Background
In patients with subarachnoid hemorrhage, one of the major early complications is rebleeding, with reported incidences ranging from 8% to 23% in the first 72 hours (Larsen 2010). If repair of the ruptured aneurysm is performed successfully in a timely fashion, the chance of rebleeding can be decreased, thereby decreasing morbidity and mortality in these patients. Traditionally, the time to aneurysm repair is set at < 72 hours after ictus (van Donkelaar 2015), but there may be potential benefit to performing repair early if it is known which patients are at increased risk for rebleeding. Early rebleeding is defined as rebleeding occurring within 24 hours after ictus. This study aimed to identify predictive risk factors for early rebleeding in relation to time after ictus.
Clinical Question
What are the predictors for early rebleeding after an aneurysmal subarachnoid hemorrhage?
Population
Patients with aneurysmal SAH in the Netherlands from 1998 to 2004 presenting to a single university neurovascular center. There was a change in standardized protocol during this time: before 2002, patients had digital subtraction angiography < 12 hours, and after 2002, patients had immediate CTA followed by digital subtraction angiography < 48 hours if they have negative CTA.
Outcomes
Primary: In-hospital rebleeding < 24 hours after the ictus Secondary: rebleeding < 72 hours There were different ways of detecting the outcome. In awake patients, clinical deterioration was monitored based on a decrease in GCS. In sedated patients, clinical deterioration was monitored based on change in blood pressure, pupil size, or fresh blood coming out of the CSF drainage system.
Design
Retrospective analysis of data that was collected prospectively
Excluded
Patients were excluded if they had non-aneurysmal bleeds, such as fusiform, dissection, non-saccular, or if they had prior SAH.
Primary Results
- 1205 patients enrolled
- 70 out of 1205 patients had rebleeding < 24 hours
- 11 out of 906 patients had rebleeding between 24 and 72 hours
- 46 patients with rebleeding died
- 100% follow up
Critical Findings
- Predictors associated with rebleeding < 24 hours
- Hypertension (defined as > 140/90 mmHg during multiple recent measurements or controlled using antihypertensive drugs)
- World Federation of Neurosurgeons Score (WFNS) at admission
- Larger aneurysm size
- Presence of intracerebral hematoma
- High mFisher grade (a score looking at the aneurysm characteristics)
- External CSF drainage before repair
- Statistically significant independent predictors associated with rebleeding < 24 hours after multivariate analysis
