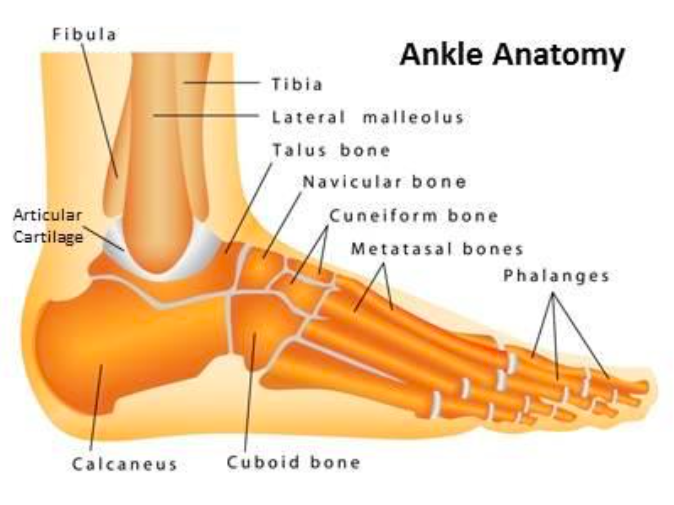
Ankle Anatomy (http://www.tsaog.com/)
Definition: Fracture of the distal tibia and/or fibula. These regions are commonly referred to as the medial, lateral or posterior malleoli
Mechanism:
- Twisting force on the ankle that leads to supination or pronation of the midfoot relative to the ankle and internal or external rotation of the talus within the joint
- Direct trauma to the distal tibia/fibula
Epidemiology:
- 187 fractures per 100,000 people per year, no gender predominance.
- 60-70% are unimalleolar, 15-20% bimalleolar and 7-12% are trimalleolar
Physical Exam:
- Look for swelling, gross deformity, and inability to bear weight
- Check for skin abnormalities such as laceration, blistering, or tenting.
- Palpate for tenderness at the medial and lateral malleoli, the base of the 5th metatarsal (Jones fracture) , the navicular bone, and along the entire length of the fibula (Maisonneuve fracture),
- Perform a complete neurovascular exam prior to manipulation and radiographs
Classification Systems
- Lauge-Hansen (Lauge-Hansen 1950)
- Supination-Adduction (SA): (~20% ankle fractures)
- Stage 1: Transverse fracture of lateral malleolus below the level of the mortise or lateral ligament tear
- Stage 2: Oblique fracture of medial malleolus
- Supination-external rotation (SER): ~60% of ankle fractures
- Stage 1: tear of anterior-inferior tibiofibular ligament (AITFL) or avulsion of anterior tibia
- Stage 2:Spiral fracture of the lateral malleolus at and above level of mortise
- Stage 3: Tear of the posterior-inferior tibiofibular ligament (PITFL) or avulsion of posterior malleolus
