Definitions:
- Accidental hypothermia: An involuntary drop in core body temperature to <35°C (95°F)
- Primary hypothermia: Simple environmental exposure, when heat production in an otherwise healthy person is overcome by the stress of excessive cold
- Secondary hypothermia: Impaired thermoregulation, much more common in urban ED
- Can occur in ill persons with a wide variety of medical conditions, even in a warm environment (Baumgartner 2008, PMID: 19099327)
| Category | Causes |
| Increased heat loss | Burns, iatrogenic |
| Impaired thermogenesis | Impaired shivering, old or young age, exhaustion, malnutrition, |
| Medications/Toxins | Alcohol, anesthetics, opiates, sedatives, vasodilators |
| Metabolic/Endocrine | ketoacidosis, hypothyroidism, adrenal crisis, hypoglycemia |
| Neurologic | Space occupying lesion, stroke, spinal cord lesion, neuromuscular disorders |
| Multifactorial | Sepsis, shock, trauma |
Table 1: Secondary Hypothermia (Adapted from Tintinalli, 2016)
Epidemiology:
- During 2006–2010 exposure to excessive natural cold, hypothermia, or both was cited for 6,660 deaths (Berko 2006, PMID: 25073563)
Predisposing factors
- Subpopulations at risk for cold-related morbidity (Berko 2006, PMID: 25073563)
- Extremes of age (elderly, infants)
- Ethanol use
- Lack of shelter (homeless persons)
- Exposure (winter sports)
- Underlying illness
Classification:
- Modified staging system combines Swiss and classic symptoms as described in table 2
- NB: Temperatures do not always correspond to clinical symptoms
| Stage | Clinical Symptoms | Temp | Treatment |
| HTI | Conscious, shivering | 35-32C | Passive external |
| HTII | Impaired conscious, not shivering | 32-28C | Active external, minimally invasive |
| HTIII | Unconscious with VS | 28-24C | As above + airway, invasive only if cardiac instability |
| HTIV | No vital signs | <24C | CPR (3 rounds epi +/- defib), ECMO/CPB, if no ECMO thoracic/peritoneal lavage |
Table 2 (Brugger 2013, PMID: 23123559)
Presentation: A patient will be cool to touch or have vitals <35 C at triage, can be found in setting of multiple other presentations
Diagnostics: Assessing core temperature
- Conventional thermometers (oral, infrared, aural) are not reliable for hypothermia
- In an intubated patient, insertion of a thermistor probe in the lower third of the esophagus is one method
- Bladder probe
- The bladder temperature may be falsely elevated during peritoneal lavage.
- Rectal probes should be inserted to a depth of 15 cm
- Readings may lag behind core temperature during rewarming
ECG (Vassallo 1999, PMID: 10569384)
- Most common abnormality is prolongation of PR/QRS/QT intervals
- Most common dysrhythmia is atrial fibrillation
- Shivering produces mechanical artifact in baseline
- Osborn wave: A deflection occurring at the junction of the QRS and ST segment is invariably present in patients with temperatures <86°F (<30°C)
- Size of J-point deflection related to temperature decrease
- Not prognostically significant
- Cardiac arrest due to VT, VF or asystole
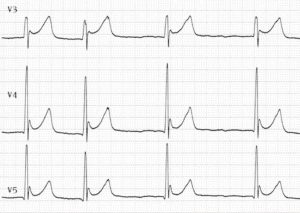
J-waves in moderate hypothermia (Image: https://litfl.com/hypothermia-ecg-library/)
Management:
- Prehospital
- Check pulse for 60 seconds
- Start CPR unless hard contraindication (frozen solid, decapitation, etc).
- Muscular rigidity and fixed pupils are not hard contraindications as may be present in reversible hypothermia
- Transport to ECMO facility if meets criteria (temp <32, no confirmed arrest before cooling, K <12) (Brugger 2013, PMID: 23123559)
- Limit patient activity and stimulation during the acute rewarming period
- Activity may increase myocardial oxygen demand or alter myocardial temperature gradients → increases the risk of iatrogenic ventricular fibrillation (Vassallo, 2015)
ABCs
- Airway: Do not delay intubation when it is indicated.
