Show Notes
Overview
- Blunt neck trauma comprises 5% of all neck trauma
- Mortality due to loss of airway more so than hemorrhage
Mechanism
- MVCs with cervical hyperextension, flexion, rotation during rapid deceleration, direct impact
- Strangulation: hanging, choking, clothesline injury (see section on strangulation in this chapter)
- Direct blows: assault, sports, falls
Initial Management/Primary Survey
- Airway
- Evaluate for airway distress (stridor, hoarseness, dysphonia, dyspnea) or impending airway compromise
- Early aggressive airway control: low threshold for intubation if unconscious patient, evidence of airway compromise including voice change, dyspnea, neurological changes, or pulmonary edema
- Assume a difficult airway
- Breathing
-
- Supplemental oxygen
- Assess for bilateral breath sounds
- Can use bedside US to evaluate for pneumothorax or hemothorax
- Circulation
-
- Assess for open wounds, bleeding, hemorrhage
- IV access
- Disability
-
- Maintain C-spine immobilization
- Calculate GCS
- Look for seatbelt sign
Secondary Survey
- Evaluate for specific signs of vascular, laryngotracheal, pharyngoesophageal, and cervical spinal injuries with inspection, palpation, and auscultation
- Perform extremely thorough exam to evaluate for any concomitant injuries (e.g. stab wounds, gunshot wounds, intoxications/ ingestions, etc.)
Types of Injuries
-
-
- Carotid arteries (internal, external, common carotid) and vertebral arteries injured
- Mortality rate ~60% for symptomatic blunt cerebral vascular injury
- Mechanism
- Hyperextension and lateral rotation of the neck, direct blunt force, strangulation, seat belt injuries, and chiropractic manipulation
- Morbidity due to intimal dissections, thromboses, pseudoaneurysms, fistulas, and transections
- Clinical Features
- Most patients are asymptomatic and do not develop focal neurological deficits for days
- if Horner’s syndrome, suspect disruption of thoracic sympathetic chain (wraps around carotid artery)
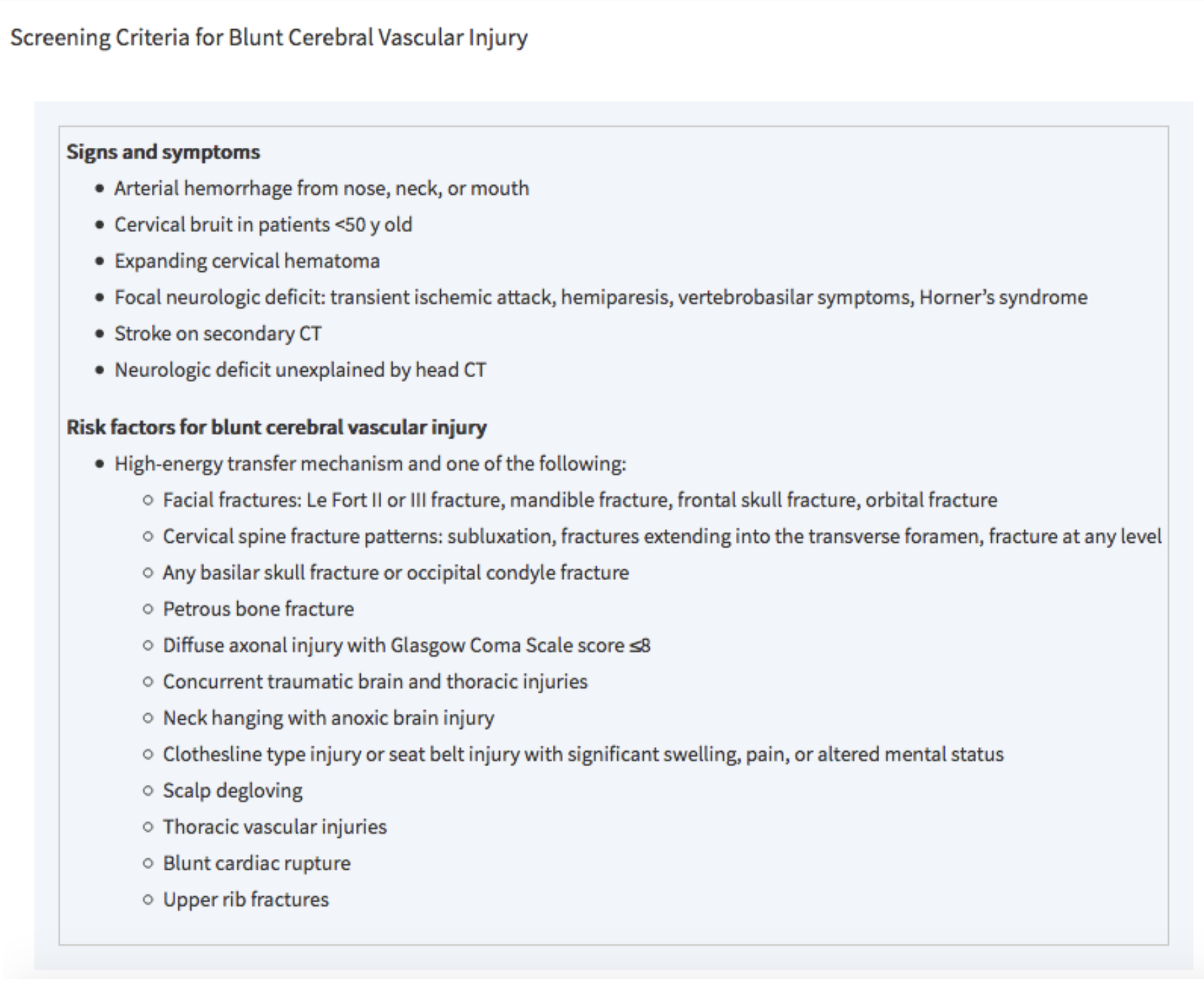
- specific screening criteria are used to detect blunt cerebrovascular injury in asymptomatic patients (see below)
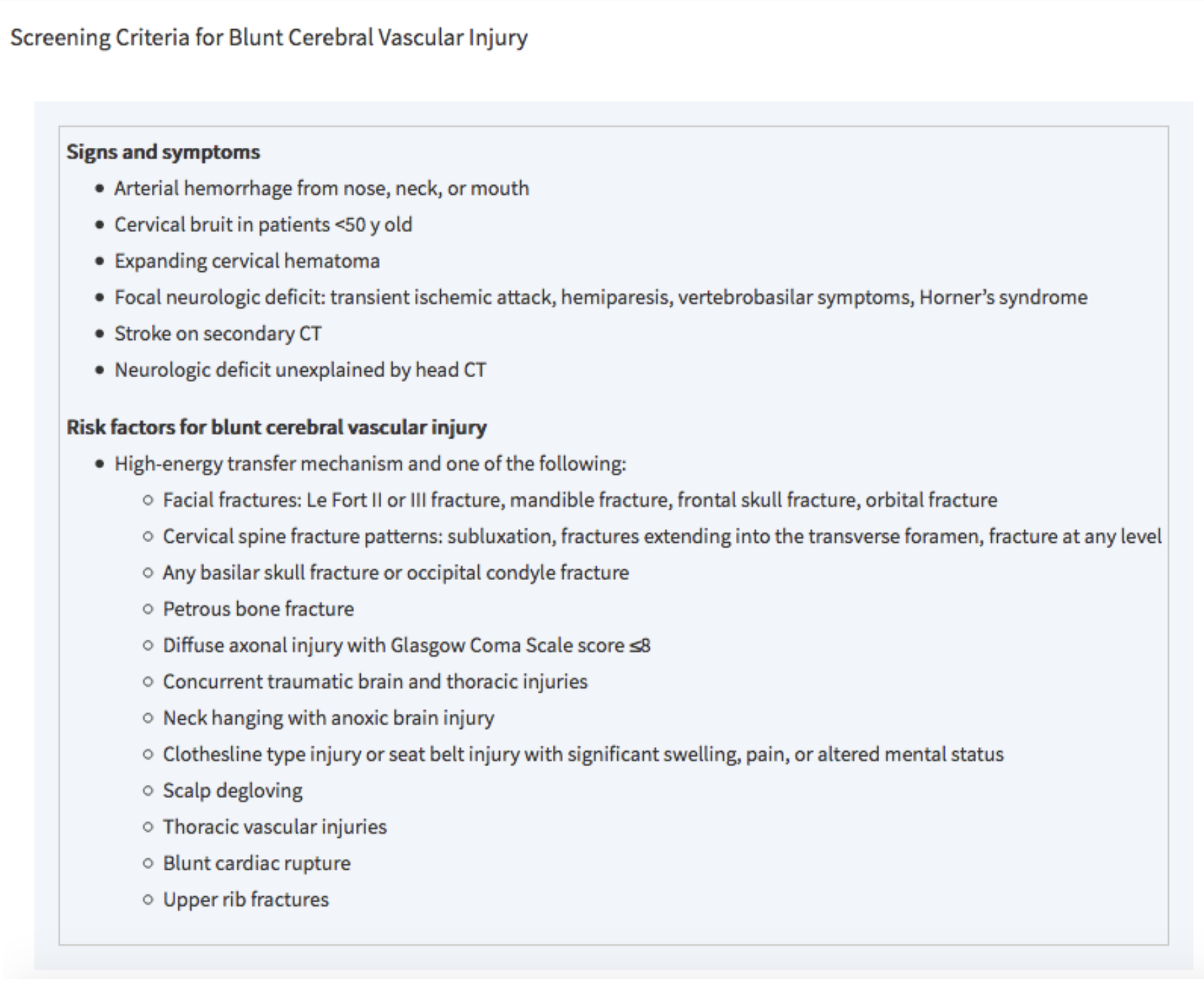
Tintinalli 2016
- Diagnostic Testing
- Gold standard for blunt cerebral vascular injury = MDCTA (multidetector four-vessel CT angiography)
- <80% sensitive but 97% specific
- Also images aerodigestive tracts and C-spine (unlike angiography)
- Followed by Digital Subtraction Angiography (DSA) for positive results or high suspicion
