Background: Acute severe asthma or status asthmaticus refers to an episode of bronchoconstriction that is unresponsive to standard management. Patients with acute severe asthma will present with significant respiratory distress and it is critical to rapidly treat them to avoid significant morbidity and mortality. Patients will present with tachypnea, retractions, diaphoresis, ability to only speak 1-2 words at a time, abdominal breathing, cold extremeties. and wheezing (although the most severe may have a “quiet chest” indicating the absence of any significant air entry).
Immediate Management:
There are three main goals of immediate management of the severe asthma exacerbation:
- Stave off intubation while your medications have time to act. Intubation is associated with increased morbidity and mortality.
- Maximize pre-intubation parameters in case the patient doesn’t turn around and intubation is required.
- Reverse bronchoconstriction to decrease work of breathing and prevent respiratory failure from exhaustion of respiratory muscles.
Basics: ABCs, IV, supplemental O2. Patient should be provided with all of the therapies used in mild to moderate asthma exacerbations but will require more aggressive management
Oxygenation + Respiratory Support
- Hypoxia only occurs late in a patient with a severe asthma exacerbation. Do not wait for hypoxia before supplying supplemental O2.
- Standard Nasal Cannula – Turn up to 15-20 L/min
- High-Flow Nasal Cannula (HFNC)
- Allows for increased flow (40-60L/min of humidified O2
- May be difficult to administer nebulizer treatments via facemask does not fit over HFNC
- Non-Rebreather with Beta-Agnoist Reservoir
- Non-invasive Positive Pressure Ventilation (NIPPV)
- Decreases work of breathing and improves gas exchange
- The evidence demonstrating a benefit to NIPPV is limited but available studies do not show substantial adverse events (Pollack 1995, Soroksky 2003, Lim 2012). These studies did not include the sickest subset of patients with asthma
- Bilevel Positive Airway Pressure (BPAP) preferred over Continuous Positive Airway Pressure (CPAP)
- Difference in inspiratory (IPAP) and expiratory (EPAP) pressure aids in increasing tidal volume delivered
- Start at IPAP 10 mm Hg, EPAP 5 mm Hg (or less) and titrate IPAP up (Typically no need to increase EPAP).
Intravenous Fluids
- Patients with severe asthma exacerbations have enormous insensible losses from increased respirations and work of breathing.
- Lung hyperinflation decreases pulmonary venous return, which can lead to hypotension. This is exacerbated by mechanical ventilation as the patient converts from negative pressure ventilation to positive pressure ventilation thus increasing intrathoracic pressure which can further decrease venous return.
- Aggressive IV fluids (30 cc/kg) should be given early to replete intravascular volume.
Epinephrine
- Epinephrine is a non-selective beta agonist that causes bronchodilation, vasoconstriction, increased cardiac contractility and increased heart rate
- Patients with severe asthma may have minimal benefit from inhaled beta agonists (i.e. albuterol) due to severe bronchoconstriction limiting delivery of medication to distal bronchioles.
- Intramuscular (IM) / Subcutaneous(SQ) Epinephrine
- Dose: 300-500 mcg
- Limited evidence demonstrates minimal significant side effects at this dose (Cydulka 1988)
- Intravenous (or Intraosseous) Epinephrine
- More rapidly reaches target tissue than IM/SQ especially if patient hypotensive
- Has effect of bronchodilation as well as vasoconstriction, which can reduce airway edema (Grandordy 1995)
- Dose: 1 – 5 mcg/min and titrate to effect
- Multiple retrospective studies demonstrate minimal adverse events with IV epinephrine (Smith 2003, Putland 2006)
- Contraindications: Epinephrine can theoretically cause uterine vasoconstriction and should be used with caution in pregnant patients.
- Terbutaline
- Selective, parenteral beta 2 agonist that causes bronchodilation without effecting heart rate or cardiac output
- Subcutaneous (SC) Terbutaline: 0.5 mg SC every 4 hours
Magnesium
- Mechanism: Bronchial smooth muscle relaxation
- Impact:
- Modest decrease in hospital admission rate in patients refractory to standard management (Levy 2014). However, the sickest subset of patients were excluded from this study
- The 3Mg trial (Goodacre 2013) demonstrated only a weak benefit to IV Magnesium in severe asthma however, this study did not include patients with life-threatening asthma.
- In the absence of robust evidence, it is reasonable to administer magnesium to severe asthma exacerbations as there are minimal side effects of the drug and a potential for benefit
- Dose: The dose in severe asthma is not established. 2 g IV over 15 minutes is a reasonable first dose and this may be repeated
Heliox
- Mechanism: Improved laminar flow of inhaled has which may allow better airflow through the constricted airways; allows better gas exchange and transport of medications to flow down to distal airways and alveoli
- A mixture of helium and oxygen(multiple possible rations – 60:40, 70:30, 80:20). Only give the minimum FiO2 necessary to achieve goal O2 saturation
- Evidence of utility limited but has not been extensively studied in the sickest subset of asthmatic patients and may still be beneficial in this group.
