Background
In critically ill patients, fluid status is a balancing act. Too little fluid resuscitation can lead to end organ hypoperfusion, while too much fluid resuscitation can lead to pulmonary edema and respiratory compromise. In some situations, it is difficult to differentiate who will benefit from more fluids and who will be fluid unresponsive or even require fluid restriction.
This article put forth two goals:
1) Review of current literature on Point of Care Ultrasound (POCUS) of IVC and Lungs to assess fluid status
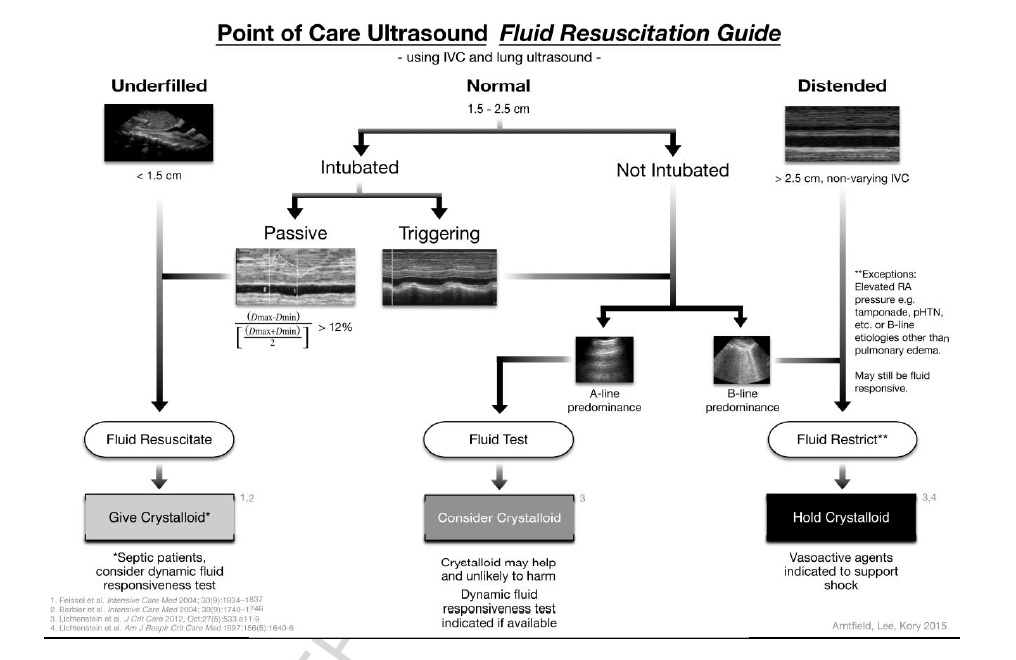
2) To create an algorithm, based on POCUS of IVC and lung fields to sort patients into 3 categories: fluid resuscitate, fluid test, fluid restrict
Lit review summarized in article:
- IVC distensibility (evidence in vented patients only):
- Barbier et al: distensibility index: (Dmax-Dmin)/Dmin x 100%. Threshold of 18% has 90% sensitivity and specificity for volume responsiveness.
- Feissel et al: respiratory variation in IVC diameter: (Dmax-Dmin)/((Dmax+Dmin)/2). Threshold of 12% predicted fluid responders with a PPV of 93% and NPV of 92%
- IVC diameter (evidence in all patients):
- Meta analysis of studies measuring IVC size in shock patients found all had IVC <15mm
- Feissel et al found that 29 of 30 fluid non-responders had IVC>15mm, 2 of 16 fluid responders had IVC>25mm
- IVC collapsiblity (evidence in non-vented patients):
- Muller et al: respiratory variation = (Dmax-Dmin)/Dmin x 100%. If greater than 40%, then usually volume responsive, if under 15% then usually not volume responsive
- Lung:
- FALLS protocol: A-line predominance indicates dry interlobular septa and low or normal left atrial pressure. B-line predominance associated with alveolar-interstitial syndrome: usually pulmonary edema, however may be malignancy, interstitial disease, or other processes.
- A-line predominance predicts patient will be fluid responsive, B-line predominance predicts patient will not be non-fluid responsive
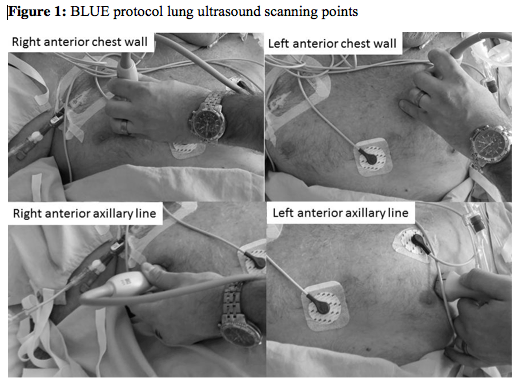
- BLUE protocol suggested to standardize approach to scanning lungs
Primary Results
Proposed Algorithm:
- Repeated use of algorithm encouraged to monitor patient’s dynamic status
Limitations
- Lack of mandated ultrasound exam of heart as part of algorithm
- Provider must understand situations in which IVC diameter may not be a reliable gauge of fluid status such as increased intraabdominal pressure, tamponade, pulmonary hypertension, high PEEP, and unconventional modes of ventilation such as oscillation
- Algorithm currently lacks prospective validation
Author's Conclusions
“Combining both IVC and lung POCUS is easy to accomplish and provides valuable information for determination of fluid responsiveness.”
Our Conclusions
POCUS use is rapidly gaining momentum for a variety of clinical tasks, and clinicians are becoming more comfortable with its uses. We agree that this algorithm is feasible in the ED and can add valuable information to the evaluation of critical patients. Though prospective validation is still lacking, incorporating it into practice to help guide (though not determine) a course of action makes sense based on existing evidence.
Potential Impact To Current Practice
As emergency physicians continue to become more comfortable with POCUS, there is little doubt that this algorithm, or a revised version, will become a routine part of clinical evaluation of critical patients.
Bottom Line
Based on the existing literature, this algorithm creates a reasonable approach to assessing volume status and volume responsiveness in patients. As with any algorithm, it should be integrated into the entire clinical picture.
is there any other article on POCUS + cardiac US results/ thank you
In many cases, diagnostic ultrasound is found to be an accurate and reproducible tool compared to conventional tests.
i read the artcle. but in our icu we have seen few pt with collpased IVC with Blines and marginally depressed EF . How to approach such pt . should we measure LVEDpressure to asses whether she will toleratw fluids or not. is there any way or other approach.