Background
There is scant evidence published on the long-term outcomes of systemic thrombolysis in acute submassive PE. Many advocate for the use of systemic thrombolysis to reduce morbidity (complications from chronic pulmonary hypertension) and mortality. The PEITHO trial compared systemic thrombolysis (with tenecteplase + heparin) vs no systemic thrombolysis (placebo + heparin) in just over 1000 patients with confirmed PE, RV dysfunction, and positive troponins. The primary outcome of all-cause death or hemodynamic decompensation within 7 days occurred less frequently in the thrombolysis arm. This statistically significant difference was driven by differences in hemodynamic decompensation, not mortality – a non-patient centered outcome. Additionally, the benefit was at the risk of increased intracranial hemorrhage. In this current study, 70% of the patients from the original PEITHO trial were followed for a 2-year follow up period, giving us some information about long-term sequelae of systemic thrombolysis in patients with submassive PE.
Clinical Question
Are there long-term benefits in terms of functional outcomes and mortality from the use of systemic thrombolytics in patients with submassive PE?
Population
Patients > 18 years of age with confirmed PE with onset < 15 days with RV dysfunction (diagnosed on echo and/or CT) and with myocardial injury (diagnosed with positive cardiac troponin I or T)
Intervention
Weight-based tenecteplase in addition to heparin
Control
Placebo in addition to heparin
Outcomes
Long-term mortality, clinical outcomes (persistent dyspnea or functional capacity) or echocardiographic findings of pulmonary hypertension
Design
This study is a follow up from the PEITHO study. The PEITHO study was a randomized, multi-national, double-blind, placebo-controlled trial
Primary Results
- Long-term outcomes available for > 98% of patients
- Median follow up 37.8 months
Critical Findings:
- Overall mortality
- At < 30 days
- No statistically significant difference
- Tenecteplase 2.2% vs. Placebo 2.9% (p = 0.595)
- Randomization until follow up
- No statistically significant difference
- Tenecteplase 20.3% vs. Placebo 18.0% (p = 0.430)
- At < 30 days
- Persistent dyspnea or functional impairment
- No statistically significant difference
- Tenecteplase 36.0% vs. Placebo 30.1% (p = 0.430)
- Echocardiogrpahic findings
- Follow up echo performed in < 50% of patients
- No statistically significant difference in any parameter
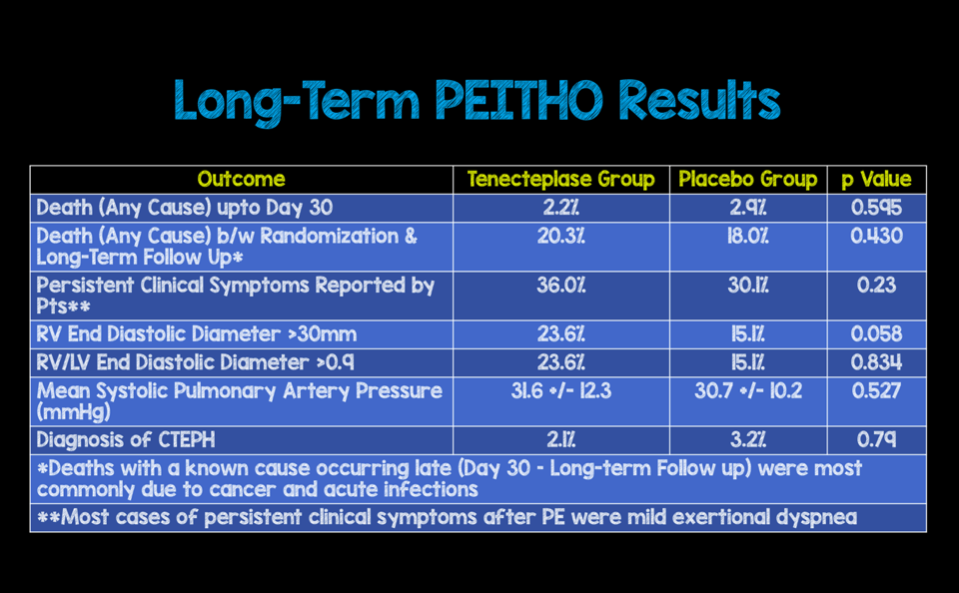
Long-Term PEITHO Results
Strengths
- Multicenter, double-blind randomized control trial
- Largest patient population to date answering an important patient oriented outcome
- There was no real baseline differences in patients followed long-term vs those not followed long term with two exceptions:
- Body weight: 81.8 +/- 17.9kg vs 84.4 +/- 18.3kg
- History of previous VTE: 25% vs 32.4%
Limitations
- Many causes of late death (beyond 30 days) were not able to be identified
- Clinical and echocardiographic evaluation could not be performed on all survivors. Therefore, this data cannot be considered the definitive evidence of how often pulmonary hypertension or RV dysfunction persists after acute PE
- Study did not investigate recurrent PE rates in the two groups which, previously, was shown to be decreased after systemic lytics
- The rate of chronic thromboembolic pulmonary hypertension (CTEPH) after acute PE was low (2.7%), which is lower than rates observed in earlier cohort studies
- The diagnostic algorithm for suspected CTEPH was not part of the original PEITHO trial protocol
Author's Conclusions
”Approximately 33% of patients report some degree of persistent functional limitation after intermediate-risk PE, but CTEPH is infrequent. Thrombolytic treatment did not affect long-term mortality rates, and it did not appear to reduce residual dyspnea or RV dysfunction in these patients.”
Our Conclusions
In the current trial, long-term mortality rates and long-term morbidity (residual dyspnea, functional limitations, and persistent RV dysfunction) were not affected by the use of systemic thrombolysis.
Potential Impact To Current Practice
The results of this study may move more providers away from giving systemic thrombolytics in undifferentiated submassive PE.
Bottom Line
Systemic lytics given along with heparin should not be used as the standard approach for all patients with submassive PE. Until further data suggests otherwise, patients need to be carefully considered for lytics based on their clinical parameters.
Read More
EM Nerd (EMCrit): The Case of the Shadowy Spector
PulmCrit (EMCrit): Submassive PE 2017 – Getting ‘em off the Cliff
REBEL EM: Episode 38 – Do All Submassive PE’s Require Treatment with Thrombolysis
REBEL EM: Treatment of Submassive Pulmonary Embolism (PE): Full Dose, Half Dose, or No Dose?
The SGEM: SGEM #184 – We Weren’t Born to Follow-Up – The PEITHO Long-Term Follow-Up Study
ALiEM: PEITHO Trial – Fibrinolysis for Intermediate-Risk Pulmonary Embolism
St. Emlyn’s Blog: The Argument for Systemic Thrombolytics in Submassive Pulmonary Embolism
References
Meyer G et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. NEJM 2014; 370(15):1402-1411. PMID: 24716681

Thank you for this post. Please consider adding the SGEM review of the paper.
http://thesgem.com/2017/07/sgem184-we-werent-born-to-follow-up-the-peitho-long-term-follow-up-study/
Oversight on our part. Added!