- Breathing: Do not correct blood gas for temperature as blood gas machine automatically rewarms blood, interpret as if patient normothermic to guide ventilation management, whether spontaneously breathing or mechanically ventilated. (Delaney 1989, PMID: 2642674; Woehrle 2018, PMID: 30377738)
- Circulation:
- When hypotension occurs in a patient with hypothermia, it may be a result of the presence of bradycardia and volume depletion; however, hypotension may be a predictor of infection, particularly when associated with a slow rewarming rate (Vassallo, 2015)
- Rewarming as management of circulation
- Passive external: Involves covering the patient with blankets and protecting the patient from further heat loss
- Uses the patient’s own endogenous heat production for rewarming and is most successful in healthy patients with mild to moderate hypothermia whose capacity for endogenous heat production is intact (Harnett 1983, PMID: 6349606)
- Active External: Bair hugger or other forced air surface rewarming device
- Hypothetical concern for suppressing shivering mechanism and peripheral vasodilation causing hypotension and worsening demand on cold myocardium
- Has not been replicated in animal studies. Remains controversial even though there is no evidence to support these concerns (Golden 1981)
- Recent literature supports forced air surface rewarming has a safe and effective method with no arrhythmia or aftedrop detected (Koller 1997, PMID: 9422306; Kornberger 1999, PMID: 10488932)
- Hypothetical concern for suppressing shivering mechanism and peripheral vasodilation causing hypotension and worsening demand on cold myocardium
- Minimally invasive active internal rewarming
- IV fluids: Normal Saline should be given to expand intravascular volume. Urine output is an important indicator of organ perfusion and the adequacy of intravascular volume in hypothermic patients, although the initial cold diuresis may lead to underestimation of fluid needs (Vassallo 2015; Wong 1983, PMID 6837026)
- Cold diuresis: Occurs when increases in central blood volume result in inhibition of the release of antidiuretic hormone, results in large volume dilute urine (Vassallo 2015, Hamlet 1983)
- Warmed saline has not been shown to speed rewarming but is theorized to prevent further iatrogenic heat loss, thus preferable but not essential to resuscitation
- Warm humidified oxygen, delivered by face mask or endotracheal tube (Hayward 1976, PMID: 1180782)
- IV fluids: Normal Saline should be given to expand intravascular volume. Urine output is an important indicator of organ perfusion and the adequacy of intravascular volume in hypothermic patients, although the initial cold diuresis may lead to underestimation of fluid needs (Vassallo 2015; Wong 1983, PMID 6837026)
- Invasive internal circulation management: Central rewarming devices (Zoll, Alsius), thoracic/peritoneal/bladder lavage, extracorporeal membrane oxygenation (ECMO) or cardiopulmonary bypass (CPB)
- Central rewarming devices
- Newer generation devices that have both a triple lumen function and a large volume infuser with a temperature control system