- mFisher grade of 3 or 4
- Adjusted HR = 4.7 (95% CI: 2.1 – 10.6)
- NNT = 15 (95% CI: 10-25)
- External CSF drainage
- Adjusted HR = 1.9 (95% CI: 1.4-2.5)
- Aneurysm diameter (> 20 mm)
- Adjusted HR = 4.4 (95% CI: 1.6 – 13.2)
- mFisher grade of 3 or 4
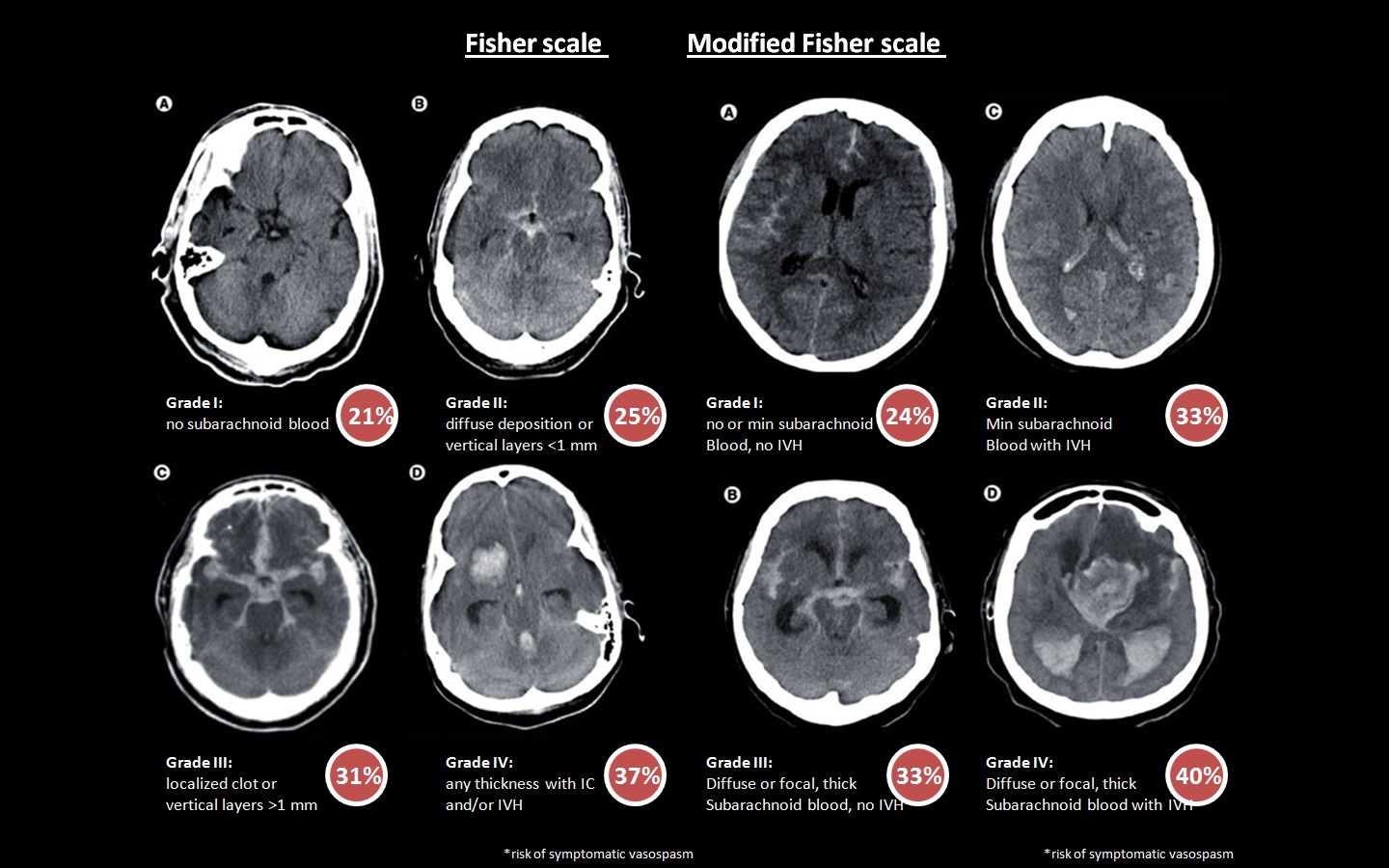
Fisher and Modified Fisher Scale in SAH (pbrainmd.wordpress.com)
Strengths
- Relatively large study population over a long period of time
- Investigate an important clinical question that may impact patient outcome
Limitations
- Analyses were performed retrospectively
- Not all previously reported predictors for a rebleeding could be assessed, including missing imaging at the time of data analysis
- Single institution
- Patients may have rebleeding without clear signs or with subtle signs that may not have been noticed, therefore possibly affecting the consistency of the data collected
Author's Conclusions
“In our opinion, timing of treatment of aSAH patients, especially those with an modified Fisher grade of 3 or 4 in a good clinical condition, should be reconsidered. These aSAH patients might be regarded a medical emergency, requiring aneurysm repair as soon as possible. In this respect, our findings should provoke the debate on timing of aneurysm repair, especially in patients considered to be at high risk for rebleeding.”
Our Conclusions
While this is an important study highlighting the statistically significant predictors associated with early rebleeding, there needs to be more investigation into whether early repair can improve patient outcomes in patients that are at higher risk for rebleeding.
Potential Impact To Current Practice
This study suggests that there are important predictors associated with rebleeding in aneurysmal SAH. Therefore, patients with these predictors should be candidates considered for early repair to potentially prevent rebleeding.
Bottom Line
For patients with aneurysmal SAH with a high mFisher grade, external CSFS drainage, or large aneurysm diameter, consider mobilizing neurosurgery and IR teams to take these patients for early repair (within 24 hours if possible).
Read More
References
Van Donkelaar CE et al. Predictive Factors for Rebleeding After Aneurysmal Subarachnoid Hemorrhage. Stroke. 2015; 46(8):2100-06. PMID: 26069261
Larsen CC et al. Rebleeding After Aneurysmal Subarachnoid Hemorrhage: a Literature Review. World Neurosurg. 2013; 79(2):307-12. PMID: 22722033
There is little reason to not secure these aneurysms early (unless the patient should be palliative care and that is not always easy to determine early on). Get the team out of bed and fix the thing.