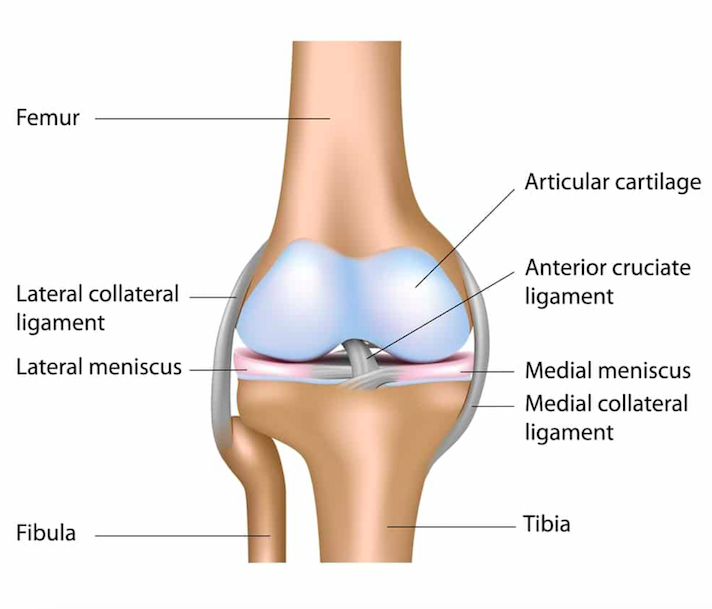
Anterior View of the Knee (www.howardluksmd.com)
Definition: Stretch or tear of the medial collateral ligament (MCL).
Epidemiology
- Ligamentous injuries have been cited to account for ~40% of knee injuries (Bolen 2000)
- The MCL is the most commonly injured ligament, accounting for ~8% of all knee injuries (Majewski 2006)
- Women > Men (Swenson 2013)
Mechanism
- Direct blows are the most common mechanism and typically cause more severe injuries (Singhal 2010).
- Indirect mechanisms are less common. They occur with a valgus stress with external rotation force to the lateral knee, i.e. when an athlete’s shoe gets caught on a playing surface during quick direction changes, or when an athlete catches a tip or the inside edge of a ski or skate.
- The MCL is the first (and therefore most common) structure affected in a predictable series of injuries from a valgus stress
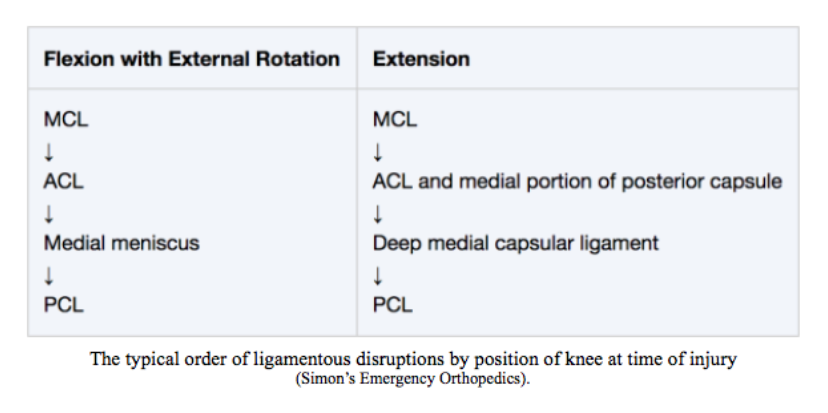
Order of Ligamentous Disruption (Simon’s Orthopedics)
Physical Exam
- General Principles
- Should be performed as soon as possible as swelling and muscle spasm occur early and obscure assessment
- Both knees should be examined using a systematic approach – inspection, palpation, testing range of motion, and using special maneuvers specific for certain injury patterns
- While it is important to evaluate the entire knee, this section will focus on findings specific to MCL injuries
- Inspection
- Assess the patient’s gait and ability to bear weight which can sometimes indicate injury severity
- Patients can often have localized swelling but effusions are uncommon in isolated MCL injuries.
- The presence of an effusion is highly suggestive of associated fractures, meniscal or cruciate injuries.
- Palpation
- Tenderness at the medial joint line suggests MCL injury
- Can also indicate medial meniscal injury and is therefore a nonspecific finding
- Range of Motion
- Pain from an isolated MCL injury can limit active motion, particularly terminal knee extension and flexion beyond 100 degrees
- Isolated MCL injury generally does not constrain passive range of motion
- Special Maneuvers – Valgus stress (abduction) test
- Laxity at 30 degree flexion => MCL injury
- Laxity at full extension => MCL +/- ACL/PCL injuries.
- To objectively assess laxity, hold finger at medial joint line and feel for medial joint widening (see injury grading below).
- Ultrasound can help quantify degree of medial joint widening.
