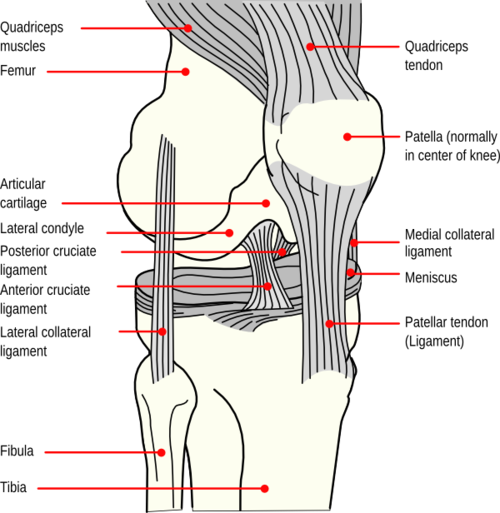
Knee Anatomy (www.stoneclinic.com)
Definition
- Knee dislocation: Tibiofemoral dislocation defined as complete displacement of the tibia with respect to the femur, with disruption of 3 or more of the stabilizing ligaments (ACL, PCL, MCL, lateral ligament complex/LCL)
- Patella dislocation: Patellar displacement from the trochlear groove
Mechanism
- Knee: Usually a high energy mechanism such as a fall from height, motor vehicle accident (dashboard injury), or high-speed athletic injury (downhill skiing). Can also be from a low-energy mechanism such as a fall from standing in the morbidly obese or a seemingly more benign sports injury such as a football tackle.
- Patella: Typically caused by direct trauma or from a twisting movement on a flexed knee
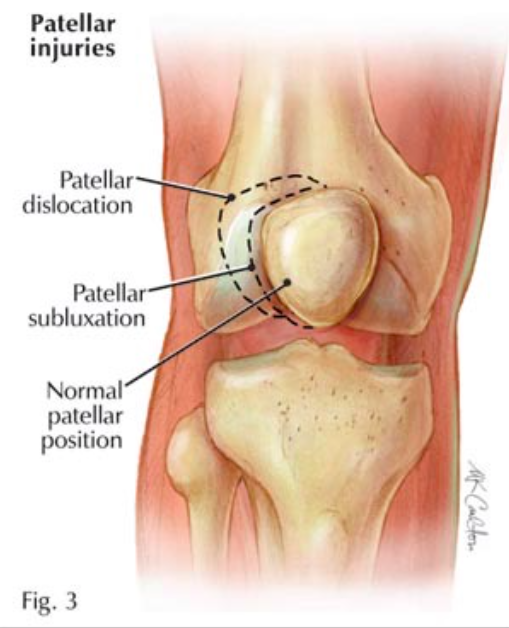
Patellar Dislocations (www.hughston.com)
Epidemiology
- True knee dislocations are rare
- The Mayo Clinic recorded 14 knee dislocations during an interval of 2 million admissions (Taylor 1972)
- The largest reported series of knee dislocations is from Los Angeles County Hospital, where 53 knee dislocations were reported over a 10-year period
- The true incidence of knee dislocations is likely higher than reported because 50% of knee dislocations spontaneously reduce before patients present to the emergency department (Kennedy, 1963)
- Patellar dislocations
- Annual patellar dislocation rate is approximately 43/100,000 (Brown, 2006).
- The majority are lateral. Superior, medial and intra-articular dislocations are uncommon.
- Young athletes suffer patellar dislocations more commonly than any other group, and the average age of occurrence is 16–20 years.