- Stage 4: Transverse fracture of medial malleolus or tear of deltoid ligament (trimalleolar fracture)
- Pronation-external rotation (PER): ~20% of ankle fractures
- Stage 1: Transverse fracture of the medial malleolus or tear of the deltoid ligament
- Stage 2: AITFL tear
- Stage 3: High spiral fracture of lateral malleolus above level of mortise
- Stage 4: PITFL tear or avulsion of posterior malleolus
- Supination-Adduction (SA): (~20% ankle fractures)
- Pronation-abduction (PA): <0.5% of ankle fractures
- Stage 1: Transverse fracture of medial malleolus or tear of deltoid ligament
- Stage 2: AITFL tear
- Stage 3: Transverse comminuted fracture of the fibula above the level of the syndesmosis
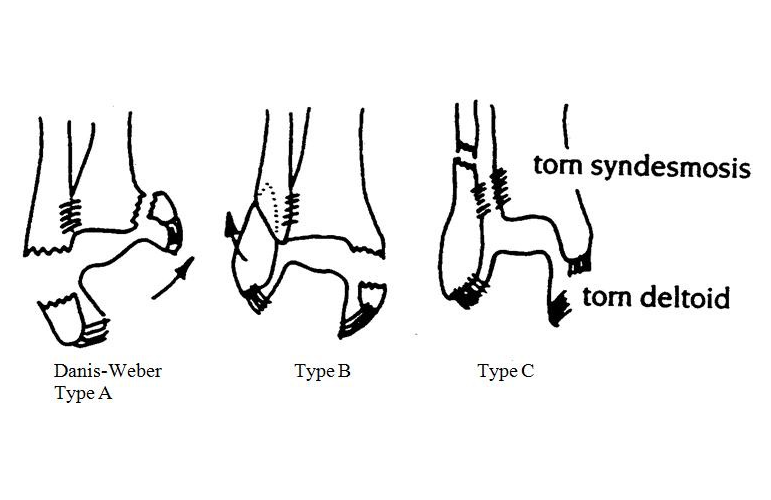
- Danis-Weber (based on location of fibular fracture)
- Type A (equivalent to Lauge-Hansen SA)
- Below the level of the talar dome
- The tibiofibular syndesmosis and the deltoid ligament are intact
- The medial malleolus is often fractured
- Usually stable if the medial malleolus is intact
- Type B (equivalent to Lauge-Hansen SER)
- Distal extent at the level of the talar dome
- The distal tibiofibular joint is widened indicating a syndesmotic injury
- Medial malleolus may be fractured
- Variable stability
- Type C (equivalent to Lauge-Hansen PER)
- Above the level the talar dome
- Tibiofibular syndesmosis disrupted
- Medial maleolus and/or deltoid ligament injury present
- Almost all are unstable
- Type A (equivalent to Lauge-Hansen SA)
Lauge Hansen Classification System
X-ray Findings
- Ottawa Ankle Rule