- Newer generation devices may reverse trauma associated coagulopathy (Taylor 2007, PMID: 18382749)
- If a central venous catheter is considered necessary, it should not be allowed to touch the endocardium (Truscott 1973, PMID: 4686525)
- Body cavity lavage: Form of active internal rewarming, suggested use for cardiac instability (VT/VF, cardiac arrest if ECMO/CPB or transfer to center with ECMO/CPB are not available)
- Thoracic lavage
- Peritoneal lavage with warmed dialysate
- ECMO or cardiopulmonary bypass should be considered for patients with severe hypothermia and subsequent cardiac instability (Truhlář 2015, PMID: 26477412)
- Central rewarming devices
- Passive external: Involves covering the patient with blankets and protecting the patient from further heat loss
| Technique | Rewarming rate (C/hr) | Indication |
| Warm environment, movement | 2 | HT I |
| Active external/minimally invasive (bair hugger, fluids) | 0.1-3.4 | HT II or HT III stable |
| PD | 1-30 | uncertain |
| HD | 2-4 | uncertain |
| Thoracic lavage | 3 | HT IV unstable if no ECMO |
| VV ECMO | 4 | uncertain |
| VA ECMO | 6 | HT III unstable or HT IV |
| CPB | 9 | As above if no ECMO |
Table 3 Comment: studied in avalanche victims, rewarming rates can vary significantly in underlying illness (sepsis etc.), see discussion of rewarming in urban patient population (Brown 2012, PMID: 23150960)
- CPR
- When signs of life and vital signs are absent (stage HT IV), there is consensus that treatment with ECMO or CPB is safe and may be beneficial (Truhlář 2015, PMID: 26477412)
- ECMO/CPB: The rate of survival without neurologic impairment is 47% to 63% (Dunne 2014, PMID: 25043580; Ruttmann 2007, PMID: 17723804)
- Without ECMO/CPB: survival rate is less than 37% (Kornberger 1999, PMID: 10488932)
- VA ECMO typically utilized over VV ECMO as need for circulatory support in cardiac arrest
- If transport to facility with ECMO is not available:
- Continue CPR
- Thoracic, peritoneal lavage
- With ongoing CPR, once >32C and still asystole, cardiac arrest likely irreversible, terminate CPR – “not dead until warm and dead”
- Defibrillation and Pharmacological circulatory support (vasopressors, ACLS medications etc)
- The evidence for the efficacy of drugs in severe hypothermia is limited and based mainly on animal studies
- Administer up to 3 rounds of defibrillation and epinephrine in initial management
- Vasopressors may also increase the chances of successful defibrillation, but with a core temperature <30 C sinus rhythm can degrade back into VF. Given that defibrillation and epinephrine may induce myocardial injury, it is reasonable to withhold epinephrine, other CPR drugs and shocks until the patient has been warmed to a core temperature ≥30 C. (Truhlář 2015, PMID: 26477412)
- Once 30 C has been reached, the intervals between drug doses can be doubled when compared to normothermia (i.e. epinephrine every 6–10 min). As normothermia (≥35 C) is approached, use standard drug protocols. (Truhlář 2015, PMID: 26477412)
- Potassium
