Definition: Acute bacterial infection of the bile ducts resulting from common bile duct obstruction. Also called ascending cholangitis. Mortality rate 5-10%
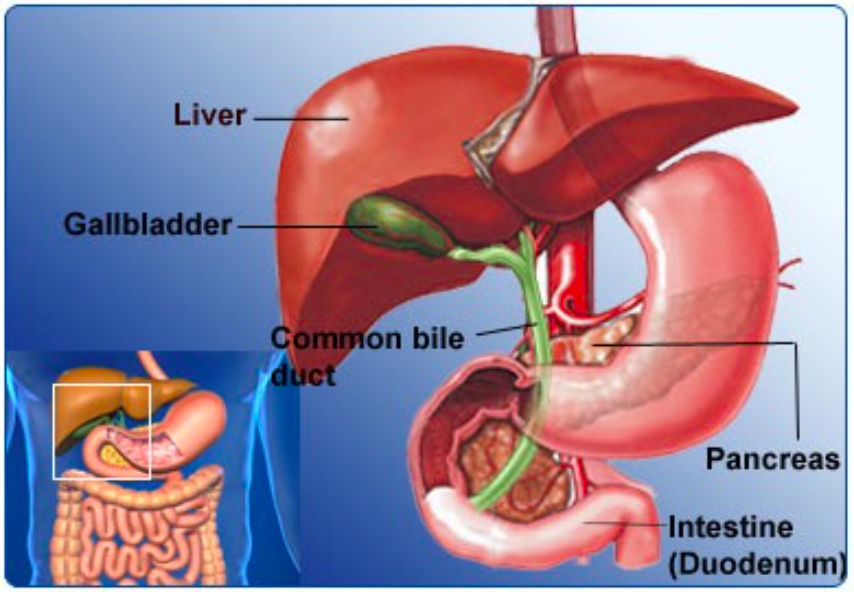
Hepatobiliary Tract Anatomy
Pathophysiology
- Bile duct develops an obstruction
- Obstruction may be incomplete (more common) or complete
- Causes: Gallstones (most common), malignancy, benign stricture, iatrogenic (i.e. ERCP), biliary parasites, primary sclerosing cholangitis (PSC)
- Elevated intraluminal pressure in the gallbladder leads to translocation of bacteria
- Bacteria may gain access via lymphatics, portal venous blood or retrograde from the duodenum
- Common pathogens: E. coli, Klebsiella, Streptococcus, Enterobacter, Pseudomonas Other causes: HIV/AIDS cholangiopathy, parasitic infections (Ascaris lumbricoides)
Presentation
- Charcot’s Triad: Fever, RUQ pain and jaundice (neither sensitive nor specific)
- Symptoms
- Fever/chills
- Nausea/vomiting
- Abdominal pain
- Physical Exam
- RUQ tenderness to palpation
- Peritoneal signs are variable
- Jaundice
- Frank sepsis (fever, tachycardia, hypotension, tachypnea) is a common presentation
- Reynold’s Pentad: Charcot’s triad + sepsis and AMS
Acute Cholangitis Infographic (mediconet.blogspot.com)
Diagnostics
- Cholangitis is a clinical diagnosis. There are no diagnostic tests that absolutely clinches or rules out the diagnosis.
- Laboratory Tests
- Lab tests are generally neither sensitive nor specific for ruling in or ruling out cholangitis. Below are common findings
- WBCs – usually elevated but may be depressed in severe infection
- Hepatic panel
- Elevated aminotransferases (i.e ALT/AST)
- Elevated alkaline phosphatase
- Hyperbilirubinemia
- Lipase – useful to evaluate for concomitant pancreatitis
- Blood gas may be useful in patients who appear septic to record lactate level
- Blood cultures
- Imaging
- Imaging is helpful in supporting the diagnosis and aids in identifying the cause. Many patients will have concomitant acute cholecystitis that will be identified on imaging
- Ultrasound (US)
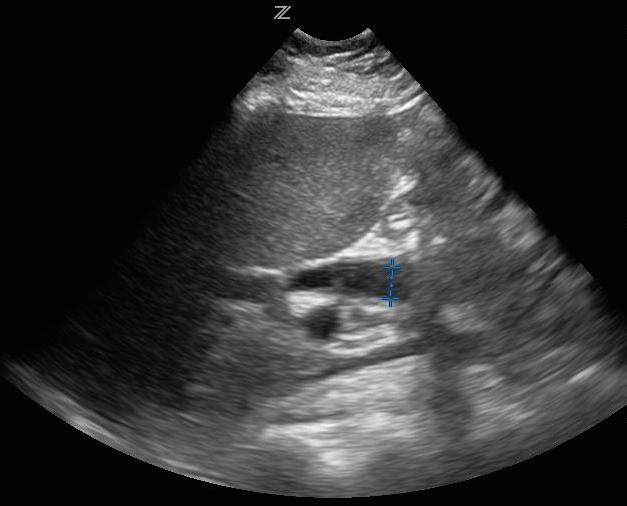
Ultrasound with Dilated Common Bile Duct (CBD)
- Common findings
- Intrahepatic biliary ductal dilation (see video below)
- Thickening of the bile duct walls
- Obstructing gallstones
- Concomitant cholecystitis findings
- 4 sonographic signs of cholecystitis: Gallstones, gallbladder wall thickening >3mm, pericholecystic fluid, sonographic murphy’s
- Gallstones + sonographic murphy’s
- Highly sensitive (87-95%) and specific (82%) when examining the gallbladder and biliary ducts (Carmody 2011, Summers 2010)
- Not highly sensitive for diagnosing choledocholithiasis: can miss distal CBD stones
- Useful to distinguish between intrahepatic and extrahepatic obstruction
- Common findings
- CT Scan
- Classic finding: non-homogenous liver enhancement during arterial phase
- Can identify dilated intra- and extrahepatic ducts
- Gallstones are poorly visualized
- Findings non-specific
- Can identify other pathologies or complications of cholangitis (perforation, abscess)
- Other Diagnostic Imaging
- Nuclear scintigraphy: may be more sensitive than US in identifying early obstruction
- Useful when ultrasound results are equivocal and the diagnosis is suspected