- Should be applied to determine which patients with traumatic ankle pain need imaging
- Test Characteristics: Sensitivty 100%, Specificity 40.1% (Stiell 1992)
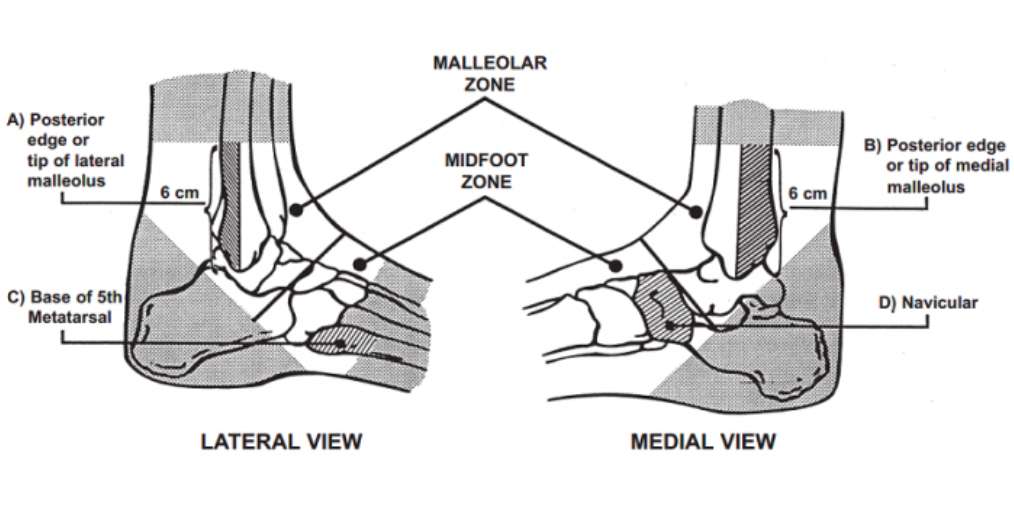
Ottawa Ankle Criteria (Stiell 1992)
- X-ray of ankle and/or foot indicated if patient has any tenderness at these landmarks
-
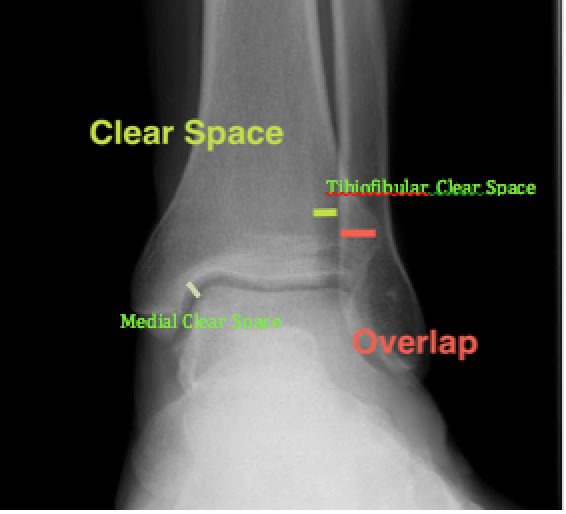
Normal AP Ankle X-Ray (http://posterng.netkey.at/)
X-ray Views
- Decreased tibiofibular overlap (<6mm on AP or <1mm on Mortise)
- Increased medial clear space (>4mm). Obtain stress view to see if the medial clear space is >5mm with external rotation of a dorsiflexed foot indicating deep deltoid disruption
- Increased tibiofibular clear space (<6mm on AP and Mortise views)
- Acquire AP, Lateral, Mortise (15-20 degrees of internal rotation so that the lateral and medial malleoli are in a horizontal line perpendicular to the xray beam)
- Consider external rotation stress view when there is tenderness to palpation of the medial malleoli or the following
-
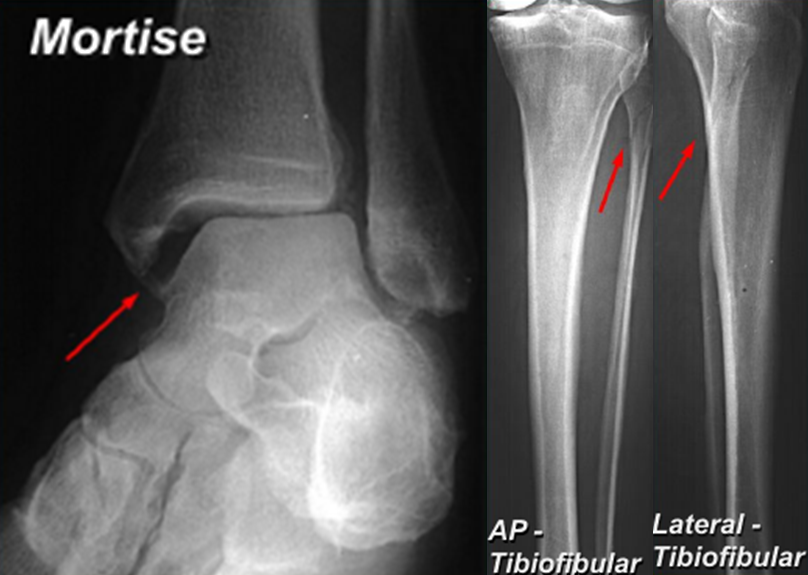
Maisonneuve Fracture (meds.queensu.ca)
Maisonneuve fracture
- Spiral fracture of the proximal third of the fibula with an associated fracture of the medial malleolus or rupture of the deep deltoid ligament (PER4 fracture)
- Palpation along the entire length of the fibular is important in order to pick up signs of this injury as it can be seen in patients with relatively unremarkable ankle X-rays
- If the patient is discovered to have either a medial malleolus fracture or high fibular fracture on X-ray, tibia-fibula films are indicated to rule out this type of fracture.