- Heliox may be used both via NIPPV and mechanical ventilator
- Limitation: If patient markedly hypoxic, may not give an adequate amount of FiO2.
Intubation
- Only about 2% of asthma exacerbations require intubation with 10-30% of those admitted to the ICU requiring invasive ventilation (Rosen’s 2014)
- Intubation is an inherently dangerous intervention in asthma because it does not fix the underlying problem (bronchoconstriction) and can cause dynamic hyperinflation (see below under ventilation), and rapid acidosis if respiration is not matched during RSI or post-intubation
- There is no specific vital sign, lab value or other diagnostic test result, which determines the necessity for intubation. The decision to intubate is based on a number of factors including the patients overall appearance, work of breathing, perceived ability to maintain their effort of breathing, mental status etc.
- Prior to intubation, be sure to maximize pre-oxygenation and intravascular volume
- Delayed Sequence Intubation (RSI)
- Procedural sedation (with dissociative dose ketamine) for the procedure of pre-oxygenation
- Useful in patients who have significant hypoxia/hypercarbia despite resuscitation and do not tolerate NIPPV to aid in pre-oxygenation
- See the EMCrit website for full details on the procedure
- Rapid Sequence Intubation (RSI) Medications
- There is no optimal set of agents for RSI in the severe asthmatic
- Ketamine
- Preferred agent because it is relatively hemodynamically stable and it has bronchodilatory properties.
- Dose: 1-2 mg/kg
- Paralytic
- Common options are rocuronium and succinylcholine
- Rocuronium offers the advantage of longer paralysis which avoids vent asynchrony early in management
Mechanical Ventilation
- Appropriate mechanical ventilation relies on ensuring that the patient has an adequate time to fully expire the delivered breath and avoid hyperinflation
- Permissive Hypercapnea: Decreasing respiratory rate and allowing PaCO2 to rise to supranormal levels.
- This strategy avoids breath stacking which leads to hyperinflation
- Hyperinflation leads to increased airway pressures and can lead the development of a tension pneumothorax
- Hyperinflation can also lead to marked decrease in venous return leading to decreased cardiac output and cardiac arrest
- Hyperinflation leads to increased pulmonary vascular resistance and right ventricular dysfunction
- Post-intubation meds (A full discussion of post-intubation care will appear in a future post)
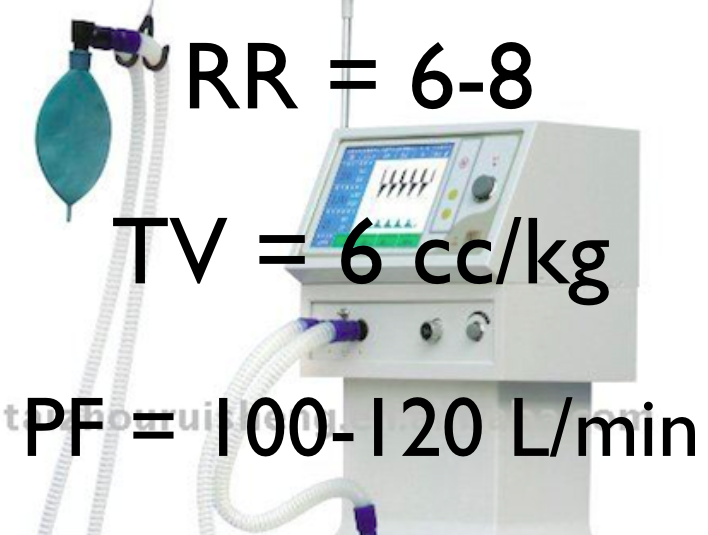
- Initial Ventilator Settings
- RR: 6-10 breaths/min
- VT: 6-8 ml/kg (ideal body weight
- PEEP: 0-5 cm H2O
- FiO2: Minimum necessary to maintain O2 sat > 93%
- Inspiratory Flow Rate: (suggest 100-120 L/min)
- Check Plateau Pressures and maintain at < 30 mm Hg
- Plateau pressure reflects the pressure experienced by alveoli
- Maintaining Pplat < 30 mm Hg helps to avoid alveolar damage
- If plateau pressure is > 30 mm Hg, consider lowering the RR and VT.
Mechanical ventilation does not fix the underlying bronchoconstriction. Be sure to continue maximal medical management.