- In severely hypothermic patients, profound hyperkalemia (K >10 mEq/L) is associated with unsuccessful resuscitation (Schaller 1990, PMID: 2402043)
- To limit unnecessary ECMO or CPB in avalanche survivor, potassium cutoff of 8 mEq/L is listed by European Resuscitation Council Guidelines (Truhlář 2015, PMID: 26477412)
- Controversy regarding potassium above 8 mEq/L as upper limit for serum K, other authors suggest the following recommendation:
- If 10-12 consult ECMO team, less than 10 CPR continuing with rewarming and ECMO consultation (Brown 2012, PMID: 23150960)
- When signs of life and vital signs are absent (stage HT IV), there is consensus that treatment with ECMO or CPB is safe and may be beneficial (Truhlář 2015, PMID: 26477412)
Special situations
- Avalanche
- Do not perform CPR if all of the following are met: Burial time >35 minutes, asystolic, snow packed in airway (Brugger 2013, PMID: 23123559)
- Hypoxia preceded hypothermia and thus CPR not beneficial
- Drowning: Better outcome if cooled (cooler the water, the more likely the brain is protected before hypoxia occurred) and able to breathebefore arrest
- Immersion: Patient in cold water but able to breathe → cooled before arrest → better prognosis
- Submersion: Patient in cold water but immediately unable to breathe → hypoxia and arrest precedes protective effects of cooling → worse prognosis
- Do not perform CPR if all of the following are met: Burial time >35 minutes, asystolic, snow packed in airway (Brugger 2013, PMID: 23123559)
Controversial Topics:
- Rescue collapse: Circulatory collapse due to hypovolemia, cardiac arrhythmias triggered by interventions (e.g., movement of the patient or central venous catheterization), and further cooling
- Action: Take care when moving patient
- Afterdrop: Continued core cooling after rescue, documented in artificial cooling experiments
- With the use of active external and minimally invasive rewarming and concurrent esophageal temperature measurement, afterdrop has not been reported
- There is no evidence that it occurs in humans. In studies with core temperature below 82.4°F (<28°C), no patient experienced afterdrop during peripheral rewarming (Röggla 2002, PMID: 12212366)
Modifications to urban ED population (Delaney 2006, PMID: 16946289)
- Most patients in urban EDs are not skiing or falling through ice
- Unlike an exposed mountaineer, hypothermia in urban ED is more likely secondary in nature and related to impaired thermoregulation, inability to seek shelter
- Retrospective studies show that death is often due to severity of underlying disease, especially infection, rather than a numerical temperature
- Patient with underlying illness and secondary hypothermia often have lower rewarming rates [figure 1]
- Given high incidence of intoxication or underlying illness, especially infection, it is vital to identify underlying cause and treat (i.e. give antibiotics empirically)
- Does not apply to the patient with hemorrhage, when coagulopathy induced by hypothermia is an important contributor to morbidity
- Invasive devices or modalities could have a roll in trauma (Taylor 2007, PMID: 18382749)
