Definition: Noninvasive measurement of the concentration (partial pressure) of expired carbon dioxide over time.
The Basics
2 types of attachments:
- Mainstream – must be attached to the ventilator circuit
- In series with endotracheal intubation tube
- Side Stream detector – takes sample of expired gas
- Can be placed in parallel and can be used in non-intubated patients (e.g. with nasal cannula detector)
2 types of measurements:
- Colorimetric – qualitative measure (color change) of expired CO2 covering a wide range of values, therefore use is limited primarily to verify correct ETT placement
- Purple (<4 mmHg CO2) to Tan (4-15 mmHg CO2) to Yellow (20 mmHg CO2)
- Cannot exclude bronchial mainstem intubation
- Capnography – quantitative measurement of expired CO2
- Normal levels = 35 to 45 mmHg
- EtCO2 closely correlated with PaCO2– EtCO2 approximately 5 mmHg higher than PaCO2
- Normal EtCO2 – 35-45 mmHg
- Hypoventilation suspected if EtCO2 > 50 mmHg or increase greater than 10 mmHg from baseline
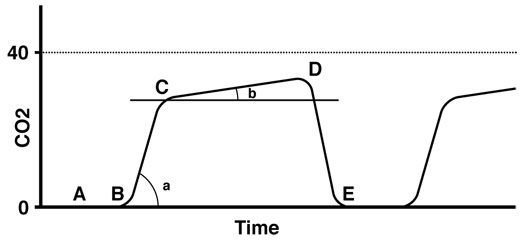
Capnography waveform (adapted from https://uichildrens.org/health-library/monitoring-devices-picu)
The Waveform
- Phase 1 [A-B] – Dead Space Ventilation
- Should contain no CO2
- Phase 2 [B-C] – Expiratory Upslope
- CO2 raises from alveoli into upper airway
- Phase 3 [C-D] – Alveolar Plateau
- Value at end of this phase (end-tidal) is that which is reported on monitor
- Provides insight into V/Q characteristics of lung
- Phase 4 [D-E] – Inspiratory Downslope