- Cannot visualize the biliary tree with complete obstruction
- Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Procedure is both diagnostic + potentially therapeutic
- Allows removal of obstructing stone, biopsy of mass, culture of bile and decompression or stent placement
- Magnetic resonance cholangiopancreatography (MRCP)
- Most sensitive noninvasive method
- Requires patient to be stable to obtain study
- Nuclear scintigraphy: may be more sensitive than US in identifying early obstruction
Immediate Management:
Basics:
- ABCs, IV, Cardiac Monitor
- Unstable patients due to sepsis or septic shock should be aggressively resuscitated per general sepsis/septic shock algorithms (IV fluids, airway management as necessary, vasoactive substances etc.)
Directed Management
- Broad spectrum antibiotics
- Antibiotics should cover gram positive, anaerobic gram negative aerobic andenteric organisms (see above)
- Common regimens
- Piperacillin/tazobactam (Zosyn®)
- Imipenem/Meropenem
- Ampicillin/sulbactam (Unasyn®) + metronidazole
- Correct electrolyte abnormalities and coagulopathies if present
- Biliary tract decompression
- Percutaneous drainage via interventional radiology
- ERCP via gastroenterology
- Should be performed emergently if the patient fails to improve with aggressive resuscitation
- In resuscitation responders, should be performed within 24 hours
- Surgical drainage
Disposition:
- All patients with cholangitis will require admission and many will require a high-resource setting (ICU or step down unit)
Take Home Points
- Cholangitis is a potentially life-threatening (mortality 5-10%), acute bacterial infection of the bile ducts
- Diagnosis is based on clinical findings and while imaging can be supportive, it is frequently non-diagnostic
- A normal ultrasound does not rule out acute cholangitis
- Treatment focuses on supportive care, broad spectrum antibiotics and consultation with a provider that can provide biliary tract decompression (IR, gastroenterology or general surgery)
Read More
Radiopaedia: Acute cholangitis
References
Oyama LC: Disorders of the liver and biliary tract, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 90: p 1186-1205.
Summers S et al. A Prospective Evaluation of Emergency Department Bedside Ultrasonography for the Detection of Acute Cholecystitis. Ann Emerg Med. 2010;56(2): 114-122. PMID: 20138397
Carmody KA, Moore CL, Feller-Kopman D, (eds). Handbook of Critical Care & Emergency Ultrasound. New York, NY: McGraw Hill, 2011, pp.123-144.
Richter J et al. Ultrasound in Tropical and Parasitic Diseases. Lancet 2003; 362:900-902. PMID: 13678978

Hi – awesome job with these reviews and podcasts! I really enjoy these quick and succinct summaries. I do have just a quick comment in regards to the antimicrobial regimens. Unasyn + Flagyl is essentially double covering anaerobes, which is not necessary. Additionally, Unasyn may not be the most appropriate empiric choice due to increasing resistance to E. coli. I tend to use Zosyn for suspected cholangitis empirically, which will adequately cover anaerobes and gram negatives, including pseudomonas (although this pathogen is uncommon).
Thanks!
Kellie – EM PharmD in Sarasota, FL