- Angiography is invasive, expensive, resource-intensive, and carries a high contrast load
- Management
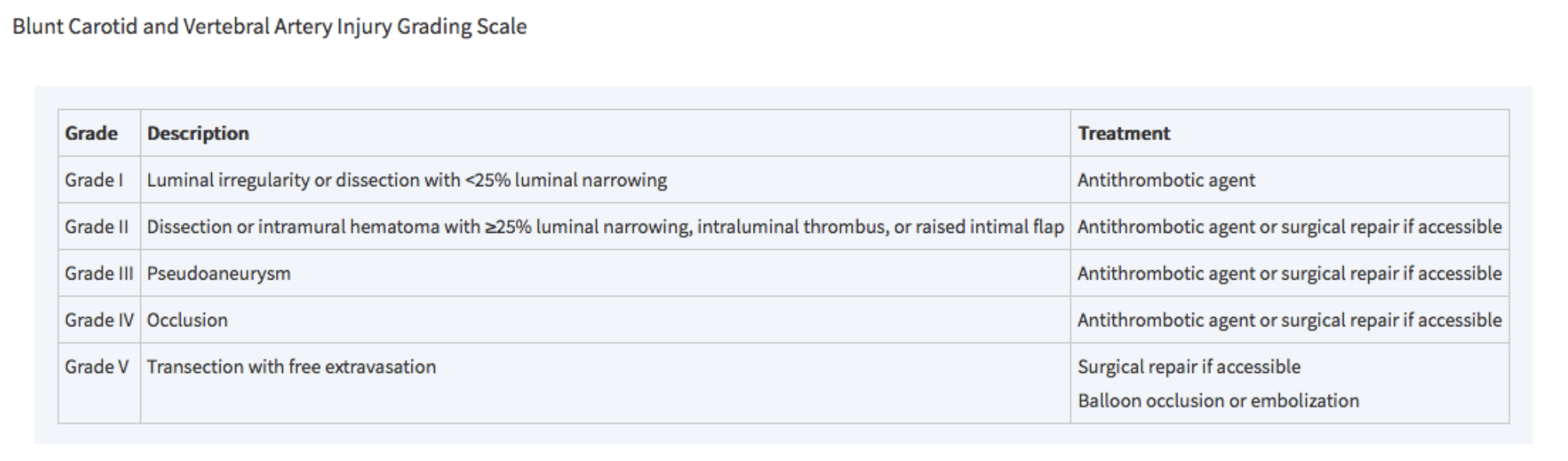
- Antithrombotics vs. interventional repair based on BCVI grading system
- Involve consultants early: trauma surgery, neurosurgery, vascular surgery, neurology
- All patients with blunt cerebral vascular injury will require admission
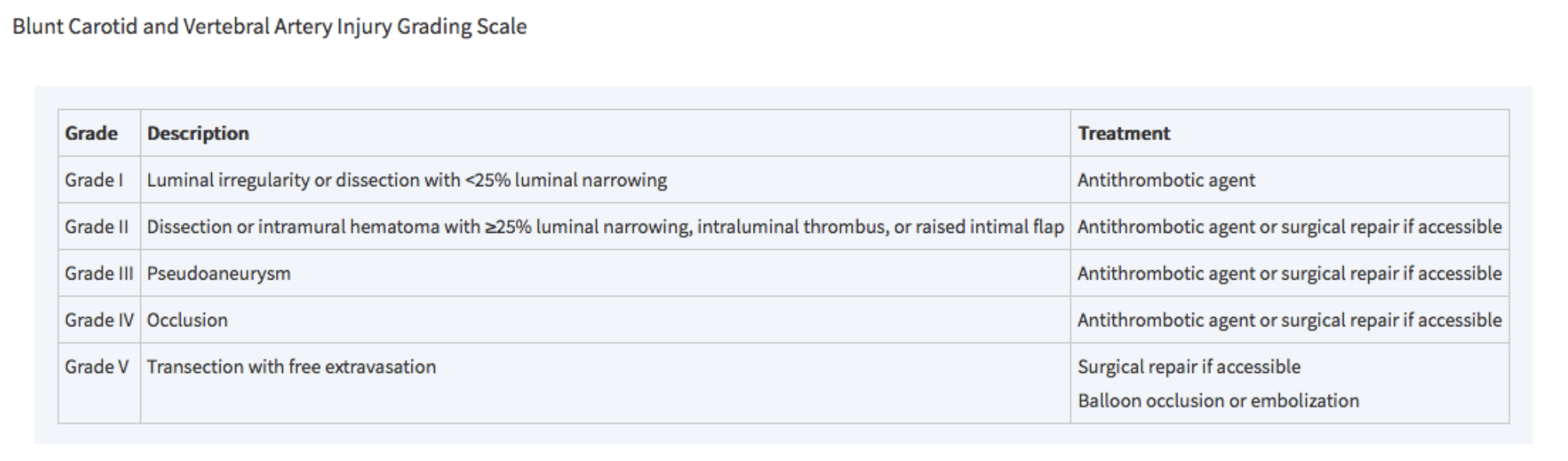
Tintinalli 2018
- Pharyngoesophageal injury
-
-
- Overview
- Rare in blunt neck trauma
- Includes hematomas and perforations of both pharynx and esophagus
- Mechanism
- Sudden acceleration or deceleration with hyperextension of the neck
- Esophagus is thus forced against the spine
- Clinical Features
- Dysphagia, odynophagia, hematemesis, spitting up blood
- Tenderness to palpation
- SC emphysema
- Neurological deficits (delayed presentation)
- Infectious symptoms (delayed presentation)
- Diagnostic Testing
- Esophagography with water-soluble contrast (e.g. Gastrograffin)
- If negative contrast esophagography, obtain flexible endoscopy (most sensitive)
- Combination of contrast esophagography + esophagoscopy has sensitivity close to 100%
- Swallow studies with water-soluble agent
- MDCTA
- Plain films of neck and chest
