Definition: A hyperglycemic, acidotic state caused by insulin deficiency. The disease state consists of 3 parameters:
- Hyperglycemia (glucose > 250 mg/dl)
- Acidosis
- Ketosis
Epidemiology
- Incidence of ~ 10,000 cases/year in US
- Mortality rate: 2-5% (prior to insulin was 100%) (Lebovitz 1995)
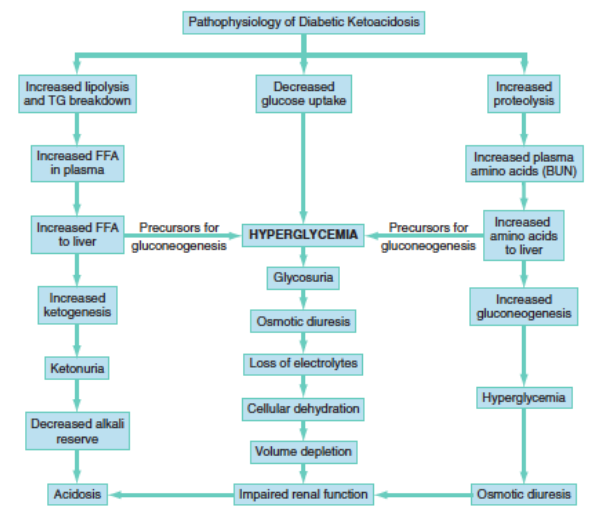
DKA Cycle – Rosen’s
Pathophysiology
- Insulin deficiency leads to serum glucose rise
- Increased glucose load in kidney leads to increased glucose in urine and osmotic diuresis
- Osmotic diuresis is accompanied by loss of electrolytes including sodium, magnesium, calcium and potassium
- Volume depletion leads to impaired glomerular filtration rate (GFR)
- Inability to properly metabolize glucose results in fatty acid breakdown with resultant ketone bodies (acetoacetate + beta-hydroxybutyrate)
Causes: An acute insult leads to decompensation of a chronic disease. Can also be first manifestation of new onset diabetes (particularly in children). Below are common triggers
- Infection (particularly sepsis)
- Myocardial ischemia or infarction
- Medication non-compliance
Clinical Presentation
- History
- Polydipsia, polyuria, polyphagia
- Weakness
- Weight loss
- Nausea/Vomiting
- Abdominal Pain
- Physical Examination
- Acetone odor on breath (“fruity” smell)
- Kussmaul’s respirations – deep fast breathing (tachypnea and hyperpnea)
- Tachycardia
- Hypotension
- Altered mental status
- Abdominal tenderness
Diagnostic Testing
- Definitive diagnosis is established by laboratory criteria as detailed above (hyperglycemia, ketosis and acidosis)
- Essential Diagnostic Tests
- Serum glucose
- Typically > 350 mg/dL
- Euglycemic DKA (< 300 mg/dL) reported in up to 18% of patients
- Blood gas
- Patients will exhibit an anion gap metabolic
- Electrolytes: hypo/hyper/normokalemia, hyponatremia
- Arterial or venous blood gas can be used (Savage 2011)
- Urinalysis
- Glucosuria
- Ketonuria
- Electrocardiogram (EKG)
- Typically will exhibit non-specific changes including sinus tachycardia
- Can see changes associated with hyperkalemia or hypokalemia
- Comprehensive Metabolic Panel
- Serum potassium
- Patients with DKA are total body potassium depleted
- Osmotic diuresis + vomiting lead to potassium loss
- Often depleted by 100’s of mEq
- Initial serum potassium can be elevated, normal or low
- Potassium elevation secondary to acidemia
- 5-10% of patients will present with hypokalemia (< 3.3 mEq/L) (Aurora 2012)
- Hyponatremia
- Total body depletion due to renal and gastrointestinal losses
- Dilutional hyponatremia caused by serum hyperglycemia causing fluid shift
- Correction factor: Add 1.6 mEq Na for every 100 mg/dL the glucose is above normal
- This is NOT pseudohyponatremia. The measured serum level is the concentration experienced by the body. However, as the serum glucose is corrected, fluid shifts will reverse and the Na will rise
- Do NOT use the corrected sodium to calculate the anion gap
- BUN/Cr
- Patients will often exhibit prerenal acute kidney injury
- BUN/Cr atio will be elevated reflecting intravascular volume depletion
- Serum ketones are typically unnecessary in the Emergency Department for the diagnosis and management of DKA. However, there may be uncommon situations where they can be beneficial.
- Additional tests should be guided by the clinical picture. Infection is an important precipitant to DKA and should be specifically sought when an alternate precipitant is not known.