- Always compare to uninjured knee to understand baseline joint laxity
- Detection of ligamentous laxity can be limited by spasm of surrounding muscles
Injury Classification
- Grade I (mild)
- Stretch injury
- No laxity elicited with valgus stress (i.e. <5mm medial joint widening)
- Grade II (moderate)
- Partial tear of MCL
- 5-9mm medial joint widening
- Grade III (severe)
- Complete tear
- 10mm or more of medial joint widening
- Typically less painful versus lower grade injuries
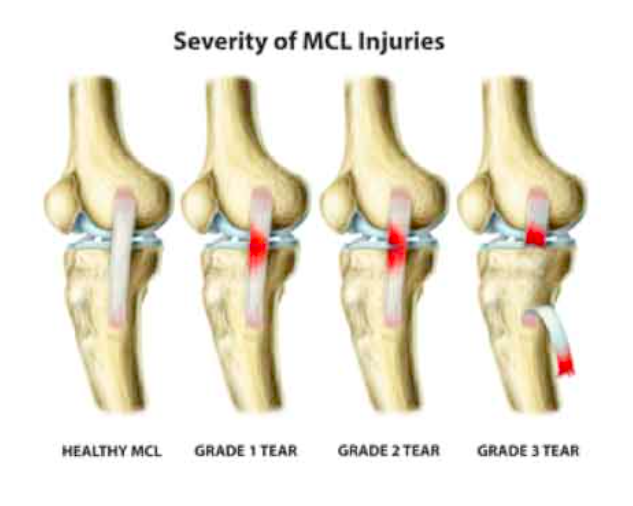
MCL Injury Grading System (zamst.us)
ED Management
- Regardless of injury grade, ED management of isolated MCL injuries is supportive
- Ice, compression, elevation, and NSAIDs
- Weight bearing as tolerated
- A hinged knee brace should be applied
- Protect against additional valgus injury
- Avoid knee immobilizers as they can lead to knee stiffness and muscle weakness
- Always encourage early mobilization (within the first week)
- Indications for emergent ortho consultation
- Associated open fracture
- Neurovascular deficit
- Suspected tibiofemoral dislocation
- Unstable knee joint
- Due to muscle spasm and soft tissue swelling, an unstable knee might appear stable
- Immobilize, make non-weight bearing, and obtain close follow-up if unstable joint without evidence of dislocation (within 1 week) for re-examination

Reverse Second Fracture: Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 19490
Imaging in the ED
- Plain Radiographs
- Views: AP, lateral, patellar (45 degrees flexion)
- Generally not necessary to evaluate isolated MCL injuries, but should be performed if concern for associated fractures
- Typically normal in isolated MCL injuries
- A “reverse segond” fracture is a subtle avulsion fracture of the medial tibial condyle that represents an avulsion of the deep portion of the MCL
- Ultrasound (Craft 2015)
- Can identify MCL injuries via abnormal MCL appearance
- Can quantify degree of medial joint opening during valgus stress testing
- CTA: Should be performed in all patients with clinical features concerning for an unstable knee, who do not have hard signs of vascular injury
- MRI: Can be done at outpatient for simple MCL injury to help identify extent of injury.
Prognosis
- Functional recovery from isolated MCL injuries is dependent on grade of injury, and achieved with physical therapy focused on gradual strengthening and range of motion exercises
- Grade I: return to activity in ~1wk
- Grade II: 2-4wks
- Grade III: 4-8wks
- Multiple prospective case-control studies have shown no difference in functional outcomes for non-op vs operative management in isolated MCL injuries (Reider 1994, Lundberg 1996, Lundberg 1997).
Take Home Points
- MCL injuries are commonly seen in the ED and the diagnosis is based on the physical exam
- Isolated MCL injuries can be managed conservatively in the ED, and safely discharged with sports medicine follow-up in 1-2 weeks
- If the patient has an unstable knee or an effusion, consider a tibiofemoral dislocation
Read More
Core EM: True Knee and Patellar Dislocations
References
McMahon PJ et al. Chapter 3. Sports Medicine. Current Diagnosis & Treatment in Orthopedics, 5e Eds. Harry B. Skinner, and Patrick J. McMahon. New York, NY: McGraw-Hill, 2014
Bond MC. Chapter: Knee. Simon’s Emergency Orthopedics, 7e Ed. Scott C. Sherman. New York, NY: McGraw-Hill, 2014
Bollen S et al. Epidemiology of knee injuries: diagnosis and triage. Br J Sports Med. 2000;34(3):227-8. PMID: 10854030
Majewski M et al. Epidemiology of athletic knee injuries: A 10-year study. Knee. 2006; 13(3): 184-8. PMID: 16603363
Swenson DM et al. Epidemiology of knee injuries among U.S. high school athletes. Med Sci Sports Exerc. 2013 Mar;45(3):462-9. PMID: 23059869
Singhal M et al. Medial ligament injuries. In: DeLee and Drez Orthopaedic Sports Medicine, DeLee J, Drez D, Miller M (Eds), Saunders, Philadelphia 2010. p.1629.
Kaufman SL, Martin LG. Arterial injuries associated with complete dislocation of the knee. Radiology 1992; 184(1):153-5. PMID:1609074
Craft JA, Kurzweil PR. Physical examination and imaging of medial collateral ligament and posteromedial corner of the knee. Sports Med Arthrosc. 2015; 23(2):e1-6. PMID: 25932881
Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures. A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med. 1996; 24(2): 160-3. PMID: 8775113
Reider B et al. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994; 22(4): 470-7. PMID: 7943511
Lundberg M, Messner K. Ten-year prognosis of isolated and combined medial collateral ligament ruptures. A matched comparison in 40 patients using clinical and radiographic evaluations. Am J Sports Med. 1997; 25(1): 2-6. PMID: 9006684