- Findings such as pneumomediastinum, hydrothorax, or retropharyngeal air may suggest perforation but are not sensitive
- Management
- All pharyngoesophageal injuries receive IV antibiotics with anaerobic coverage
- Parenteral/ enteral nutrition
- NGT should only be placed under endoscopic guidance to avoid further injury
- Medical management vs. surgical repair depending on extent of injury
- Surgical repair for esophageal perforations or pharyngeal perforations >2cm
- Involve consultants early: trauma surgery, vascular surgery, otolaryngology, gastroenterology
- All patients with blunt cerebral vascular injury will require admission
- Laryngotracheal injury
-
- Overview
- Occurs in >0.5% of blunt neck trauma
- Includes hyoid fractures, thyroid/ cricoid cartilage damage, cricotracheal separation, vocal cord disruption, tracheal hematoma or transection
- Mechanism
- Assault, clothesline injuries, direct blunt force from MVCs compressing the larynx between a fixed object and the spine
- Clinical Features
- Patients are often asymptomatic at first and then develop airway edema and/or hematoma resulting in airway obstruction
- Children are at higher risk for airway compromise due to less cartilage calcifications
- Diagnostic Testing
- Flexible fiberoptic laryngoscopy (FFL) to assess airway patency and extent of intraluminal injury
- MDCTA
- Obtain 1-mm cuts of larynx and perform multiplanar reconstructions
- Consider POCUS to detect laryngotracheal separation
- Plain films of neck and chest
- Poor sensitivity for penetrating neck trauma injuries
- Can show extraluminal air, fracture or disruption of cartilaginous (e.g. larynx) structures
- Management
- When securing airway, use an ETT that is one size smaller due to likelihood of airway edema
- Conservative management (IV antibiotics, steroids, observation) vs. surgical repair
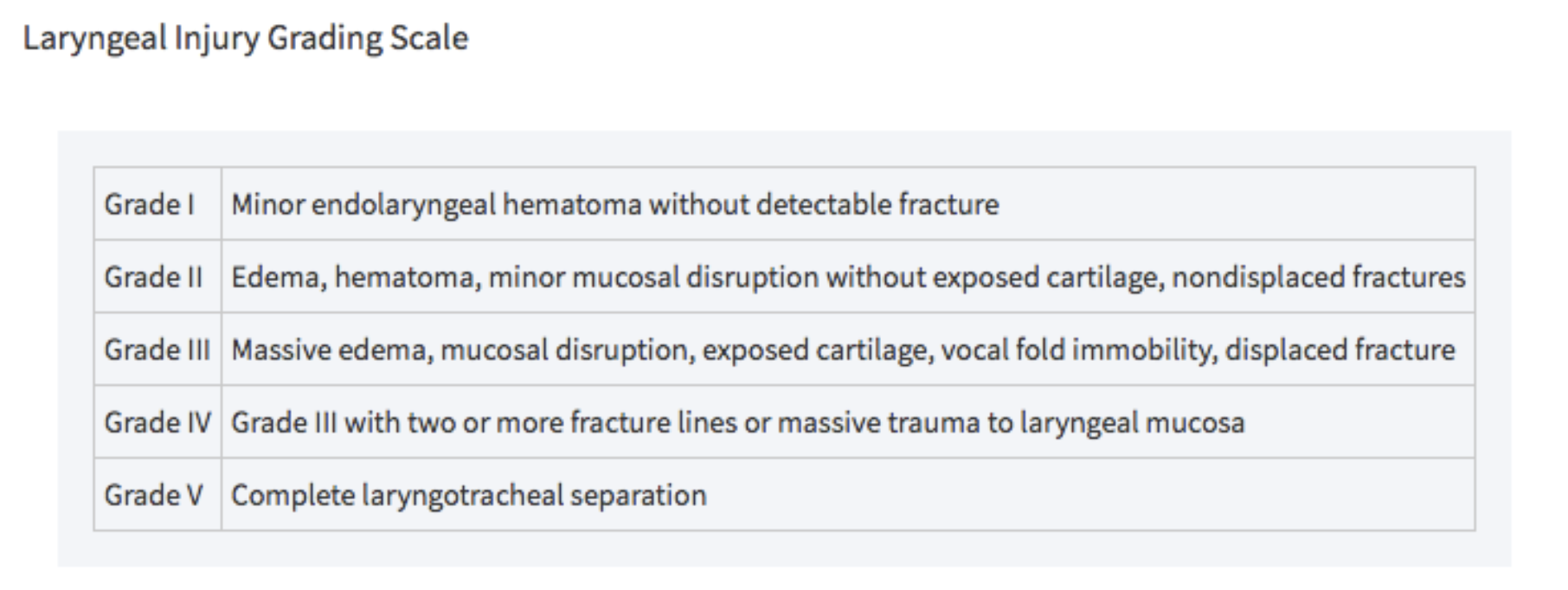
- Grades III, IV, and V laryngotracheal injuries as defined by Schaefer and Brown’s classification system require OR
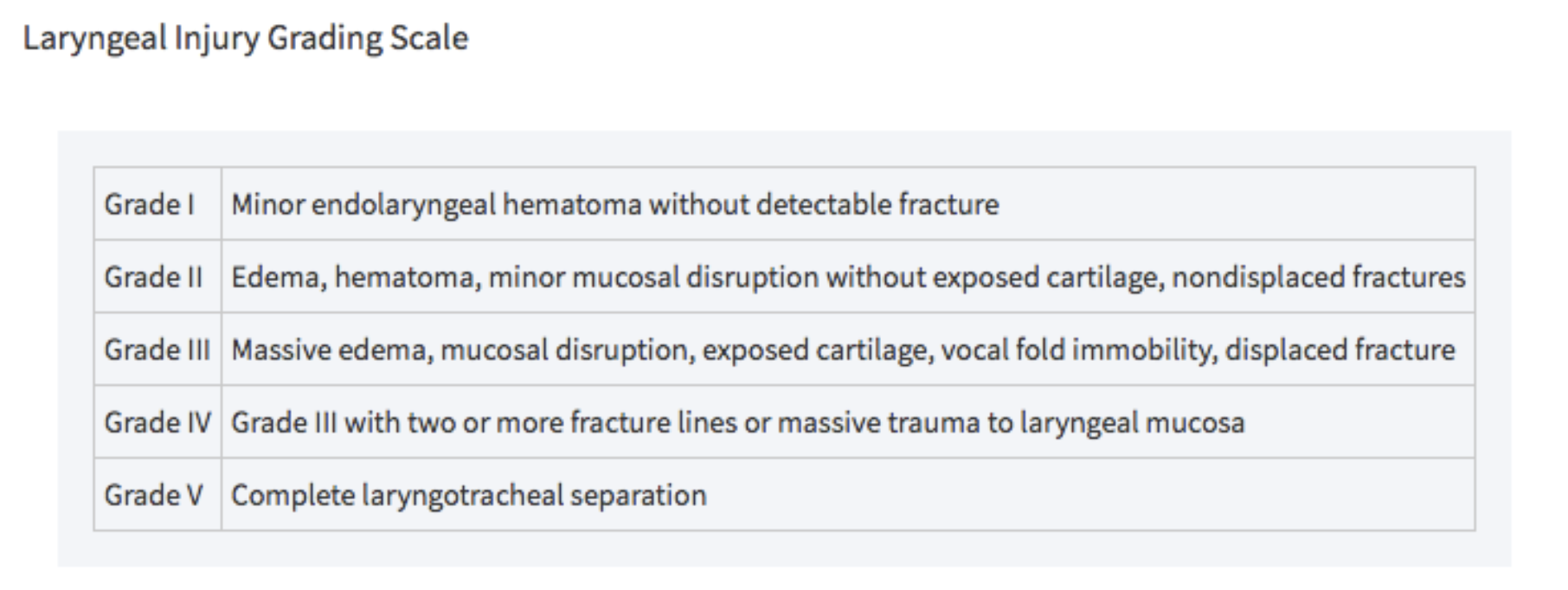 Tintinalli 2018
Tintinalli 2018
-
-
-
- Involve consultants early: trauma surgery, neurosurgery, vascular surgery, neurology, otolaryngology
- Cervical spine/ spinal cord injury
-
- See chapter for spinal trauma
Disposition
- Admit symptomatic patients to monitored setting
- Given delayed symptoms, consider monitoring patients who are asymptomatic on arrival
- Serial exams for worsening dyspnea, dysphonia, stridor, drooling, bruits, focal neuro deficits
