Special thanks to Salim Rezaie for providing expert peer-review for this post.
Background
The presence of a left bundle branch block (LBBB) on EKG can make recognition of an acute ST segment elevation myocardial infarction (STEMI) difficult. While a patient with a new or presumed new LBBB and either hemodynamic instability or signs of heart failure should be transferred for percutaneous coronary intervention or coronary artery bypass, patients with chronic LBBB present more challenging decisions. Patients with LBBB tend to have “appropriate discordance” of ST segments and T waves (i.e. ST segments and T waves are typically shifted in a discordant direction at baseline). This has the potential to delay diagnosis and, thus, effect patient outcomes. Understanding the available criteria for making this diagnosis is critical.
Cardiac Conduction System (www.heart.valve-sugery.com)
The Left Bundle Branch Block (See post from REBEL EM for further information)
Definition: A LBBB is a cardiac conduction abnormality in which activation of the left ventricle is delayed due to a block in conduction down the left bundle branch.
Normal Conduction
- Impulses from the AV node spread down the left bundle more rapidly than the right bundle
- The intraventricular septum is depolarized from left to right
Conduction in a LBBB
- Impulses spread down the right bundle branch and then across the septum to the left ventricle
- Produces tall R waves in the lateral leads (I, aVL, V5-6) due to depolarization of the RV prior to the LV and deep S waves
- Produces a left axis deviation
LBBB Criteria
- QRS > 120 msec
- Dominant S wave in V1 (due to proximity of lead V1 to RV)
- Broad R waves in the lateral leads (I, aVL, V5-6) that are monophonic
- Absence of Q waves in the lateral leads (I, V5-6)
- R wave peak time is prolonged (> 60 msec) in V5-6

EKG with LBBB
The Sgarbossa Criteria (Sgarbossa 1996)
Purpose: The Sgarbossa criteria were created to address the issue of diagnosing STEMI in the presence of a LBBB. At the time of publication of this article, there was no reliable system for doing this.
Criteria
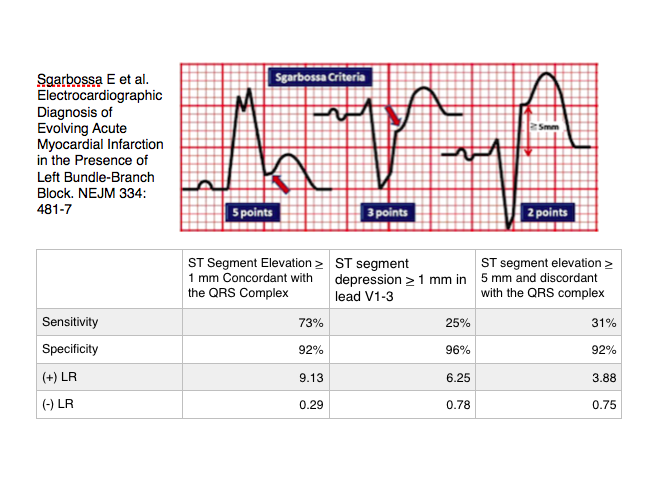
The Original Sgarbossa Criteria (Sgarbossa 1996)
Critique of Original Sgarbossa Criteria
- Decision instruments looking for STEMI should be highly sensitive
- High sensitivity ensures that cases aren’t missed
- Meta-analysis of 11 studies and 2100 patients looking at score > 3 (Tabas 2008)
- Sensitivity 20%
- Specificity 98%
- (+) LR = 7.9
- (-) LR = 0.89
- Bottom Line: The original Sgarbossa criteria are fairly good at “ruling in” STEMI in the setting of a LBBB but they are extremely bad at ruling the disease out.
- Specificity is good but suboptimal leading to false positive screening and, thus, false positive cardiac catheterization lab activation
- Acute myocardial infarction (AMI) was defined as an elevation in CK-MB not by evidence of acute coronary occlusion. This limits the rule’s sensitivity as it groups NSTEMI and STEMI together.