- Physiologic decline in CO2 partial pressure as patient’s inspire
Sample Abnormal Waveforms
- Obstructive Lung Disease – Increased baseline indicates there is some trapping of CO2 within the lungs while the same amount of CO2 is expired each breath
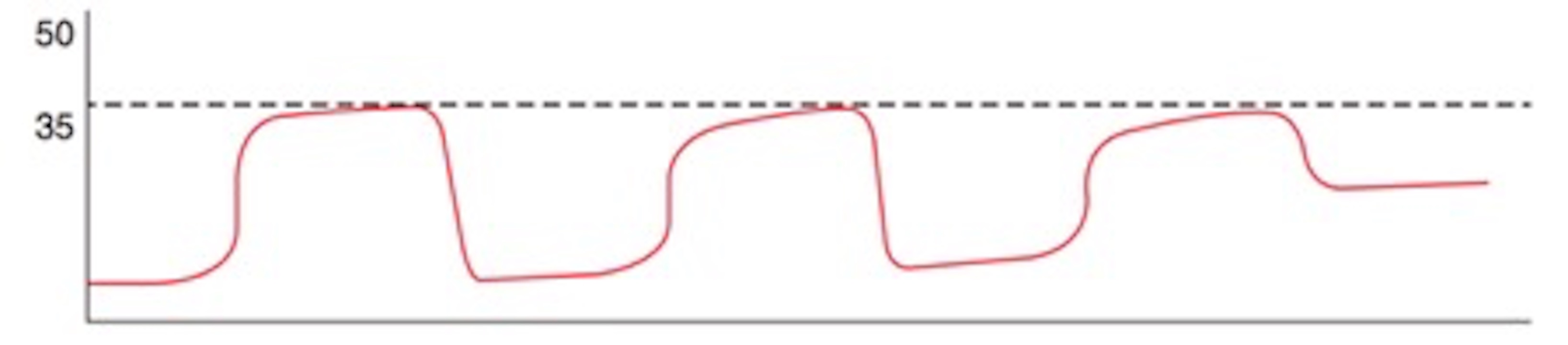
Tintinalli 2016
- Hypoventilation – Increased amount of CO2 expired each breath, without a change in baseline
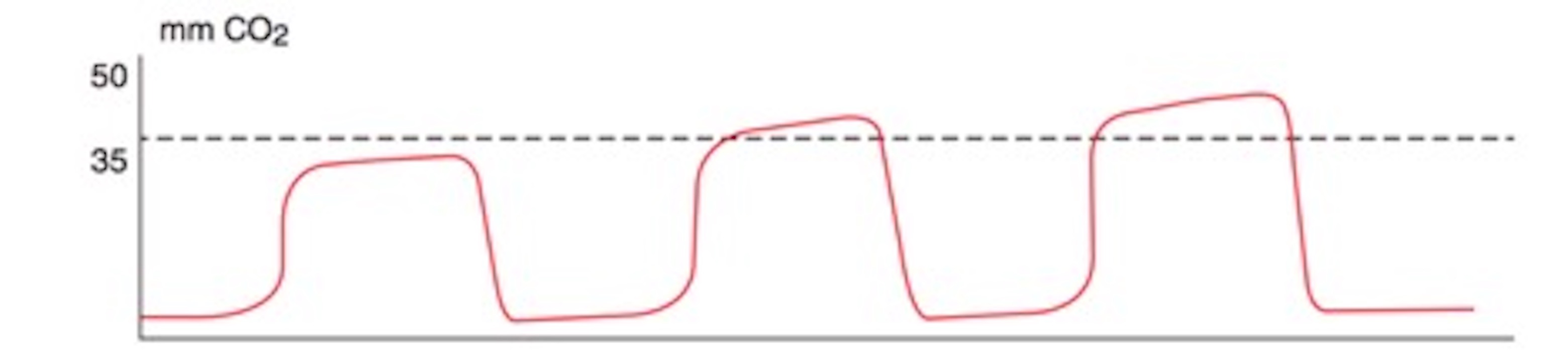
Tintinalli 2016
- Apnea – Serially decreasing amounts of CO2 as decreased amount of CO2 expired
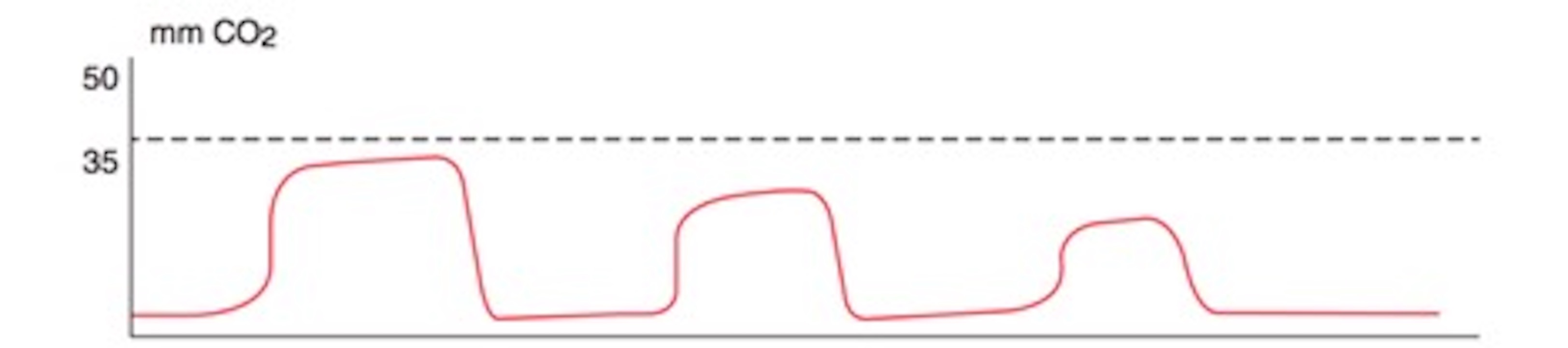
Tintinalli 2016
Clinical Applications in the Emergency Department
- Spontaneously Breathing Patients
- Sedated patients (Opioid Abuse, EtOH intoxication, procedural sedation, etc.)
- Monitoring Airway Ventilation
- Unlike pulse-oximetry, not prone to motion artifact
- Earlier recognition of respiratory depression when compared to pulse-oximetry (Deitch 2010)
- Median time to difference in detection = 60 seconds
- May also detect other adverse effects, such as bronchospasm, laryngospasm, or upper airway obstruction
- Metabolic Acidosis (Taghizadieh 2016)
- Metabolic acidosis → decreased HCO3 → compensatory hyperventilation → increased minute ventilation and decreased ETCO2
- Obstructive Lung Disease
- Upsloping of alveolar plateau due to alveolar leak of CO2
- Pattern also seen in leaks in breathing system (endotracheal tube leaks)
- Monitoring Airway Ventilation
- Sedated patients (Opioid Abuse, EtOH intoxication, procedural sedation, etc.)
