Show Notes
Episode Produced by Audrey Bree Tse, MD
Background:
- Why do we care about Jones fractures?
- Propensity for poor healing due to watershed area of blood supply
- Fifth metatarsal fractures account for 68% of metatarsal fractures in adults
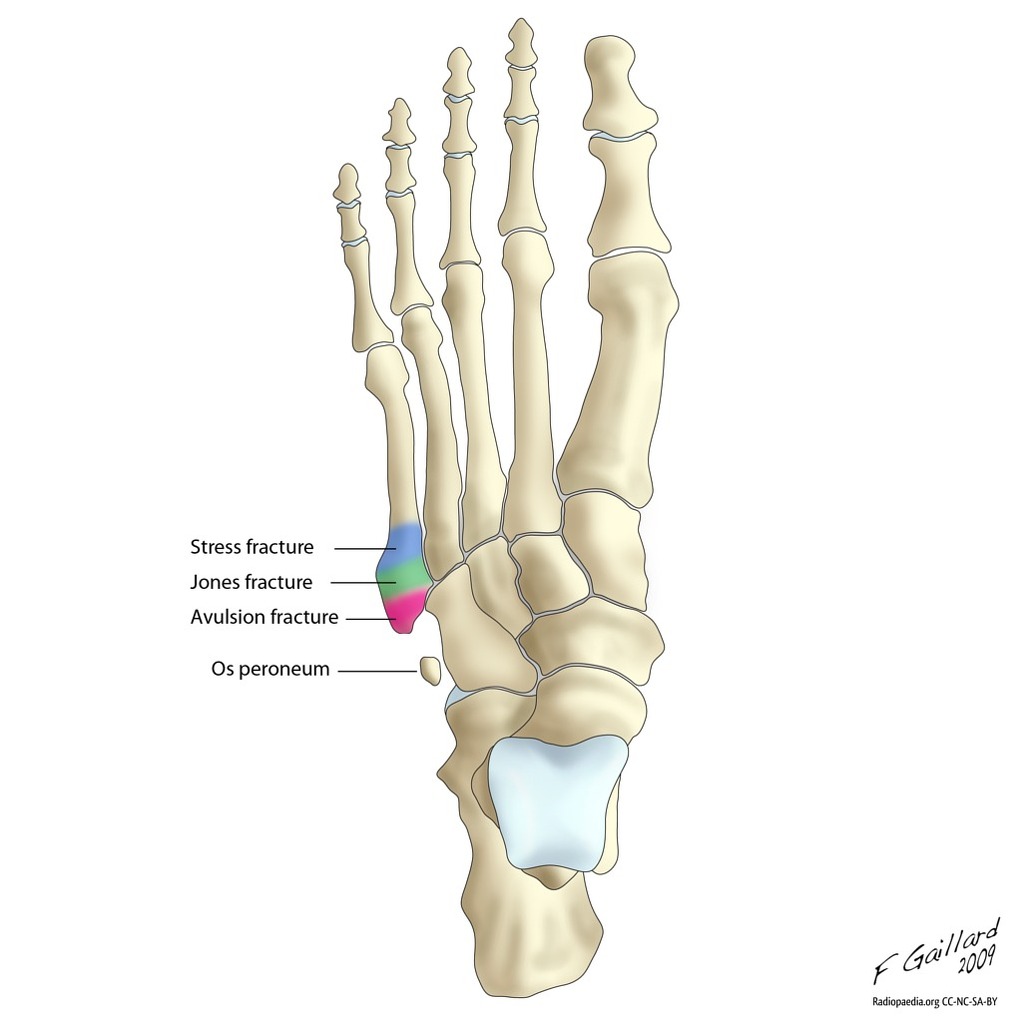
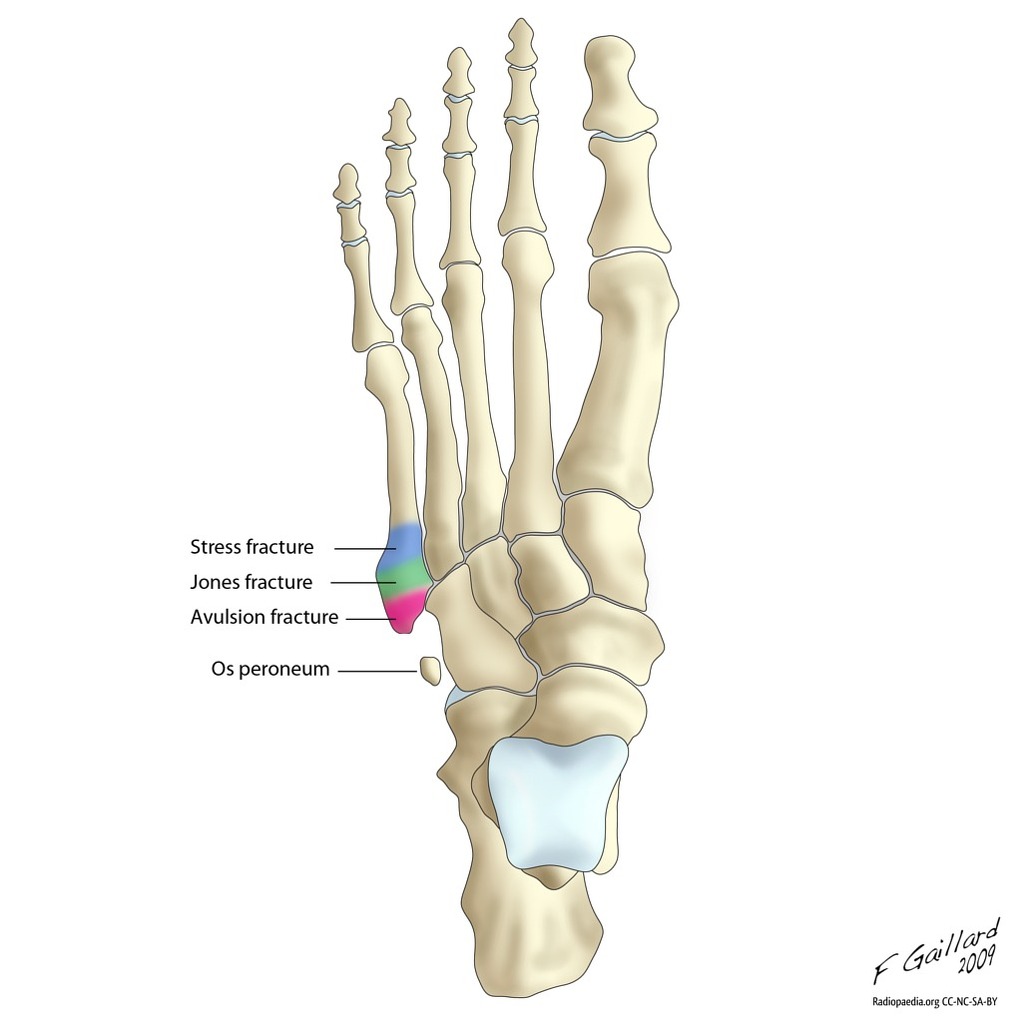
- Proximal 5th metatarsal fractures are divided into 3 zones (93% zone 1, 4% zone 2, 3% zone 3)
- Zone 1 (pseudo-Jones):
- Tuberosity avulsion fracture
- Typically avulsion type injuries due to acute episode of forefoot supination with plantar flexion
- Typical fracture pattern is transverse to slightly oblique
- Zone 2 (Jones fracture):
- Fracture at the metaphyseal-diaphyseal junction of the fifth metatarsal
- Typically acute episode of large adduction force applied to forefoot with the ankle plantar flexed