Knee Dislocation (emedicine.medscape.com)
Physical Examination
- Knee dislocations
- Many are clinically obvious given the history of acute trauma and the grossly abnormal position of the knee
- Spontaneous Relocation
- Up to 50% may have a normal appearance following spontaneous reduction prior to presentation
- When there is concern for a spontaneously reduced dislocation, look for more subtle signs of injury including swelling, ecchymosis and joint effusion
- Injury to the popliteal artery is the most feared complication and is common
- Check for popliteal, dorsalis pedis (DP) and posterior tibialis (PT) pulses
- Assess for joint instability by testing each cruciate ligament for laxity both at zero and 30 degrees of flexion

Patella Dislocation (www.exceptyou.org)
- MCL/LCL: Varus/valgus stress
- ACL/PCL: Anterior/posterior stress
- Patellar dislocation
- Inspection reveals a swollen knee typically held in 20 to 30 degrees of flexion with the patella displaced
- Perform distal neurovascular exam including DP/PT pulses. (Brown, 2006)
Knee Dislocations (www.emedicinehealth.com)
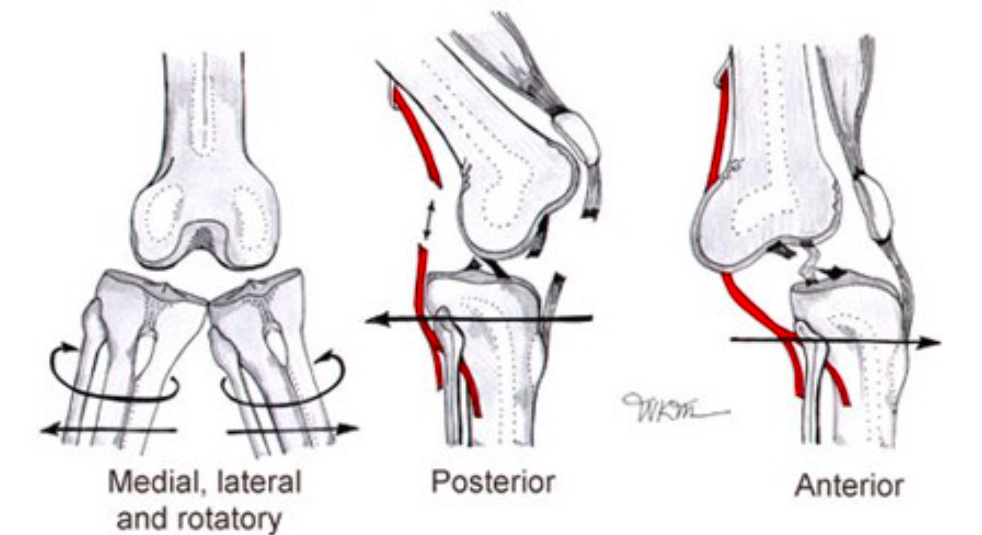
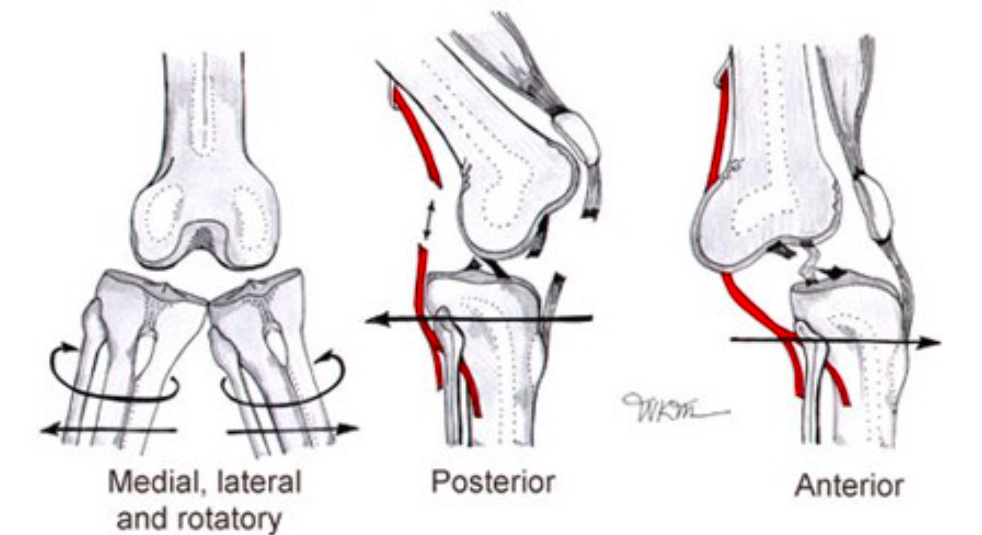
Knee Dislocation Classification System
- Tibiofemoral dislocations are classified as open or closed, and by the displacement of the tibia with respect to the femur.