- Pilon Fracture
- Fracture of the distal part of the tibia involving the articular surface with the talus bone
- Usually occurs in high energy injuries and most likely will require surgery, as these fracture tend to be unstable
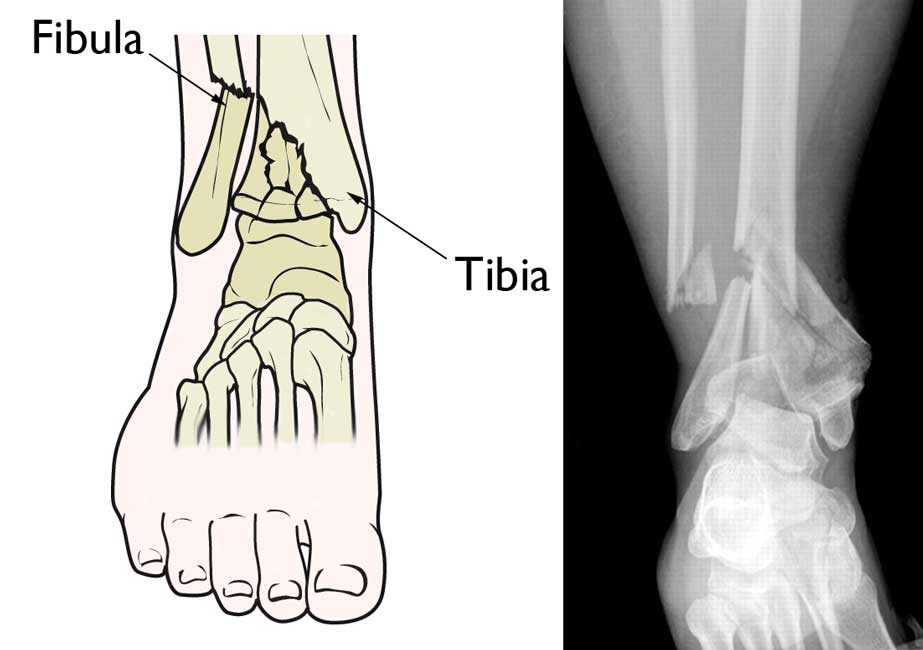
Pilon Fracture (http://orthoinfo.aaos.org/)
ED Management
- Open fractures or fractures with neurovascular compromise require immediate orthopedic consultation and treatment
- Ankle fractures with concomitant dislocation need to be emergently reduced
- Obtaining anatomic alignment critical to avoid downstream arthritic changes (even in those requiring operative fixation)
Operative vs. Non-Operative Management
- Generally, one can use Danis Weber classification to distinguish non-operative vs operative management. Type A fractures are almost always non operative. Many Type B fractures require operative management (but not all) and type C fractures tend to all require operative management.
- Non-operative
- Stable, non-displaced, isolated uni-malleolar fracture (without opposing ligament injury), can be splinted in short leg splint or boot (with ankle at 90 degrees) with early weight bearing as tolerated (Phillips 1985), Mehta 2014)
- Operative:
- Indications are loss of joint congruency (i.e. pilon fractures) or loss of joint stability
- Unstable (when two or more sites are significantly injured) and/or displaced fractures require reduction, splinting (posterior ankle with stirrup splint- see picture below), strict non-weightbearing, and future ORIF with follow up within 1 week (Phillips 1985), Mehta 2014)
Prognosis
- Post-traumatic arthritis seen in up to 70% of cases and commonly occurs when the normal anatomy is not restored
- Failure to recognize ankle instability can lead to articular surface degeneration and early osteoarthritis (5% in those with unrecognized unimalleolar fracture vs 20% in those with unrecognized bimalleolar fracture). This is common in those with single malleolus fracture with undetected opposing ligament injury
- Rehabilitation is important component of treatment to help patients return to baseline range of motion, strength and proprioception (Mehta 2014)
Take Home Points
- Utilize the Ottawa Ankle Rule to minimize the amount of X-rays performed
- It is imperative to perform a good physical exam and to acquire the appropriate imaging to capture fractures that may easily be missed
- Associated dislocations should be reduced and anatomic alignment should be achieved prior to immobilization
- Obtain emergent orthopedic surgery consultation for open fractures or evidence of neurovascular compromise
Read more
Radiopaedia: Weber Classification of Ankle Fractures
Radiopaedia: Ankle Fractures
Ortho Bullets: Ankle Fractures
Core EM: Ottawa Ankle Clinical Decision Instrument Derivation Study
References
Egol K et al. Handbook of Fractures. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health, 2010. Pages 476-506
Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60(5):957-985. PMID: 15411319
Mehta SS et al. Understanding risk and complications in the management of ankle fractures. Indian J Orthop 2014;48:445-52. PMID: 25298549
Phillips WA et al. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg 67(1): 67-78. PMID:3881447
Stiell, I. G., et al. (1992). “A study to develop clinical decision rules for the use of radiography in acute ankle injuries.” Ann Emerg Med 21(4): 384-390. PMID: 1554175




in your supination adduction chart, the weber fracture is labeled as B, it is a weber A fracture distal to the syndesmosis that is assocaited with SAD