- Zone 3:
- Proximal diaphyseal stress fracture
- Typically results from a fatigue or stress mechanism
Clinical Presentation:
- History of acute or repetitive trauma to forefoot
- Fracture type / pattern closely related to injury location
- Foot often swollen, ecchymotic, very tender to fifth metatarsal +/- crepitus, inability to hear weight
Diagnosis:
- Clinical exam:
- Evaluate skin integrity
- Check neurovascular status
- Evaluate toes/ feet/ ankles/ tib fib/ knees/ hips, involved tendon function, associated adjacent structures (Achilles, ankle ROM/ function, etc)
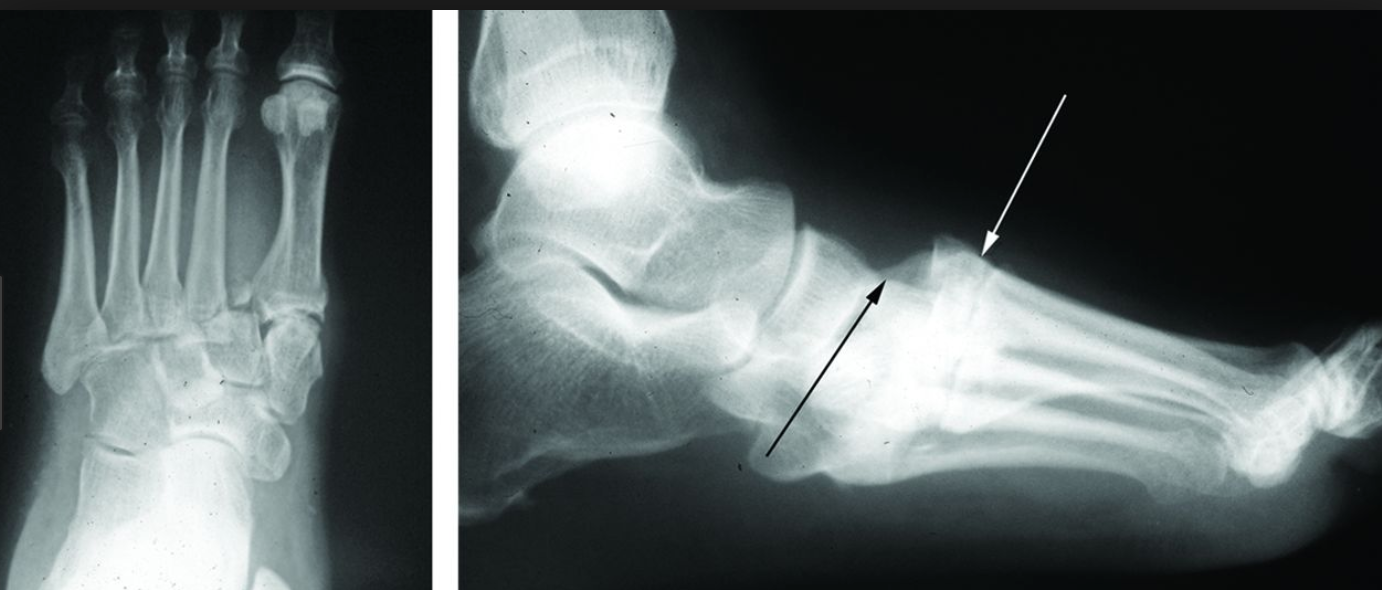
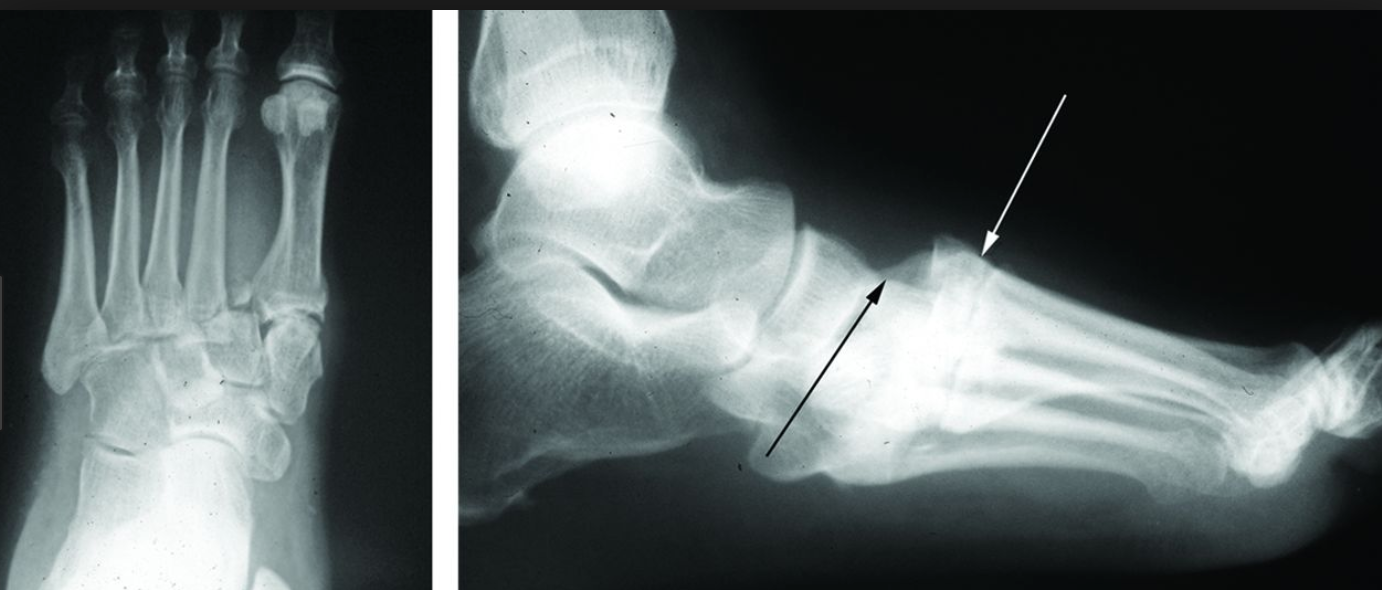
- 3 XR views: lateral, anteroposterior, 45* oblique
- Acute stress fractures are typically not detected on the standard 3 views; therefore, repeat XRs 10-14d after onset of sx (may see radiolucent reabsorption gap around fracture)
- For more complex mid foot trauma, consider CT to r/o Lisfranc
Treatment:
- Consider classification of fracture, patient demographics & activity level when deciding on treatment
- Tertiary care centers that have access to Orthopedics/Podiatry services
- Consider consultation for “true” Jones fractures, as some cases may be operatively managed acutely and/or for expedited follow-up to be arranged
- If working in community/rural locations: other than patients that present with “open” injuries, concerns for compartment syndrome (almost never), and “high-end”/professional athletes, there are generally no other circumstances that would require expedited transfer to a tertiary care center for immediate further evaluation.
