Background
Fever without source in infants less than three months old presents a difficult diagnostic dilemma for ED physicians. Over the past 25 years several algorithms have been developed to help guide clinicians, most notably the Rochester, Philadelphia and Boston Criteria, in determining which infants require admission vs. outpatient management. These studies were designed published between 1992 and 1994 prior to the wide spread use of HiB and pneumococcal vaccines in children, maternal GBS screening and the development of many new biomarkers.
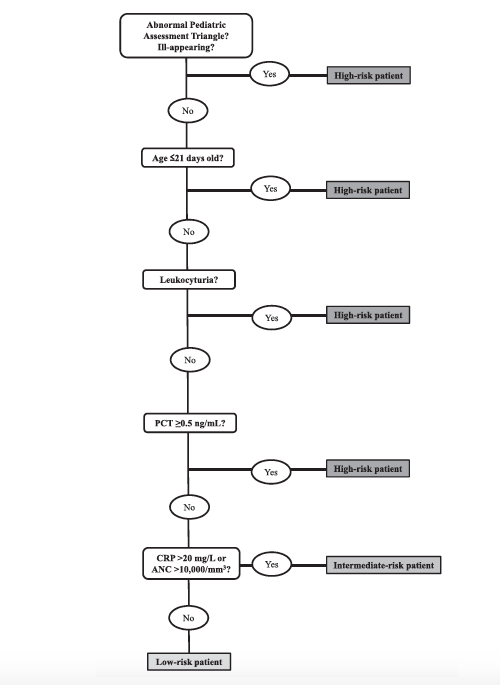
The “Step-by-Step” approach was developed by a European group of pediatric emergency physicians with the objective of identifying low risk infants who could be safely managed as outpatients without lumbar puncture or empiric antibiotic treatment. The algorithm was designed using retrospective data and this study attempts to prospectively validate it.
Clinical Question
How does the “Step-by-Step” approach compare to the Rochester criteria or the “Lab-score” method in identifying infants 90 days or younger with a fever of unknown source to be at a low risk of invasive bacterial infections?
Population
Infants 90 days old or younger with “fever without a source” defined as objective temperature of > 38C at home or in the ED without a clear source on history or physical exam, more specifically pulmonary exam findings or history of diarrhea.
Intervention
Application of the “Step-by-Step” approach (detailed below)
Control
The step-by-step approach was compared against two established algorithms (Rochester and the Lab Value algorithm) for assessing the febrile infant (detailed below)
Outcomes
Detection of an invasive bacterial infection (IBI) defined by having a positive blood culture or positive CSF or non-IBI defined as infant with positive stool or urine cultures but without positive blood or CSF cultures.
Design
Multi-center prospective study including 11 European pediatric emergency departments (8 Spanish, 2 Italian and 1 Swiss).
Excluded
Patients without fever in the ED and only subjective fevers at home
Clear source of fever identified on careful history and physical exam
Absence of 1 or more of the mandatory ancillary tests (Blood culture, Urine Culture, Urine dipstick, PCT, CRP or WBC)
Refusal of the parents to consent
Primary Results
Step-By-Step Algorithm
- 2635 infants 90 days or younger with a fever without source
- 177 (6.7%) visits the study was either not offered or the parents refused
- 273 (10%) visits lacked the appropriate data
- 2185 (83%) infants were enrolled in the study
- Diagnosed with a bacterial infection: 504 (23.1%)
- IBI: 87 patients (3.9%)
- non-IBI: 417 patients (19.1%)
Critical Results
| Sensitivity | Specificity | PPV | NPV | (+) LR | (-) LR | |
| Rochester Criteria | 81.6% (72.2-88.4) | 44.5% (42.4-46.6) | 5.7% (4.6-7.2) | 98.3% (97.3-99.0) | 1.47 (1.32-1.64) | 0.41 (0.26-0.65) |
| Lab-Score | 59.8% (49.3 – 69.4) | 84.0 (82.4-85.5) | 13.4% (10.4-17.2) | 98.1 (97.3-98.6) | 3.74 (3.07-4.56) | 0.48 (0.37-0.62) |
| Step by Step | 92.0% (84.3-96.0) | 46.9 (44.8-49.0) | 6.7% (5.4-8.3) | 99.3 (98.5-99.7) | 1.73 (1.61-1.85) | 0.17 (0.08-0.35) |
- 6 of the 7 IBIs missed by the “Step-by-Step” approach had fevers for <2 hours and in 3, fever was not the primary complaint but instead first noticed in the ED
- 4 out of 7 IBIs missed by the “Step-by-Step” approach were in the 21-28 day old range
Strengths
- Well conducted multicenter prospective study
- Seeks to validate a retrospectively derived tool
- Follow up was sufficiently long and complete
- The effect was large enough and precise enough to be clinically significant
Limitations
- Absolute bands, a metric in the Rochester criteria, was not available in all patients
- The rule includes subjective criteria, “Abnormal pediatric assessment triangle” & “Ill-appearing” without inter-rater reliability comparison
- The availability of procalcitonin is not currently universal, limiting the applicability of the study
- Data collected in 11 European Pediatric Emergency Departments therefore the use in other patient populations or settings other then dedicated pediatric EDs should be cautioned.
- Prevalence of SBI was similar to previous European studies but higher then those reported in US studies, specifically the rate of UTIs
- The “Step-by-Step” approach was not compared to the Philadelphia criteria, the most used criteria in the US (20% of practioners) due to the need to LP all infants under 60 days
- Rochester study was designed to screen infants younger then 60 days (not 90)
Author's Conclusions
“ We validated the Step by Step as a valuable tool for the management of infants
with fever without source in the emergency department and confirmed its superior accuracy in identifying patients at low risk of IBI, compared with the Rochester criteria and the Lab-score.”
Our Conclusions
The febrile infant can be a diagnostic/management challenge for the emergency medicine physician. The “Step-by-Step” approach to identifying infants at risk for potentially life threatening invasive bacterial infections has a 92.0% & 99.3% sensitivity and negative predictive value making it a reliable clinical decision instrument which can avoid invasive studies such as lumbar punctures. The study found that its sensitivity is primarily limited by onset of fever, specifically fevers starting <2 hours from presentation. When factoring this into detecting infants at risk for IBIs a sensitivity of 99.9% can be achieved.
Bottom Line
The Step-by-Step approach to assessing febrile infants has excellent sensitivity and NPV but should be used with caution in infants presenting within 2 hours of onset of fever and in infants 21-28 days of age.
Read More
SGEM # 171: Step-by-Step Approach to the Febrile Infant