Trouble Shooting the Ventilator
- Hemodynamic instability and hypoxia after intubation and mechanical ventilation are common and life-threatening. Rapid recognition of the underlying problem and treatment are critical
- DOPES Mnemonic – describes the most common causes of instability
- Displacement of the endotracheal tube (ETT)
- Direct visualization with laryngoscope preferred (US confirmation another option)
- Obstruction of the endotracheal tube
- Pass ETT suction catheter
- Pneumothorax (tension)
- Lung POCUS for lung sliding
- Empiric needle decompression or finger thoracostomy
- Equipment failure
- Disconnect the vent and deliver manual BVM breaths
- Stacked Breaths
- Forcibly exhale patient (gently push down on anterior chest wall with two hands until no further exhalation detected)
- Displacement of the endotracheal tube (ETT)
Trouble Shooting – Severe Acidemia
- A pH < 7.15 can lead to physiologic issues
- Check plateau pressure and if < 30 mm Hg, consider increasing ventilation (increase RR/TV)
- Invasive Treatment
- Inhaled Anesthetics (i.e. sevoflourane)
- Veno-Venous (VV) ECMO
Take Home Points
- Consider parenteral epinephrine in patients with severe asthma exacerbations as inhaled beta agonists are unlikely to penetrate into the distal airways.
- Intravenous epinephrine is life-saving and safe when used appropriately.
- Use NIPPV and high-flow nasal cannula to appropriately pre-oxygenate patients and avoid critical desaturations during intubation.
- Use a strategy of permissive hypercapnea for mechanical ventilation to avoid breath stacking, hyperinflation and high airway pressures. Aim for plateau pressures < 30 mm Hg.
- Use the DOPES mnemonic to troubleshoot hemodynamic instability after initiation of mechanical ventilation.
Read More:
EMCrit Podcast 15: The Severe Asthmatic
EMCrit Podcast 16: Coding Asthmatic, DOPES and Finger Thoracostomy
REBELCast: The Crashing Asthmatic
References:
Pollack CV et al. Treatment of acute bronchospasm with beta-adrenergic agonist aerosols delivered by a nasal bilevel positive airway pressure circuit. Ann Emerg Med 1995; 26(5): 552-7. PMID: 7486361
Soroksky A et al. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest 2003; 123: 1018-25. PMID: 12684289
Lim WJ et al. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev 2012. PMID: 23235608
Cydulka R et al. The use of epinephrine in the treatment of older adult asthmatics. Ann Emerg Med 1988; 17(4): 322-6. PMID: 3354935
Grandordy BM et al. The effect of intravenous phenylephrine on airway calibre in asthma. Eur Respir J. 1995;8:624-631. PMID: 7664864
Smith D et al. Intravenous epinephrine in life-threatening asthma. Ann Emerg Med 2003; 41(5): 706-711. PMID: 12712039
Putland M et al. Adverse events associated with the use of intravenous epinephrine in emergency department patients presenting with severe asthma. Ann Emerg Med 2006; 47(6): 559-564. PMID: 16713785
Levy Z, Slesinger TL. Does intravenous magnesium reduce the need for hospital admission among adult patients with acute asthma exacerbations. Ann Emerg Med 2014. PMID: 25128007
Goodacre S et al. Intravenous or nebulized magnesium sulphate versus standard therapy for severe acute asthma (3Mg trial): a double-blind, randomised controlled trial. Lancet Respir Med 2013; 1: 293-300. PMID: 24731521
Nowak RM, Tokarski GF: Asthma in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 73: p 941-58


Its a simplified and point to point presentation. Thanks
Being a paramedic educator, my scope of care concerns are limited, but I read at the, “Oxygenation + Respiratory Support” section the following:
“Standard Nasal Cannula – Turn up to 15-20 L/min”
Could this be a mistake? Perhaps a “standard nasal cannula” is different from the prehopsital environment, but our maximum liter flow is 6 L/min.
Thanks for the great article
Jay, for pre-ox, we recommend using a standard NC and cranking the O2 up until the little ball is popping of the top. This is what Levitan and Weingart stressed in their article in Ann of EM on pre-oxygenation. If your flow is limited to 6L/min, you won’t be able to do this. Hope that helps.
Good morning
I am curious as to your thoughts on nebuliser epinephrine at 5mg doses for severe asthma. Would this be beneficial from a topical beta effect or are we looking at a systemic defect via IM/IV doses?
We also uses Hydrocortisone to assist with stability. What are your thoughts here as well please?
Paul – interesting questions. I’ve looked at using neb epi but not too excited by it and have seen great effects. It seems to be more useful in large airway disease but not in small airway disease.
Not sure what you mean by “hydrocortisone to assist with stability.” Do you mean in HD unstable patients?
Hi Swami,
It appears Epinephrine is falling out of favor with a lot of national advisory groups, even in extremis. Are you aware of any more recent literature supporting its use?
Thankyou!
Nothing that I’ve seen but the drug has been life-saving in a small number of cases I’ve seen. I’m gonna keep it in my algorithm for the time being.
Terbutaline? http://blog.clinicalmonster.com/2017/03/its-weezy-baby/
Kings – agree that terbutaline can be used. I don’t mention it because I haven’t used in years, it’s not commonly stocked in my ED and always easier to get epi.
Hi there! I’m an RN and trying to figure out why “Hypoxia only occurs late in a patient with a severe asthma exacerbation.” Can anyone help me understand this? Probably something simple that I’m just not catching. 🙂
Thanks for the excellent review. Just noted a minor typo, the unit for plateau pressure should be 30 cm H20.