- Ventilated Patients/Apneic Patients
- ET Tube Placement
- The gold standard for confirmation of tracheal placement (Grmec 2002)
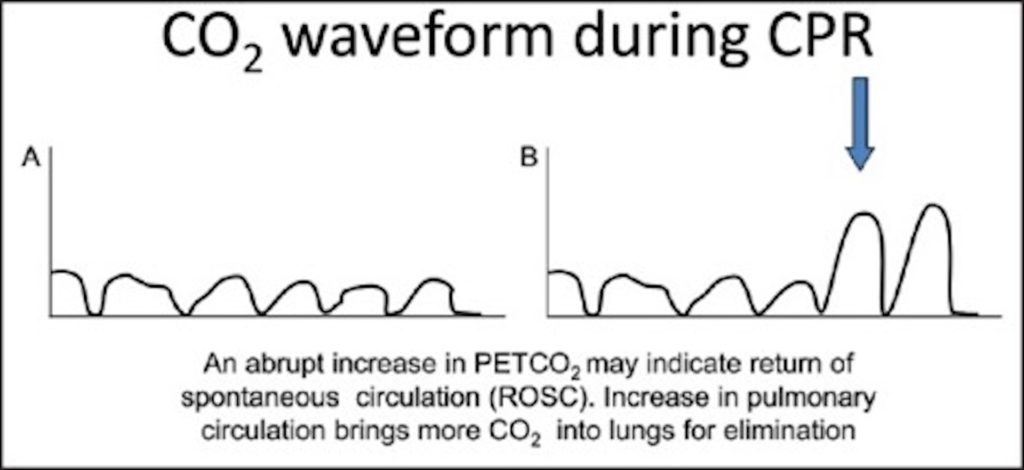
- CPR Effectiveness/ROSC
- Can provide a quantitative measure of chest compression effectiveness
- Prognostic factor of ROSC if <10 mmHg at 20 min of CPR (Levin 1997)
- An early indicator of reperfusion from ROSC is sudden rise in EtCO2 and thereby may help to decrease deleterious pauses in chest compressions for pulse checks
- ET Tube Placement
Kodali 2014
Take Home Points
- Capnography is the measure of carbon dioxide expired during each breath over time
- Capnography can be an accurate quantitative measure of a sedated patients respiratory status
- The gold standard for ensuring accurate endotracheal tube placement
- The waveform’s shape, frequency, baseline, can be suggestive of various pathologies
References
Deitch K, Miner J, Chudnofsky CR, Dominici P, Latta D. Does end tidal CO2 monitoring during emergency department procedural sedation and analgesia with propofol decrease the incidence of hypoxic events? A randomized, controlled trial. Ann Emerg Med. 2010;55(3):258-64. PMID: 19783324
Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28(6):701-4. PMID: 12107674
Kodali BS, Urman RD. Capnography during cardiopulmonary resuscitation: Current evidence and future directions. J Emerg Trauma Shock. 2014;7(4):332-40. PMID: 25400399
Levine RL, Wayne MA, Miller CC. End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. N Engl J Med. 1997;337(5):301-6. PMID: 9233867
Long B, Koyfman A, Vivirito MA. Capnography in the Emergency Department: A Review of Uses, Waveforms, and Limitations. J Emerg Med. 2017;53(6):829-42. PMID: 28993038
Marx JA, Rosen P. Rosen’s emergency medicine : concepts and clinical practice. 8th ed. Philadelphia, PA: Elsevier/Saunders; 2014.
Taghizadieh A, Pouraghaei M, Moharamzadeh P, Ala A, Rahmani F, Basiri Sofiani K. Comparison of end-tidal carbon dioxide and arterial blood bicarbonate levels in patients with metabolic acidosis referred to emergency medicine. J Cardiovasc Thorac Res. 2016;8(3):98-101. PMID: 27777693
Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Meckler GD, Yealy DM. Tintinalli’s emergency medicine : a comprehensive study guide. Eight edition. ed. New York: McGraw-Hill Education; 2016. xliii, 2128 pages p.

Can’t the ETCO2 vary much more than 5 from PaCO2? I think that sentence above “EtCO2 closely correlated with PaCO2– EtCO2 approximately 5 mmHg higher than PaCO2” is an oversimplification.