- Less favorable outcomes associated with certain patient factors: female gender, DM, obesity
Surgical:
- Different modalities of surgery:
- Intramedullary screw
- Bone graft
- Closed reduction and fixation with K-wire
- ORIF (all +/- need for bone graft)
- Surgery likely recommended for displacement >10 degrees of plantar angulation or 3-4 mm of translation in any plane
- Indications for OR:
- Neck and shaft fractures with >10 degrees plantar angulation or 3mm of displacement in any plane with insufficient closed reduction
- Avulsion fractures (zone one) with >3 mm of displacement or comminuted
- Zone two fractures: displaced zone two fractures require operative management. For acute non displaced Jones fractures, consider early intramedullary screw fixation in athletes (studies have shown return to sport ~ 8 weeks, weight bearing within 1-2 weeks)
- Zone three fractures (diaphyseal stress fractures) in athletes
Nonoperative:
- All non displaced fifth metatarsal fractures can be treated non operatively
- Non displaced zone 1 fractures: protected weight bearing/ symptomatic care in short leg walking cast, air-boot, posterior splint, or compression wrap/ rigid shoe until discomfort subsides
- Zone 2 and 3 fractures are more complex because they often result in prolonged healing time and potential for delayed/ nonunion
- Acute zone 2 fractures: nonweightbearing in short leg cast for 6-8 weeks
- Acute zone 3 fractures: nonweightbearing in short leg cast for up to 20 weeks
- With respect to athletes: repeat fracture after surgical treatment of Jones fracture can occur after healing and screw removal; thus it is recommended that the screw be left in until the end of the athlete’s career
References:
Bowes J, Buckley R. Fifth metatarsal fractures and current treatment. World J Orthop. 2016;7(12):793–800. Published 2016 Dec 18. doi:10.5312/wjo.v7.i12.793
Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006 Mar; 27(3): 172-4.
Rammelt S, Heineck J, Zwipp H. Metatarsal fractures. Injury. 2004;35 Suppl 2:SB77–SB86.
Tham W, Sng S, Lum YM, Chee YH. A Look Back in Time: Sir Robert Jones, ‘Father of Modern Orthopaedics’. Malays Orthop J. 2014;8(3):37–41. doi:10.5704/MOJ.1411.009
Thomas JL, Davis BC. Three-wire fixation technique for displaced fifth metatarsal base fractures. J Foot Ankle Surg. 2011;50:776–779.
______________________
LISFRANC SHOW NOTES:
Intro:
- Can’t miss diagnoses: needs stat ortho
- 20% miss rate
- Can be dislocation, fracture, fracture dislocation, or ligamentous injury
- Jacques Lisfranc in Napoleonic Wars: performed transmetatarsal amputation for midfoot gangrene
Anatomy:
- Lisfranc ligament: 3 ligaments that run from the base of the second metatarsal to the medial cuneiform bone. Helps attach the forefoot to the midfoot bones
- If ligament complex gets disrupted, can end up with chronic deformity and disability
Injury definitions:
- Dislocation: widening between base of 1st and 2nd metatarsal, or between cuneiforms
- Fracture dislocation: associated fracture, most commonly at the base of the proximal second metatarsal
Physical Exam:
- Pain and swelling in midfoot
- Pain elicited with passive abduction and pronation of the midfoot while holding heel steady
- Plantar ecchymosis
- r/o compartment syndrome
- Feel for DP pulse!
Diagnosis:
- XRs: AP, lateral, oblique, stress views with weight bearing
- Watch out for “fleck sign”
- Consider CT if pt cannot bear weight, or even if XR negative and high suspicion
Treatment:
______________________
THANKS TO DANNY PURCELL, MD and MAY LI, MD