Background
Prehospital trauma team activation criteria allow for prompt mobilization of personnel and resources. Prehospital hypotension is one of those criteria. Pulse pressure is the difference between systolic and diastolic blood pressure. This is variously defined as a difference of 30-40 mmHg. A narrow pulse pressure occurs due to compensatory increased systemic vascular resistance in the setting of decreased cardiac output. A narrow pulse pressure has been shown to predict the need for hemorrhage control in the ED setting but has not been assessed as a predictor in the prehospital setting.
Clinical Question
In trauma patients, 16-60 years of age, presenting to a level one trauma center, is a prehospital narrow pulse pressure (< 30 mmHg) with a systolic blood pressure of > 90 mmHg, associated with in-hospital mortality, need for a resuscitative thoracotomy, need for an emergent intervention (NFEI), need for a trauma intervention (NFTI) and mortality?
Design
Observational: Retrospective Cohort
POPULATION:
Inclusion:
- Age 16-60 years
Exclusion:
- Age < 16 (lower BP range) or < 60 years (higher BP range)
- Unrecorded prehospital vital signs
- Transferred from an outside hospital
- On-scene cardiac arrest
- Missing discharge disposition
Setting:
Single Level I Trauma Center (Trauma registry data), (1/2008-5/2020)
EXPOSURE:
- Narrow pulse pressure (PP): Systolic BP 90 mmHg AND PP < 30 mmHg
- (PP = Systolic BP – Diastolic BP)
- Hypotensive: Systolic BP < 90 mmHg (regardless of pulse pressure)
NO EXPOSURE:
- Normotensive: Systolic BP 90 mmHg AND Pulse Pressure 30 mmHg
OUTCOMES:
- Resuscitative thoracotomy
- Mortality
- Need For Emergent Intervention (NFEI): Transfer directly from the ED to the:
- Operating room
- Interventional radiology
- Need For Trauma Intervention (NFTI): 1 of the following:
- Packed red cell transfusion < 4 hours after arrival
- Need for operative intervention or angioembolization < 90 minutes of arrival
- Admission to the ICU from the ED with LOS ≥ 3 days
- Mechanical ventilation initiated within 72 hours of arrival
Primary Results
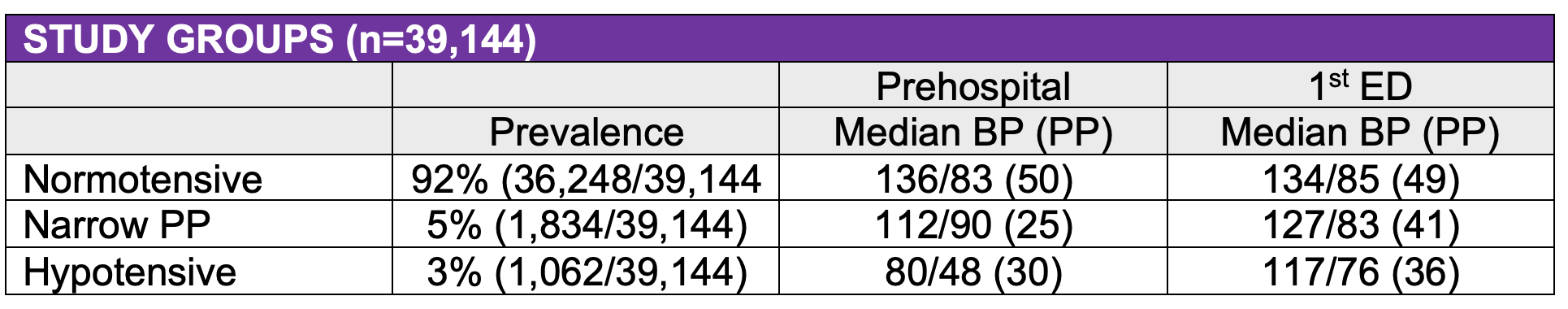
Univariable Analysis: patients with a narrow pulse pressure were intermediate in risk of:
- resuscitative thoracotomy, need for trauma intervention, need for any operative intervention, central line insertion, chest tube insertion, and mortality compared to normotensive patients and hypotensive groups
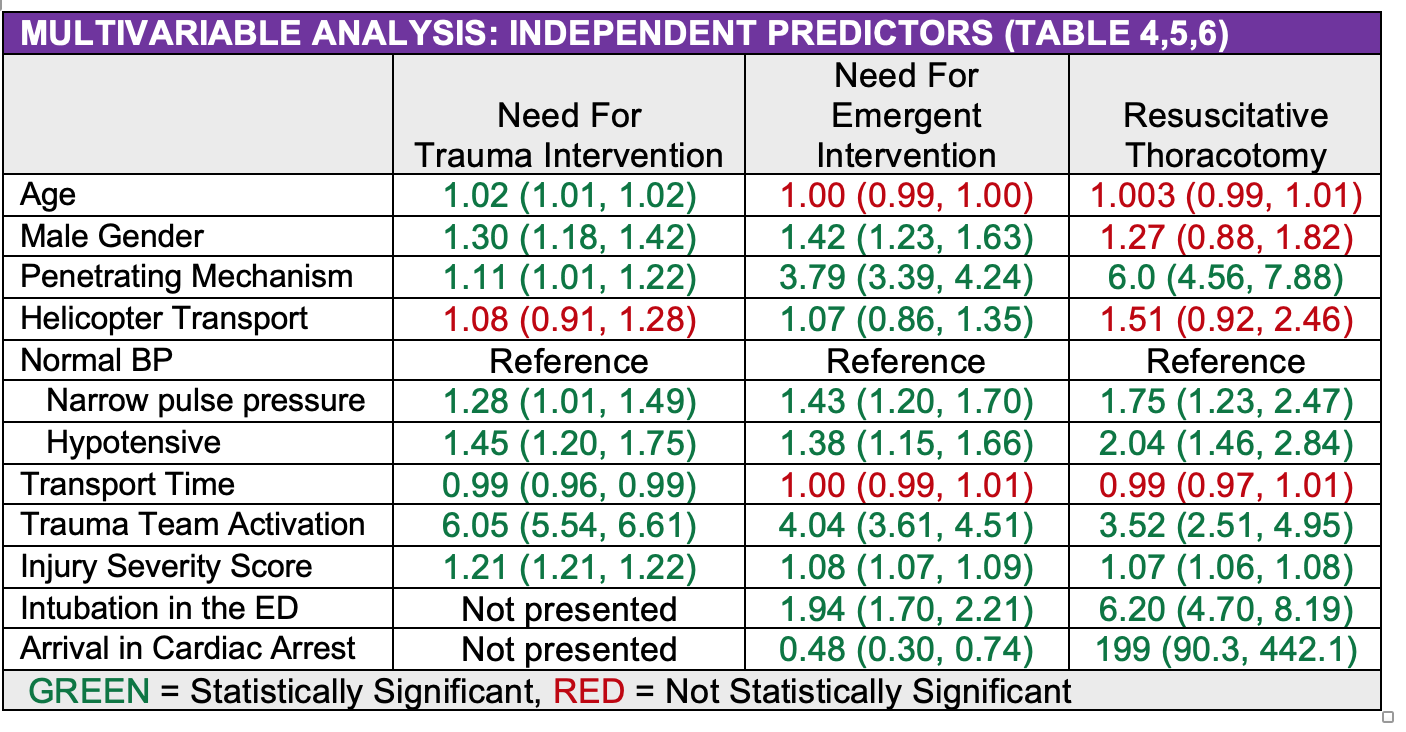
Multivariable Analysis:
- A narrow pulse was an independent predictor of the need for a trauma intervention (aOR 45, 95% CI (1.20, 1.75)), the need for resuscitative thoracotomy (aOR 2.04 95% CI (1.46, 2.84)) and the need for an emergent intervention (aOR 1.38, 95% CI (1.15, 1.66)).
- A narrow pulse was not an independent predictor of mortality (p value 0.15, aOR 1.31 with 95% CI not presented).