- The weighted scoring system reduces false positive results
- A score > 3 has a specificity of > 95% (Cai 2013)
- The weighted score reveals the low predictive value of criteria 3 (disconcordant elevations > 5 mm) as this criteria doesn’t provide enough points to diagnosis acute myocardial infarction (AMI)
The Modified Sgarbossa Criteria
Purpose: Response to shortcomings of the original Sgarbossa criteria attempting to increase the value of criteria 3 and, subsequently, increase the sensitivity for detection of AMI in the setting of a LBBB
Criteria (Smith 2012)
- Criteria 1 and 2 are preserved in their current state. If either of these is present, the patient should be considered to have a STEMI
- The absolute > 5 mm ST elevation in criteria 3 is replace with a proportional criterion
- Proportional criteria looks for an ST-segment (measured at the J-point) to R or S-wave (whichever is more prominent) ratio < – 0.25
- Discordant deviation of > 1 mm
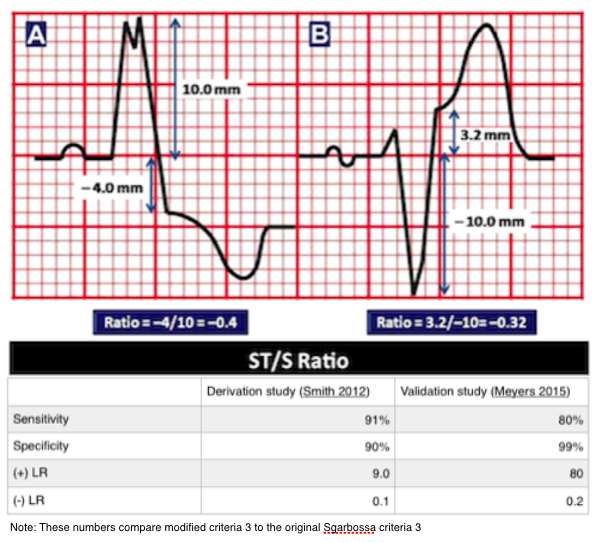
The Modified Sgarbossa Criteria (Smith 2012)
Performance of Modified Sgarbossa Criteria
- The modified Sgarbossa criteria have increased sensitivity in comparison to the original criteria with only a small decrease in specificity
- Neither the derivation nor validation studies are prospective. Further external validation using a prospective methodology would be useful
- Although the modified criteria requires a calculation not performed by the EKG machine, it is simple and easy to perform
Bottom Line: Although the modified Sgarbossa criteria should undergo prospective validation, it seems unlikely that the replacement of absolute discordant elevations with proportional elevations will be less sensitive than the original criteria. Adoption of this modified Sgarbossa criteria will likely lead to better detection of STEMI in the presence of a LBBB.
- The original Sgarbossa paper included only 17 patients with paced rhythms making it difficult to draw conclusions from this data set (Sgarbossa 1996)
- Retrospective data (Maloy 2010)
- Identified 57 patients with AMI and LBBB and compared them to 99 patients with LBBB and no AMI
- Criteria 1 (Concordant ST elevation): No data available as no EKGs fit this criteria
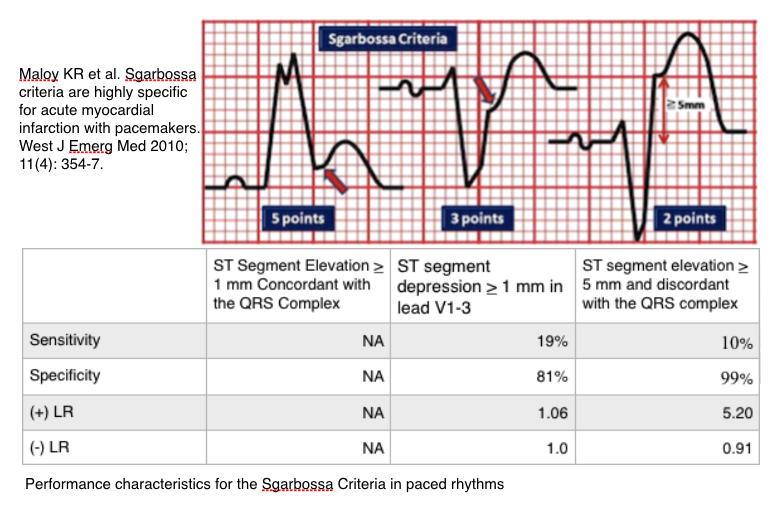
Bottom Line: Sgarbossa criteria are not sensitive for detecting AMI in paced rhythms with LBBB morphology but, the original Sgarbossa criteria 3 appears to be highly specific based on the best available evidence.
How Should the Modified Sgarbossa Criteria Be Applied Clinically?