- Patients with DKA are total body potassium depleted
- Serum potassium
- Serum glucose
Management
Basics: ABCs, IV, Cardiac Monitor and 12-lead EKG
- Establish at least 2 peripheral IVs as patients typically require multiple medication and infusions.
- Diligently search for the underlying cause
Initial Management
- Intravenous fluids
- Role
- Replenish intravascular depletion resulting from osmotic diuresis
- Correct decreased GFR
- Initial Dose: 20-30 cc/kg of crystalloid
- 9% NaCl (Normal Saline)
- Typical resuscitation fluid in DKA
- Problems
- NS is far from “normal”
- Large volume infusions can cause hyperchloremic metabolic acidosis (unclear impact on patient)
- In profoundly acidemic patients, avoidance of NS may be beneficial
- Lactated Ringers
- Closer to physiologic solution
- Does not cause hyperchloremic metabolic acidosis
- Other options: balanced solutions (i.e. Plasma-Lyte)
- Repeat fluid bolus as necessary to replete intravascular volume
- Electrolyte Disorder Correction
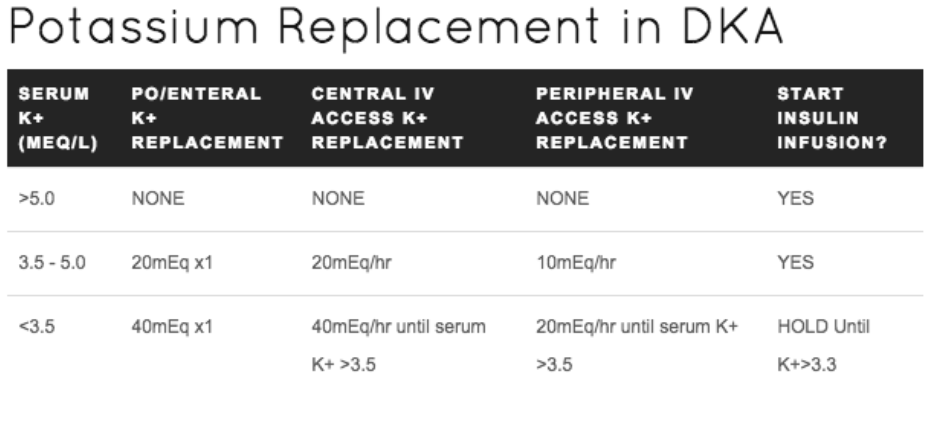
- Potassium – the most important lab value in DKA
- Aggressive repletion frequently necessary
- Patients often 100s of mEq depleted
- Many of DKA treatments (i.e. fluids, insulin) will decrease serum potassium level
- Supplementation (see hypokalemia post)
- Oral: KCl 40 mEq every hour
- Intravenous: KCl 10-40 mEq in each liter of fluid
- Insulin + Potassium
- Insulin infusion will shift potassium intracellularly and decrease serum level
- Basic guide to potassium replacement (courtesy of REBEL EM)
- Aggressive repletion frequently necessary
- Potassium – the most important lab value in DKA
- 9% NaCl (Normal Saline)
- Role
- Sodium
- Typically dilutional hyponatremia. Will correct without specific treatment
- Magnesium
- Hypokalemia = Hypomagnesemia (Boyd 1984)
- Both electrolytes lost during osmotic diuresis
- Cannot replete intracellular potassium without magnesium
- Serum magnesium level may not correlate with total body stores
- Dose: 1-2 gm MgSO4
- Hypokalemia = Hypomagnesemia (Boyd 1984)
- Phosphorous
- If PO4 < 1.0 mEq, consider repletion with KPO4
- Insulin therapy
- Ultimately, patients will require insulin repletion in order to reverse pathophysiology in DKA and stop ketosis
- Insulin should be held until the it is confirmed that the patient does not have severe hypokalemia to avoid resultant worsening hypokalemia with insulin infusion
- Dose
- Regular (Humalog/Novalog) insulin infusion 0.1 – 0.14 units/kg (Kitabchi 2008)
- Bolus regular insulin
- Unnecessary and potentially harmful
- No difference in change in serum glucose, closure of anion gap (Goyal 2010)
- Bolus insulin associated with increased hospital length of stay and hypoglycemic episodes (Goyal 2010)
- Bicarbonate for acidosis
- Guidelines recommend administration of bicarbonate if pH < 7.1 but existing evidence does not show benefit to this therapy (Morris 1986, Duhon 2013, Green 1998)
- In order for bicarbonate to increase serum pH, the patient must blow off CO2. Ventilatory rate must be artificially increased in order to accomplish this
- Potential deleterious effects
- Worsening hypokalemia and intracellular acidosis (Villon 1999)
- Inhibition of RBC oxygen release at tissue level
- Delay in improvement of ketosis (Okuda 1996)
- More on the role of bicarbonate from REBEL EM
Cerebral Edema
- Definition + Background
- Excess accumulation of intracellular and extracellular fluid in the brain
- Rare (< 1%) complication but high mortality (> 30%)
- More common in patients with newly diagnosed diabetes presenting with DKA
- Cause: it is unclear what causes patients to develop cerebral edema. Retrospective literature has shown association between initial bicarbonate levels, administration of bicarbonate, fluid administration etc but no causality has been shown.
