Background
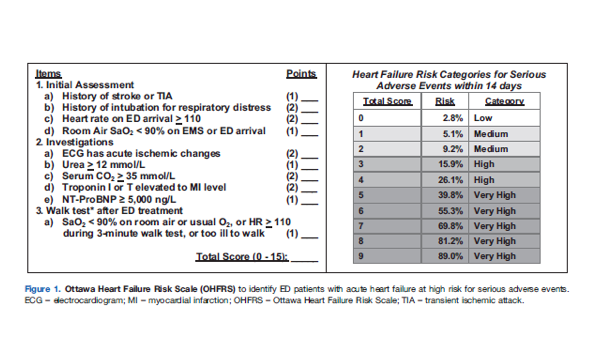
In the United States, heart failure affects 5.7 million people. Acute heart failure exacerbation is a common ED presentation and 1 in 9 deaths in the US included heart failure as a contributing cause. Each year it contributes to more than 1 million hospitalizations, and while in the past almost all patients with acute heart failure exacerbations were admitted, today many are treated in the ED and discharged. The ED provider is faced with the challenge of identifying and hospitalizing all the patients who are going to have a bad outcome, while at the same time avoiding unnecessary admissions and increasing healthcare costs. Currently, there is no established guidelines on who should be admitted versus discharged. Previous work from this group derived the Ottawa Heart Failure Risk Scale (OHFRS), which uses clinical variables to estimate the probability of an adverse event in a patient presenting with acute heart failure exacerbation. In this study, the group applies the OHFRS to patients to see if it can truly identify those patients with an impending bad outcome.
Clinical Question
Is the Ottawa Heart Failure Risk Scale (OHFRS) able to identify patients that require admission for acute heart failure exacerbation based on the rate of serious adverse outcomes in 30 days?
Population
Adults over 49 years old, who presented to six Canadian teaching hospitals, between 8AM and midnight, with shortness of breath due to acute heart failure. Heart failure was defined as having appropriate symptoms, with signs of fluid overload, in a person with underlying cardiac function abnormality.
Outcomes
Primary: Serious Adverse Events (SAE)
Death from any cause within 30 days of ED visit
Any of the following within 14 days: Admission to monitored setting, Intubation or NIV after admission, Myocardial infarction, Major procedure (CABG, PCI, cardiac surgery or new HD), Relapse for related problem and admission
Secondary: Physician accuracy in interpretation of OHFRS, Performance of OFHRS with and without NT-proBNP, Acceptability
Design
Prospective, multi-center, observational, cohort
Excluded
Shortness of breath for 7 days or more or too ill to be considered for discharge.
Oxygen saturation <85% at rest on baseline O2 supplement, Heart rate >120 bpm, Systolic BP <85 mm Hg, confusion/disorientation/dementia, acute ischemic ST changes, STEMI, expected death within weeks from chronic illness, nursing home, on HD, enrolled in the past 2 months
Primary Results
- 4999 patients presented with shortness of breath
- Enrolled 1100 based on inclusion criteria
- 1098/1100 (99.8%) patients were followed up in 30 days
- 57% of patients were admitted, 43% of patients discharged home
- NT-proBNP (part of the OHFRS) measured in 62.2% of patients
Critical Findings:
- Serious Adverse Event Rate (Primary Outcome)
- Overall: 15.5%
- Admitted patients: 19.4%
- Discharged patients: 10.2%
- Mortality (Primary Outcome): 3.7%
- Physician discomfort with the OHFRS (Secondary Outcome): 11.9% of cases
Ottawa Heart Failure Risk Scale
|
# patients |
SAE % |
Sensitivity % |
Specificity % |
Admission% |
|
| Current Practice |
1100 |
15.5 |
71.8 |
45.5 |
57.2 |
| OHFRS Score | |||||
| 1 |
323 |
10.8 |
91.8 (86.6-95.2) |
24.9 (24.0-25.6) |
77.6 |
| 2 |
219 |
13.7 |
71.2 (64.2-77.4) |
55.9 (54.6-57.0) |
48.3 |
|
# patients |
SAE % |
Sensitivity % |
Specificity % |
Admission% |
|
| Current Practice |
684 |
17.4 |
69.8 |
41.1 |
60.8 |
| OHFRS Score With NT-proBNP | |||||
| 1 |
171 |
11.1 |
95.8 (90.5-98.4) |
13.6 (12.5-14.2) |
88 |
| 2 |
148 |
12.2 |
79.8 (72.0-86.2) |
40.5 (38.9-41.9) |
63 |
Strengths
- Study not only addressed patient centered outcomes, but also looked at ED providers’ perception of the tool and ability to accurately use it, which is important to implementation
- Researchers calculating the true OHFRS score were blinded to outcome
- Prospective, real-time data collection
- Follow-up was near complete at 30 days
Limitations
- Study sites were all in Canada, where only 40-60% of acute heart failure exacerbation patients are admitted, compared to the US where admission rate is ~ 80%
- There were two primary outcomes
- Convenience sample: did not enroll patients that arrived off business hours or when the clinician was too busy
- A large number of patients (63%) were excluded limiting generalizability of the study
- Acute ischemic ST changes were an exclusion criteria but also a variable in the OHFRS
- Follow up data was near complete but mostly done by phone or by health records instead of in person
- Physician interpretation of risk category was poor
- Use of the scale in disposition decision making would likely lead to an increase in hospitals admissions
- There’s no evidence that admitting these patients (as opposed to discharge) will result in better outcomes (I.e. are we able to help the higher risk patients)
Author's Conclusions
“Prospective clinical validation found the OHFRS tool to be highly sensitive for SAEs in acute heart failure patients, albeit with an increase in admission rates. When available, NT-proBNP values further improve sensitivity. With adequate physician training, OHFRS should help improve and standardize admission practices, diminishing both unnecessary admissions for low-risk patients and unsafe discharge decisions for high-risk patients.”
Our Conclusions
In this study, accurate application of the OHFRS with a threshold score of 1 would identify more high-risk patients, but will increase admissions compared to current practice. A threshold score of 2 (with NT-proBNP), would identify more high-risk patients (~80%) compared to current practice without significant increase in the admission rate. But the 5% risk of having a SAE after discharge, when using a threshold of 2 for admission, may be an unacceptable rate in the US. It is also unclear whether application of this tool in disposition decision-making will prevent adverse events.
Potential Impact To Current Practice
The OHFRS score could be used to describe risk and aid in shared decision-making for those patients with medium risk (score 1). It can also be used as an additional data-point to validate admission for patients (score 2 or greater translates to 9% or greater risk).
Bottom Line
OHFRS is useful to discuss risk with patients and hospitalists. Further research, in the United States, looking at the effect of OHFRS application on patient outcomes, is needed before using it to determine if patients should be admitted versus discharged.
Read More
Read More
The SGEM: SGEM #170: Don’t Go Breaking My Heart – Ottawa Heart Failure Risk Scale
First 10EM: The Ottawa Heart Failure Risk Scale