- Only discharge after ruling out airway threat, neurological deficit, vascular injury, or suicidal/ homicidal ideation
- Monitor asymptomatic patients on home anticoagulation in ED for at least 6 hours from trauma to rule out delayed neck hematoma
- Social work and/or psychiatry for patients in whom you suspect suicide risk or domestric violence, look for other signs of self harm
Take Home Points
- Aggressive early airway management for unconscious patient, evidence of airway compromise including voice change, dyspnea, neurological changes, or pulmonary edema
- Involve consultants early: trauma surgery, neurosurgery, vascular surgery, neurology, otolaryngology
- Victims of blunt cerebral vascular injury may present completely asymptomatic but develop delayed neurological symptoms; close observation and monitoring is recommended especially for patients on home anticoagulation
- Remember to evaluate for concomitant injuries
- Psychiatric evaluation for all attempted suicides
References
- Bromberg, William. et al. Blunt Cerebrovascular Injury Practice Management Guidelines: The Eastern Association for the Surgery of Trauma. J Trauma. 68 (2): 471-7, Feb 2010.
- Cothren CC, Moore EE, Biffl WL, et al. Anticoagulation is the gold standard therapy for blunt carotid injuries to reduce stroke rate. Arch Surg. 2004;139:540–545; discussion 545–546.
- Joshua AA. Neck Trauma, Blunt, Anterior. In: Schaider J, Barkin R, Hayden S, Wolfe R, Barkin A, Shayne P, Rosen P. Rosen and Barkin’s 5-Minute Emergency Medicine Consult. 5th Edition. Philadelphia, PA: Wolters Kluwer; 2015; 738-739.
- Tintinalli, J., Stapczynski, J. Stephan, editor, Ma, O. John, editor, Yealy, Donald M., editor, Meckler, Garth D., editor, & Cline, David, editor. (2018). Tintinalli’s emergency medicine : A comprehensive study guide (9th ed.).
- Walls, R., Hockberger, Robert S., editor, & Gausche-Hill, Marianne, editor. (2018). Rosen’s emergency medicine : Concepts and clinical practice (Ninth ed.).
- Advanced trauma life support. (2018). 10th ed. Chicago, IL: American College of Surgeons.
Special thanks to Sana Maheshwari, MD
NYU Bellevue Emergency Medicine Residency PGY3
 Tintinalli 2018
Tintinalli 2018
Thanks for these wonderful reviews. Short full of so much information. I’m at the end of my career after 40 years 20 years as a paramedic and 20 years as a PA and it’s Interesting to re-learn stuff I’ve forgotten, stuff I learned from doctors while working in the ER, and stuff I wish I’d known. Best regards, Mike