- Anterior (30-50%): Hyperextension injury that injures posterior structures (PCL) and drives the distal femur posterior to the proximal tibia.
- Posterior (25%): Axial blow to the flexed knee (dashboard injury) that displaces the tibia posterior to the femur (Taylor 1972)
- Lateral (13%): Varus force to the proximal tibia and carries the highest risk of peroneal nerve injury.
- Medial: valgus force to the proximal tibia. Rotatory – indirect rotational force, usually caused by the body rotating in the opposite direction of a planted foot (Taylor 1972)
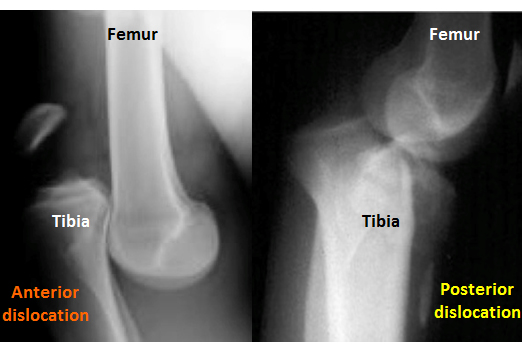
X-Ray: Anterior + Posterior Dislocations (www.bleacherreport.com)
X-Ray Findings
- Knee dislocation:
- In addition to dislocation, look for:
- An asymmetric or irregular joint space
- Osteochondral defects or avulsion fractures (Segond sign – lateral tibial condyle avulsion fracture, associated with ACL tears) (Shearer, 2010)
- Note that x-ray may appear normal if spontaneously reduced
- In addition to dislocation, look for:
- Patellar dislocation: Knee AP, lateral and axial (sunrise) views can be helpful to assess for patellar dislocation and fracture
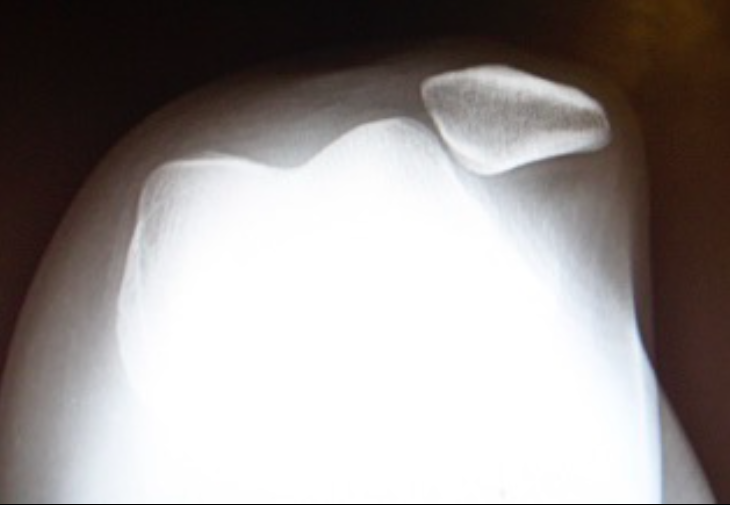
X-Ray Sunrise View Showing Patella Dislocation (drhem.wordpress.com)
Emergency Department Management
- General Principles
- Knee dislocations often involve high-energy mechanisms. Always evaluate the patient for concomitant injuries
- Only patients with bilateral strong peripheral pulses should undergo pre-reduction imaging, reduction of suspected knee dislocation should not be delayed if there is any sign of vascular impairment (Seroyer, 2008)
- Do not assume the spontaneously reduced injury was the patella and not the knee
- Knee Joint Reduction (see video below)
- Apply longitudinal traction to the tibia (this may be all that is required with severe ligament damage)
- If traction is not successful, the next step is to reverse the direction of the dislocation.
- Anterior dislocation: lift the distal femur and push the tibia posteriorly.
- Posterior dislocation: place pressure over the distal femur and lift the tibia anteriorly.
