Background
Prior to the creation of the Ottawa Ankle Decision Instrument, most patients presenting to the Emergency room with a complaint of acute ankle injury had ankle and or foot radiographs ordered to evaluate for fracture, even though the incidence of fracture among this population is relatively low (~ 15%). While ankle radiographs do not expose the patient to large amounts of radiation, they do incur costs for patients, costs for the health care system, increase length of stay and contribute to Emergency Department crowding. Clinical decision instruments can help clinicians decide which patients do not need imaging without missing clinically significant fractures.
Clinical Question
Can a decision instrument help determine which patients with acute ankle injuries do not need imaging thus reducing the use of ankle and foot X-rays?
Population
Adults >18 presenting to the emergency room with blunt ankle injuries including twisting, MVA, fall from height.
Intervention
Standardized clinical assessments were filled out on 32 different variables by trained assessor physicians prior to undergoing radiography of either ankle, foot or both. A second trained physician assessed the patient as well to evaluate for inter-observer variability. After finding variables with the highest correlation that also had kappa scores or inter-observer agreement of at least 60% greater than chance, they applied a recursive partitioning model set with 100% sensitivity and allowing for low specificity. The final model was chosen for simplicity as it had the fewest number of variables. A similar technique was used for mid foot fractures.
Control
Investigators compared the predictor variables with the presence of clinically significant fracture determined by a radiologist who was blinded to the assessments that had been completed
Outcomes
Creation of a decision instrument that reduces the use of imaging of ankle injuries while also not missing clinically significant fracture greater than 3mm avulsion (generally accepted as the cutoff point at which a plaster splint would be applied at the investigating institutions)
Design
Multi-center prospective cohort study
Excluded
Age < 18, non blunt trauma mechanism, patients who only had superficial skin injuries, pregnant patients, those referred from an outside hospital with prior radiographs, injury occurred > 10 days earlier, re-evaluation of previously evaluated injury
Primary Results
- 750 patients were enrolled and assessed for the outcome measure
- Twisting mechanism present in 83.9% of patients
- 520 patients had ankle radiographs only, 61 had foot radiographs only, and 169 had both
- There were 70 patients (9.3%) with significant malleolar fractures, and 32 (4.2%) with significant mid foot fractures
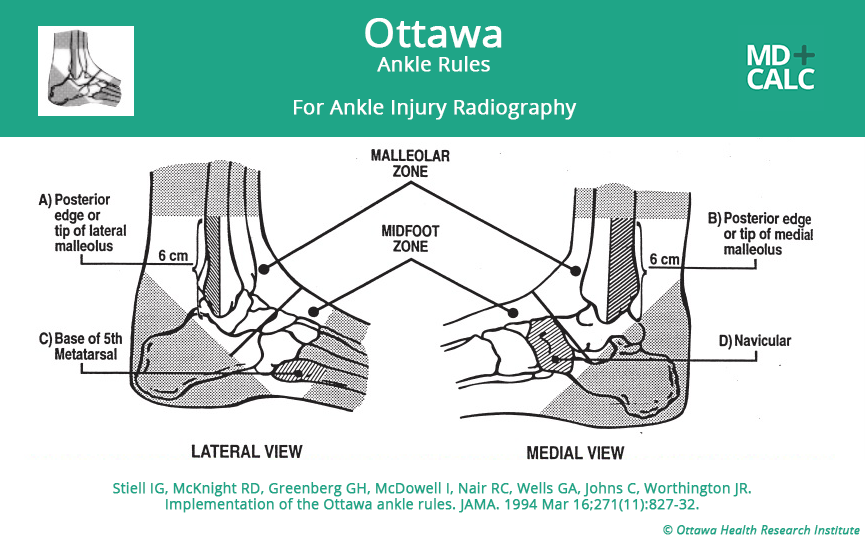
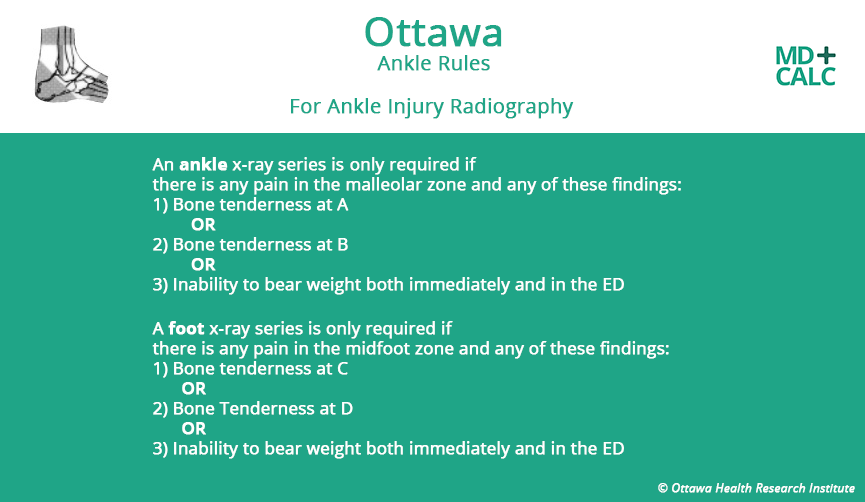
- A decision tool was created for ankle films including 4 variables formed through recursive partitioning. A second decision tool for mid foot fractures including 3 variables was also created using the same methods
