ICU) for severe sepsis or septic shock?
Population
All patients over age 17 admitted to 30 ICUs across Sweden diagnosed with severe sepsis or septic shock within 24 hours of arrival to an ED between 2007 and February 2015.
Outcomes
Primary:In-hospital mortality
Design
Observational cohort study based on a prospectively compiled registry of sepsis patients in Sweden, the Swedish national quality sepsis register (SNQSR)
Excluded
Patients lacking data on survival
Patients lacking body temperature (BT) measurement in the ED
Patients transferred to the ICU after 24 hours
Patients lacking fundamental data
Primary Results
- 2,610 patients were recorded in the SNQSR. After excluding patients, primarily for missing data, 2,225 were included in the main analysis.
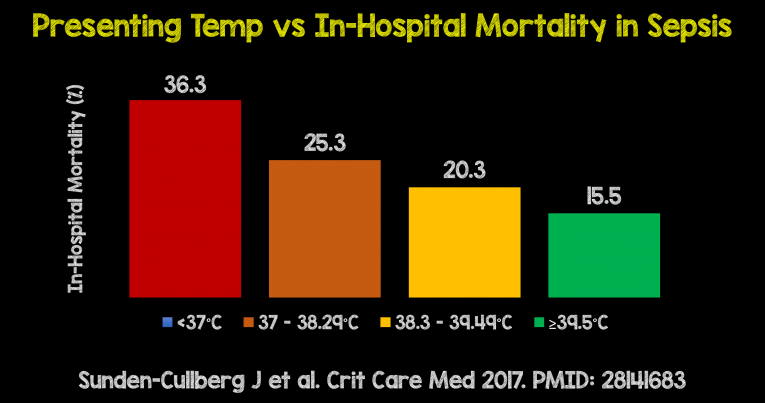
- Patients were divided into 4 groups based on BT
- < 37°C, 37–38.29°C, 38.3–39.5°C, ≥39.5°C
- Odds ratios for mortality were calculated
- Subgroup analyses were also performed to adjust for age, sex, disease severity, and treatment
Critical Results
- Interestingly, “Mortality was inversely correlated with temperature and decreased, on average, more than 5% points per °C increase, from 50% in those with the lowest temperatures to 9% in those with the highest.”
- In the 37°C, 37–38.29°C, 38.3–39.5°C, and ≥39.5°C groups, mortality was 36.3%, 25.3%, 20.3% and 15.5%, respectively.
- Patients with increased body temperature in the ED had shorter hospital stays, and received better quality of care by sepsis guidelines.
- When controlling for quality of care and other possible confounders, the inverse mortality relationship with temperature remained. In the 37°C, 37–38.29°C, 38.3–39.5°C, and ≥39.5°C groups, length of stay among survivors was 17, 13, 11, and 11 days, respectively.
- Of the clinical signs, body temperature had the highest predictive value for in-hospital mortality. This was followed by respiratory rate, heart rate, O2 saturation, and systolic blood pressure, in that order.
- A strong correlation between temperature and mortality was present when subgroup analyses were performed adjusting for age, lactate level, microbiological etiology (gram positive vs negative vs other), and sepsis bundle completion.
Sepsis-Fever Relationship (Courtesy of Salim Rezaie)
Strengths
- Large, multicenter study with good capture of patients
- First study investigating the prognostic significance of fever in septic patients
- Robust statistical analysis to account for confounding variables, such as comorbidities and severity of illness.
- Inverse correlation between BT and mortality was present in all statistical models, and there is the suggestion that patients with missing data would likely have increased the correlation
Limitations
- Sweden has a national health system, and their patient population and management of sepsis may differ from other locations
- The sepsis database used in this study did not include disease severity scores such as Sequential Organ Failure Assessment or Acute Physiology and Chronic Health Evaluation (not recorded in the NQSR), which would have allowed for more precise adjustment for disease severity
- Temperature was not measured by one standard approach (i.e. oral, ear or rectal)
- 42% of patients had at least some data missing
- ~ 10% of patients did not have a temperature measured
Author's Conclusions
“Contrary to common perceptions and triage guidelines, this study shows a strong inverse association between BT at ED admission and mortality and LOS in septic patients admitted to the ICU. Quality of care, including prompter antibiotic treatment, improved with rising BT, but this did not explain lower mortality.”
Our Conclusions
This large, multicenter center study provides good evidence for an inverse relationship between first BT measured in the ED and mortality in patients admitted to the ICU for severe sepsis or septic shock. The presence of fever on initial presentation tends to initiate more complete and rapid sepsis treatment, but this is unlikely to be the only factor contributing to these findings.
Potential Impact To Current Practice
This study reinforces the fact that many patients presenting with sepsis will be afebrile, but also provides good evidence that the sickest patients will lack a fever. This study reminds us to be vigilant in trying to detect sepsis early.
Bottom Line
Fever is not the sine qua non of sepsis: septic patients can be afebrile and it is this group that we need to be particularly vigilant in identifying as they currently appear to have increased in-hospital mortality.
Read More
REBEL EM: Is Fever the New Hotness?
Scan Crit: Is Fever the Normal Temperature of Sepsis