- Rotatory dislocations: rotate the tibia back towards its natural position.
- Post-reduction Care
- Check popliteal artery, DP + PT pulses
- Obtain emergent vascular surgery consultation if pulses are weak/absent, or if there are hard signs of an ischemic limb or vascular injury (diminished or absent pulses, pale or dusky skin, paresthesias, paralysis)
- Obtain ankle-brachial index (ABI) and/or bedside duplex ultrasound screen
- ABI>0.9, distal pulses are strong, and normal duplex: immobilize the knee and admit for observation and serial vascular examinations.
- ABI<0.9, pulses are asymmetric, or if the duplex is abnormal: obtain an urgent arteriogram or CTA in consultation with vascular surgery
- Patellar Dislocation
- Lie the patient supine with hips flexed to relax the quadriceps.
- Slowly extend the knee while applying gentle and gradual medial pressure to the lateral aspect of the dislocated patella, allowing it to “pop” back into place
- Post-reduction Care
- AP, lateral, and patellar (“sunrise” view) knee radiographs should be obtained after the reduction to assess for fracture or avulsion
- Disposition: weight bearing as tolerated with crutches if needed. No knee immoblizer or splint required.
This video has been shortened for quicker review of the procedure. This patient's knee was dislocated during a motor vehicle accident. In this video the reduction of the dislocated knee is demonstrated.
Complications
- Knee Dislocation
- Vascular Injury
- Popliteal artery injury is the most dangerous complication with potential for downstream limb ischemia
- 5-15% of patients with knee dislocations will have a vascular injury
- 40-50% of patients with anterior/posterior dislocations will have a popliteal artery injury, due to tethering of the artery at the popliteal fossa. (Kaufman, 1992)
- Ischemia time >8 hours has amputation rates as high as 86% (Kaufman, 1992)
- Vascular Injury
Knee Dislocations (www.emedicinehealth.com)
- Common peroneal nerve injury occurs in 25% of cases [3]
- Fractures are present in 60% of knee dislocations with tibia and femur most common
- Stiffness (arthrofibrosis) as well as laxity and instability are the most common complications
- Patellar Dislocation
- Patients are at risk of ligamentous damage and ligamentous laxity which can lead to future patellar dislocations as well as patellar subluxation
- Subluxation is a partial dislocation in which the patella attempts to dislocate but does not do so completely. The patient feels a buckling or a sense of giving way. These patients should be referred to a sports medicine specialist for rehabilitation
Take Home Points
- Knee dislocations are commonly complicated by popliteal artery injury. This limb-threatening complication MUST be recognized early to reduce morbidity
- 50% of knee dislocations will spontaneously reduce before ED arrival. Suspect dislocation in patients with significant joint swelling and laxity
- Knee reduction should not be delayed for imaging due to the risk for arterial injury
- After reduction, always check ABIs or duplex ultrasound. Consult vascular surgery early if there is suspicion for an arterial injury.
References
Brown A, Cadogan M. (2006).Patellar Dislocation. Emergency Medicine: Emergency and Acute Medicine: Diagnosis and Management. pp. 307. London: Hodder Arnold
Girgis FG et al. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop. 1975 Jan-Feb. (106):216-31. PMID: 1126079
Kaufman SL, Martin LG. Arterial injuries associated with complete dislocation of the knee. Radiology. 1992 Jul. 184(1):153-5. PMID:1609074
Kennedy JC. Complete Dislocation of the Knee Joint. J Bone Joint Surg. 1963; 45(5):889-904. PMID:1921923
Manske R. Multiple Ligament Knee Injury: Complications, N Am J Sports Phys Ther. 2008; 3(4): 226-233, PMID:2953344
Shearer D et al. Dislocation of the knee: imaging findings. J Spec Oper Med. 2010; 10(1):43-7. PMID:20306414
Seroyer ST et al. Management of the acute knee dislocation: The Pittsburgh experience. Injury. 2008; 39(7):710-8. PMID:18472101
Taylor AR et al. Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br. 1972; 54(1):96-102. PMID:2642548