Critical Findings
- Derived Decision Instrument Performance (for identifying clinically significant fractures)
- Ankle Fractures
- Sensitivity: 100%
- Specificity: 41.7% and 100% sensitivity and 24.7% specificity to identify clinically significant mid foot fractures
- Foot Fractures
- Sensitivity: 100%
- Specificity: 24.7%
- Ankle Fractures
- All clinically significant fractures were identified using this tool
- A potential savings of 36% of ankle radiographs, and 21.3% of foot radiographs could have been achieved by using this rule.
Strengths
- Large, multicenter trial
- Study asked a clear clinical question that was patient centered
- Outcome measures were objective reducing bias
- Radiologists were blinded to the clinician assessments
- All variables were assessed by two clinicians in order to obtain inter-observer agreement measures
Limitations
- Not all patients had both foot and ankle radiography performed
- Twisting mechanism made up the majority of injuries limiting generalizability to other mechanisms
Author's Conclusions
“Highly sensitive decision rules have been developed and
will now be validated; these may permit clinicians to confidently reduce the number of radiographs ordered in patients with ankle injuries.”
Our Conclusions
This was a high-quality study with a good sample size. The final decision instrument had excellent sensitivity for detecting clinically significant fractures However this study is only derivation, and at the time of original publication had not undergone any validation, indicating it was not ready for use in clinical settings.
Subsequent studies have validated the rule in multiple clinical settings (Stiell 1993, Stiell 1994, Stiell 1995), as well as in children (Plint 1999) who were not included in this original derivation study. Impact analyses have been completed as well indicated that this decision rule informs the decisions made by many physicians, however while 91-99% of US emergency physicians are aware of the rule, only 32% report that it informs there clinical decisions.
Potential Impact To Current Practice
This article was named one of ALiEM’s Landmark Articles (www.aliem.com/52-articles-in-52-weeks-landmark-em-articles-2013/). It has become an integral part of how many physicians in the ED assess patients who present with ankle and foot injuries.
Bottom Line
The Ottawa ankle decision instrument is a highly sensitive tool for determining which patients do not need imaging performed.
Read More
Stiell IG et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA 1993; 269(9):1127-32 PMID: 8433468
Stiell IG et al. Implementation of the Ottawa Ankle Rules. JAMA 1994; 271 (11): 827-832. PMID: 8114236
Stiell IG et al. A multicentre trial to introduce clinical decision rules for the use of radiography in acute ankle injuries. BMJ 1995; 311:594-597. PMID: 7663253
Plint AC et al. Validation of the Ottawa Ankle Rules in children with ankle injuries. Acad Emerg Med 1999; 6(10) 1005-9 PMID: 10530658