- Does not apply to the patient with hemorrhage, when coagulopathy induced by hypothermia is an important contributor to morbidity
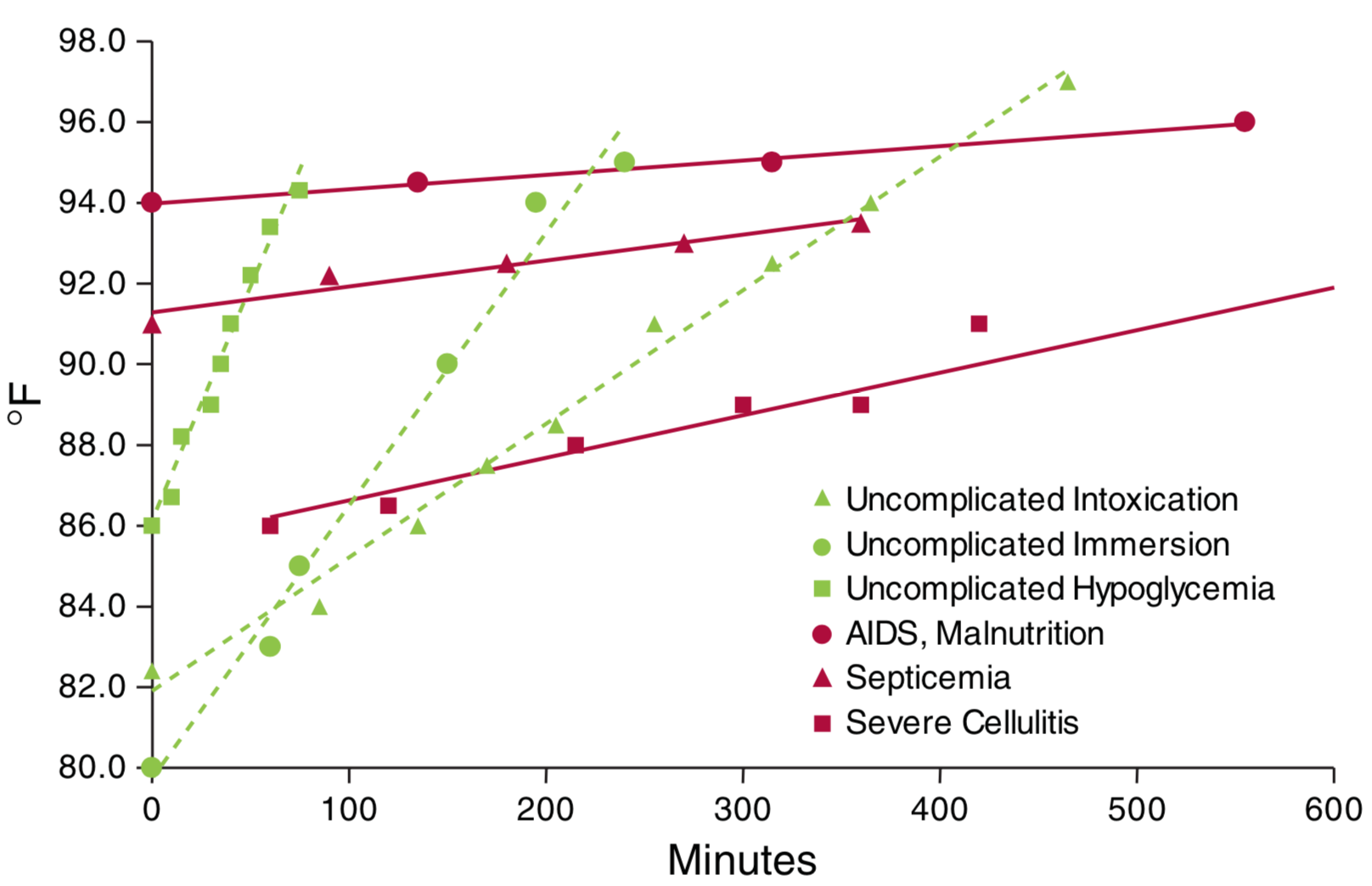
Figure 1: Relation of rewarming rate to underlying illness (Vassallo 2015)
Take Home Points
- Hypothermia is defined as core body temperature <35 C
- Primary hypothermia is purely due to exposure
- Secondary hypothermia associated with underlying condition causing impaired temperature regulation
- Always start with vital signs or no vital signs
- Basics: Remove wet clothing, warm drinks if able to take PO, provide warm dry insulating clothing, apply warming blanket, warm humidified O2, warm IVF for fluid resuscitation
- Reserve advanced invasive methodologies (ECMO, CPB, catheter rewarming, thoracic/bladder lavage) for absence of VS, instability (VF/VT/asystole), trauma
- ECMO is emerging as a possibly superior option for patients in cardiac arrest and patients with cardiac instability, many resuscitation guidelines suggest transfer to ECMO center if criteria met, otherwise internally invasive rewarming in addition to standard life support
- In urban settings hypothermia is often a reflection of underlying disease state, the rate of rewarming can reflect underlying pathology (i.e. inability of a sick patient to warm themselves); sepsis is an under-appreciated cause
REFERENCES
Baumgartner EA, Belson M, Rubin C, Patel M. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995–2004. Wilderness & environmental medicine. 2008 Dec 1;19(4):233-7. PMID: 19099327
Berko J, Ingram DD, Saha S, Parker JD. Deaths attributed to heat, cold, and other weather events in the United States, 2006–2010. PMID:25073563
Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. New England Journal of Medicine. 2012 Nov 15;367(20):1930-8. PMID:23150960
Brugger H, Durrer B, Elsensohn F, Paal P, Strapazzon G, Winterberger E, Zafren K, Boyd J. Resuscitation of avalanche victims: evidence-based guidelines of the international commission for mountain emergency medicine (ICAR MEDCOM): intended for physicians and other advanced life support personnel. Resuscitation. 2013 May 1;84(5):539-46. PMID: 23123559
Danzl DF, Pozos RS, Auerbach PS, Glazer S, Goetz W, Johnson E, Jui J, Lilja P, Marx JA, Miller J, Mills W. Multicenter hypothermia survey. Annals of emergency medicine. 1987 Sep 1;16(9):1042-55. PMID: 3631669
Delaney KA, Howland MA, Vassallo S, Goldfrank LR. Assessment of acid-base disturbances in hypothermia and their physiologic consequences. Annals of emergency medicine. 1989 Jan 1;18(1):72-82. PMID: 2642674
Dunne B, Christou E, Duff O, Merry C. Extracorporeal-assisted rewarming in the management of accidental deep hypothermic cardiac arrest: a systematic review of the literature. Heart, Lung and Circulation. 2014 Nov 1;23(11):1029-35. PMID: 25043580
Golden FS, Hervey GR. The “afterdrop” and death after rescue from immersion in cold water. Hypothermia ashore and afloat. 1981:37-56.
Hamlet MP: Fluid shifts in hypothermia. In: Pozos RS, Wittmers LE, eds.The Nature and Treatment of Hypothermia. Minneapolis: University of Minnesota Press; 1983:94–99.