Activate the cardiac catheterization lab for all patients with (Cai 2013)
- A new or presumed new LBBB with either hemodynamically instability or signs of heart failure (not discussed in this post)
- Sgarbossa criteria score > 3 (highly specific for AMI)
- Modified Sgarbossa criteria is positive: ST/S ration < – 0.25
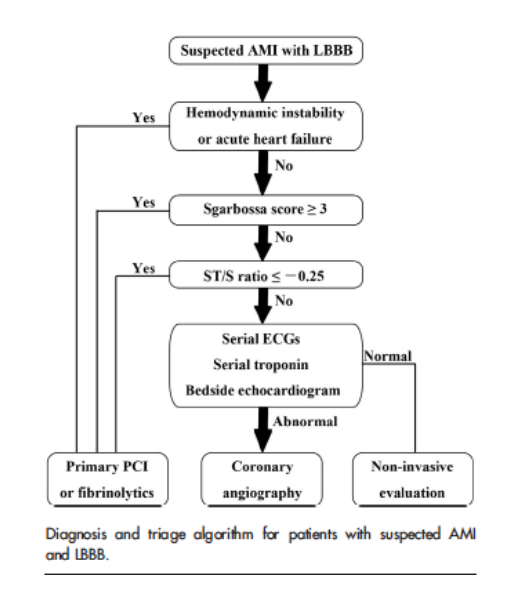
Diagnostic Algorithm for Suspected in AMI in LBBB (Cai 2013)
Take Home Points
- Detection of an STEMI in patients with an underlying LBBB can be challenging but it is not impossible.
- The presence of a Sgarbossa criteria score > 3 should prompt immediate cardiac catheterization lab activation.
- Application of the modified Sgarbossa criteria increases sensitivity of STEMI detection with little loss of specificity and should be incorporated into decision making.
- There is little guidance on identifying STEMI in paced rhythms with LBBB morphology. If the patient’s symptoms are concerning, consider emergent cardiology consultation regardless of the EKG findings.
Read More
ECG Case of the Week: November 4th, 2013
LITFL: Left Bundle Branch Block
REBEL EM: Bundle Branch Blocks 101
REBEL EM: Modified Sgarbossa Criteria: Ready for Primetime?
REBEL EM: Modified Sgarbossa Criteria: Part Deux
Dr. Smith’s ECG Blog: Validation of Smith Modified Sgarbossa Criteria Published in American Heart Journal
References
Sgarbossa E et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. NEJM 1996; 334: 481-487 PMID: 8559200
Tabas JA et al. Electrocardiographic criteria for detecting acute myocardial infarction in patients with left bundle branch block: a meta-analysis. Ann Emerg Med 2008;52(4): 329-36. PMID: 18342992
Cai Q et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J 2013; 166(3): 409-13. PMID: 24016487
Smith S et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Ann Emerg Med 2012; 60(6): 766-76. PMID: 22939607
Meyers HP et al. Validation of the Modified Sgarbossa Criteria for Acute Cornoary Occlusion in the Setting of Left Bundle Branch Block: A Retrospective Case-Control Study. Am Heart J 2015; 170: 1255 – 1264. PMID: 26678648
Maloy KR et al. Sgarbossa criteria are highly specific for acute myocardial infarction with pacemakers. West J Emerg Med 2010; 11(4): 354-7. PMID: 21079708

This is truly a great post! I have some minor comments. Most of them are nothing important.
1. This sentence: “While a patient with a new or presumed new LBBB and either hemodynamic instability or signs of heart failure should be transferred for percutaneous coronary intervention or coronary artery bypass, patients with chronic LBBB present more challenging decisions.” –> is this in line with ACC/AHA/ESC guidelines? Last time I checked them they did not mention anything about hemodynamics or heart failure symptoms. Good to be sure on this, because it affects management.
2. “Impulses from the AV node spread down the left bundle more rapidly than the right bundle”. –> I’m not sure that it is correct. Transmission speed is equal (4 meters/s) in left and right BBB, which consist of identical fibers. However, the right bundle branch does not give of any Purkinje Fibers until reaching the origin of the anterior papillary muscle (of the right ventricle).
3. “Produces a left axis deviation”. –> If I recall correctly, left ax dev only occurs in 40% of the cases. It is not, however, a criteria.
4. “Broad R waves in the lateral leads (I, aVL, V5-6) that are monophonic” –> the term “monophonic” should perhaps be “monophasic”?
5. This sentence: “There is little guidance on identifying STEMI in paced rhythms with LBBB morphology. If the patient’s symptoms are concerning, consider emergent cardiology consultation regardless of the EKG findings.” –> Might be worth noting that paced rhythms can be checked for ischemia by activating the magnet function. This pauses the pacing and unmasks the intrinsic QRS-ST-T morphology. However the following must be noted: (1) this can not be done in patients who are completely dependent on their pacemaker and (2) the intrinsic QRS-ST-T morphology may show something called “cardiac memory” (or “ST-T memory”), which basically means that the discordance persist for a few hours or even days after shutting off the pacemaker.
If you need any figures from http://www.ecgwaves.com please let me know.
Coreem is superb!
Cheers!