- A penetrating mechanism, trauma team activation and injury severity score were also independent predictors of all three outcomes.
Strengths
- Large sample size though
-
- High percentage excluded due to missing data (? Selection bias)
- Only 5% with narrow pulse pressure
- Mean blood pressure on ED arrival was normal with a normal pulse pressure in the narrow pulse pressure group, strengthening its predictive ability (not just a marker for ED narrow pulse pressure)
- Regression analysis to account for baseline difference in blood pressure groups
- Trauma registry data prospectively collected though retrospective analysis
- BP groups mutually exclusive and collectively exhaustive
Limitations
- Single center with high proportion of penetrating trauma
-
- Subgroup analysis penetrating vs blunt would have been helpful
- Generalizability to centers with less penetrating trauma, non-level one trauma centers, pediatric and geriatric patients is unclear
- NTEI and NFTI are composite outcomes. Results for individual outcomes that make up the composite are not provided
- There was no table for the multivariable analysis primary outcome of in-hospital mortality.
Author's Conclusions
“As we continuously seek methods to improve our care of the injured patient, prompt control of hemorrhage to reduce morbidity and mortality remains one of the central tenets of trauma surgery. For this reason, appreciation of early indicators of blood loss are invaluable. In the current study, narrow pulse pressure in the field was independently associated with the need for resuscitative thoracotomy, emergent intervention for hemorrhage control, and the presence of major traumatic injuries. We propose that narrow pulse pressure be further studied in the future as a possible addition to existing American College of Surgeons Committee on Trauma prehospital trauma team activation criteria.”
Our Conclusions
Prehospital narrow pulse pressure with a systolic blood pressure > 90 mmHg was an independent predictor of resuscitation thoracotomy, need for emergent intervention and need for trauma intervention but not in-hospital mortality. A subgroup analysis by trauma mechanism (blunt vs penetrating) would have been helpful as penetrating trauma patients were more likely to have a prehospital narrow pulse pressure.
Potential Impact To Current Practice
A pre-hospital narrow pulse pressure could serve as a marker of intermediate risk when compared to normotensive and hypotensive patients and prompt mobilization of personnel (e.g. trauma team activation) and resources (e.g. initiation of a massive transfusion protocol). A prospective, multicenter study to examine the impact of a narrow pre-hospital pulse pressure on trauma interventions and outcomes would validate its importance and improve the study’s generalizability.
Read More
EMCAR – Prehospital Traumatic Narrow Pulse Pressure – J Surg Res 2021