Harnett RM, Pruitt JR, Sias FR. A review of the literature concerning resuscitation from hypothermia: Part II–Selected rewarming protocols. Aviation, space, and environmental medicine. 1983 Jun;54(6):487-95. PMID: 6349606
Hayward JS, Steinman AM. Treatment of accidental hypothermia: An experimental study of inhalation rewarming. 1976. PMID: 1180782
Koller R, Schnider TW, Neidhart P. Deep accidental hypothermia and cardiac arrest rewarming with forced air. Acta anaesthesiologica scandinavica. 1997 Nov;41(10):1359-64. PMID: 9422306
Kornberger E, Lindner KH, Mayr VD, Schwarz B, Rackwitz KS, Wenzel V, Krismer AC, Mair P. Effects of epinephrine in a pig model of hypothermic cardiac arrest and closed-chest cardiopulmonary resuscitation combined with active rewarming. Resuscitation. 2001 Sep 1;50(3):301-8. PMID: 11719160
Kornberger E, Schwarz B, Lindner KH, Mair P. Forced air surface rewarming in patients with severe accidental hypothermia. Resuscitation. 1999 Jul 1;41(2):105-11. PMID: 10488932
Krismer AC, Lindner KH, Kornberger R, Wenzel V, Mueller G, Hund W, Oroszy S, Lurie KG, Mair P. Cardiopulmonary resuscitation during severe hypothermia in pigs: does epinephrine or vasopressin increase coronary perfusion pressure?. Anesthesia & Analgesia. 2000 Jan 1;90(1):69-73. PMID: 10624981
Röggla M, Frossard M, Wagner A, Holzer M, Bur A, Röggla G. Severe accidental hypothermia with or without hemodynamic instability: rewarming without the use of extracorporeal circulation. Wiener klinische Wochenschrift. 2002 May;114(8-9):315-20. PMID: 12212366
Ruttmann E, Weissenbacher A, Ulmer H, Müller L, Höfer D, Kilo J, Rabl W, Schwarz B, Laufer G, Antretter H, Mair P. Prolonged extracorporeal membrane oxygenation-assisted support provides improved survival in hypothermic patients with cardiocirculatory arrest. The Journal of thoracic and cardiovascular surgery. 2007 Sep 1;134(3):594-600. PMID: 17723804
Schaller MD, Fischer AP, Perret CH. Hyperkalemia: a prognostic factor during acute severe hypothermia. Jama. 1990 Oct 10;264(14):1842-5. PMID: 2402043
Stoner J, Martin G, O’Mara K, Ehlers J, Tomlanovich M. Amiodarone and bretylium in the treatment of hypothermic ventricular fibrillation in a canine model. Academic emergency medicine. 2003 Mar;10(3):187-91. PMID: 12615580
Taylor EE, Carroll JP, Lovitt MA, Petrey LB, Gray PE, Mastropieri CJ, Foreman ML. Active intravascular rewarming for hypothermia associated with traumatic injury: early experience with a new technique. InBaylor University Medical Center Proceedings 2007 Apr 1 (Vol. 20, No. 2, pp. 2-8). Taylor & Francis. PMID: 18382749
Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Meckler GD, Yealy DM. Tintinalli’s emergency medicine : a comprehensive study guide. Eight edition. ed. New York: McGraw-Hill Education; 2016.
Truhlář A, Deakin CD, Soar J, Khalifa GE, Alfonzo A, Bierens JJ, Brattebø G, Brugger H, Dunning J, Hunyadi-Antičević S, Koster RW. European Resuscitation Council Guidelines for Resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation. 2015 Oct;95:148. PMID: 26477412
Truscott DG, Firor WB, Clein LJ. Accidental profound hypothermia: successful resuscitation by core rewarming and assisted circulation. Archives of Surgery. 1973 Feb 1;106(2):216-8. PMID: 4686525
Vassallo SU, Delaney KA, Hoffman RS, Slater W, Goldfrank LR. A prospective evaluation of the electrocardiographic manifestations of hypothermia. Academic emergency medicine. 1999 Nov;6(11):1121-6. PMID: 10569384
Vassallo SU, Delaney KA. Thermoregulatory Principles. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e New York, NY: McGraw-Hill; 2015.
Woehrle T, Lichtenauer U, Bayer A, Brunner S, Angstwurm M, Schäfer ST, Baschnegger H. Misleading symptoms and successful noninvasive rewarming of a patient with severe hypothermia (23.1° C). Der Anaesthesist. 2018 Dec 1;67(12):931-5. PMID: 30377738
Wong KC. Physiology and pharmacology of hypothermia. Western Journal of Medicine. 1983 Feb;138(2):227.PMID: 6837026
