Background
This analysis was originally posted on REBEL EM here
Endotracheal intubation is a common occurrence in the Emergency Department (ED). Many patients requiring airway management are at a higher risk of hypoxia due to deranged respiratory physiology (i.e. decreased functional residual capacity and/or increased shunt fraction). Advocates of VL argue that it provides better visualization of the airway anatomy, but it is less clear if better visualization correlates with better patient oriented outcomes. Good preparation, pre-oxygenation, and having a plan A, B, and C prior to intubation are essential requirements in 1st pass intubation success rate and decreased intubation time.
Clinical Question
What is the clinical efficacy of VL in comparison to DL in ED airway management?
Design
Meta-analysis and systematic review of randomized controlled trials of adults intubated in the ED
Literature Search
PubMed (1946 to 20th October 2017) and The Cochrane Central Register of Controlled Trials (CENTRAL) were searched for potentially eligible trials on 20th October 2017.
Outcomes
Primary: First pass intubation success rate
Secondary:
- Overall intubation success rate
- In-hospital mortality
- Esophageal intubation rate
Inclusion
Randomized controlled trials of adults intubated in the ED
Excluded
- Trials on cadavers
- Trials on manikins
- Simulated reviews
- Non-English publications
Primary Results
- 1250 patients from 5 RCTs
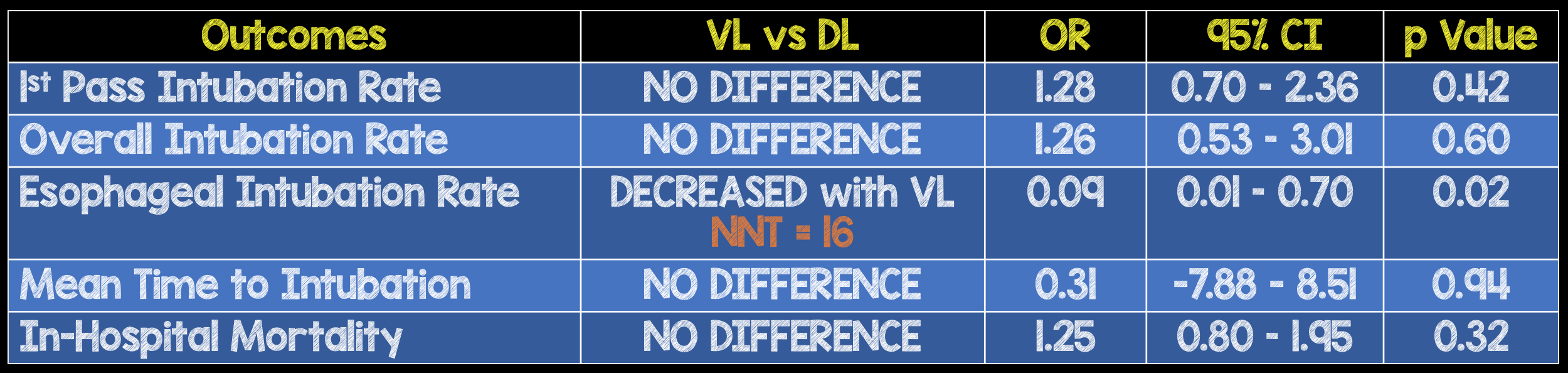
|
Outcomes |
VL vs. DL |
OR |
95% CI |
p value |
| 1st Pass Intubation Rate |
NO DIFFERENCE |
1.28 |
0.70 – 2.36 |
0.42 |
| Overall Intubation Rate |
NO DIFFERENCE |
1.26 |
0.53 – 3.01 |
0.60 |
| Esophageal Intubation Rate |
DECREASED with VL NNT = 16 |
0.09 |
0.01 – 0.70 |
0.02 |
| Mean Time to Intubation |
NO DIFFERENCE |
0.31 |
-7.88 – 8.51 |
0.94 |
| In-Hospital Mortality |
NO DIFFERENCE |
1.25 |
0.80 – 1.95 |
0.32 |
Strengths
- Asks a clinically important, patient centered question
- A number of databases were reviewed for appropriate articles (Cochrane, PubMed CENTRAL etc)
- Included on only RCTs
- Followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)
- Cochrane questions were used to assess methodological quality of included studies
Limitations
- The protocol for this meta-analysis was not registered
- There was no blinding of participants and personnel in the individual studies potentially causing a performance bias
- First pass success (primary outcome) was not uniformly defined across studies
- All included studies were small
- There is a wide range of heterogeneity most likely due to differences in patients and operator expertise levels
- Incidence of hypoxemia was only reported in one trial and therefore not able to be evaluated in this meta-analysis
- Most of the included studies excluded patients with potentially difficult airways. It is this population where VL may have an advantage over DL.
Other Issues
- In the 5 trials included, 3 trials were a comparison of C-MAC VL vs the Macintosh blade and in the remaining 2 trials Glidescope VL vs the Macintosh blade were compared. It is important to note that not all VL devices are the same (i.e. hyperangulated Glidescope vs standard geometry Glidescope/C-MAC)
- Potential reasons why VL was not superior to DL:
- Limited experience with VL
- RSI medications may not have been optimal during emergency intubation
- VL may have had a poorer alignment of oral, pharyngeal and laryngeal axes
Author's Conclusions
“Use of video laryngoscopy for emergency endotracheal intubation in adult patients is associated with reduced oesophageal intubation over direct laryngoscopy. However, no benefit was found in terms of overall intubation success.”
Our Conclusions
We agree with the author’s conclusions. VL was not found to be superior to DL in terms of 1st pass success in this study. Although there is no difference in 1st pass intubation rate, overall intubation rate, time to intubation, and in-hospital mortality, all of which are clinically important outcomes when comparing video laryngoscopy to direct laryngoscopy, better airway anatomy visualization with video laryngoscopy does reduce esophageal intubation rate compared to direct laryngoscopy.
Potential Impact To Current Practice
The results of this study do not impact clinical care.
Bottom Line
There is no perfect device for intubation and the skill of the operator is more important than the tool being used. Clinicians should train with both VL and DL techniques and use the tool best suited to the airway at hand.