- Signs + Symptoms
- Vomiting
- Headache
- Altered mental status or fluctuating mental status
- Focal neurologic deficits (CN III, IV or VI palsy common)
- Lethargy
- There are explicit diagnostic, major and minor criteria (Muir 2004)
- Management
- Nonpharmacologic
- Elevate head of bed to 30 degrees
- Decrease IV fluid infusion
- Pharmacologic
- Mannitol: 1 gm/kg over 20 minutes
- 3% Hypertonic saline: 5-10 ml/kg
- Nonpharmacologic
Continued Management
- Continuous Monitoring
- Vital Signs
- Urine output
- Serum glucose K+, Cl–, HCO3–, pH q1 hour until stable
- Insulin Infusion
- Continue until anion gap normalizes
- When serum glucose < 300 mg/dL add D5W/0.45%NS solution to avoid hypoglycemia
- Disposition: Patients should be admitted to highly monitored area
Take Home Points
- DKA is a common, life-threatening emergency but aggressive, comprehensive care markedly reduces morbidity and mortality
- DKA should be suspected and rapidly diagnosed in all patients with diabetes who present to the Emergency Department
- Severe hypokalemia is the most common cause of morbidity and mortality in patients with DKA. Hold insulin until the serum potassium is known and aggressively replete potassium and monitor serum concentrations
- Always search for the underlying cause of the patients DKA presentation keeping in mind that infection is the most common cause.
Read More
CanadiEM: Is NS the Coke of Crystalloid Fluid?
EMDocs.net: Myths in DKA Management
REBEL EM: Diabetic Ketoacidosis (DKA) Myths
Peds EM Morsels: Cerebral Edema and Diabetic Ketoacidosis
Cydulka RK, Maloney GE: Diabetes Mellitus and Disorders of Glucose Homeostasis; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 126: p 1652-1668.
References
Lebovitz HE: Diabetic ketoacidosis. Lancet 1995; 345: 767-772. PMID: 7891491
Savage MW et al. Joint British Diabetes Societies guideline for the management of diabetic ketoacidosis. Diabet Med. 2011; 28(5):508-15. PMID: 21255074
Aurora S et al. Prevalence of hypokalemia in ED patients with diabetic ketoacidosis. Am J Emerg Med 2012; 30: 481-4. PMID: 21316179
Boyd JC et al. Relationship of potassium and magnesium concentrations in serum to cardiac arrhythmias. Clin Chem 1984; 30(5): 754-7. PMID: 6713638
Kitabchi AE et al. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis? Diabetes Care. 2008;31(11):2081. PMID: 18694978
Goyal N et al. Utility of Initial Bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med 2010; 38(4): 422-7. PMID: 18514472
Morris LR et al. Bicarbonate therapy in severe diabetic ketoacidosis. Ann Intern Med. 1986;105(6):836. PMID: 3096181
Duhon B et al. Intravenous sodium bicarbonate therapy in severely acidotic diabetic ketoacidosis. Ann Pharmacother 2013; 47: 970-5. PMID: 23737516
Green SM et al. Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis. Ann Emergency Medicine 1998; 31: 41-48. PMID: 9437340
Villon A et al. Does bicarbonate therapy improve management of severe diabetic ketoacidosis? Crit Care Med 1999; 27: 2690-2693. PMID: 10628611
Okuda Y et al. Counterproductive effects of sodium bicarbonate in diabetic ketoacidosis. J Clinical Endocrinology Metabolism 1996; 81: 314-320. PMID: 8550770
Muir AB et al. Cerebral edema in childhood diabetic ketoacidosis: natural history, radiographic findings, and early identification. Diabetes Care 2004; 27(7):1541-6. PMID: 15220225

Awesome info!
How is the process of changing from IV insulin to subcutaneous insulin?
Thanks
Henrique – I’ll admit that I rarely do this in my place. Patients move to the ICU fairly quickly. Do you have a protocol you use?
in the ER where I work, once DKA is resolved, we start them on long acting insulin an hour before we shut off the insulin drip… then it becomes a sliding scale insulin administration set up with accuchecks q2hours.
Thanks, that was a great easy to understand guide to DKA
Thanks for a great easy to read article,
Should we confirm pt has a urine output before giving potassium