Background
GRACE Background
- The GRACE guidelines – “Guidelines for Reasonable and Appropriate Care in the Emergency Department” – are a Society for Academic Emergency Medicine (SAEM) program designed to “reduce wasteful testing, provide explicit criteria to reduce foreseeable risk, and define sensible and prudent medical care”. The GRACE-1 guidelines were about chest pain, and the GRACE-2 guidelines were about abdominal pain.
- GRACE guidelines are written by a diverse group of clinicians with content expertise. GRACE-3 guidelines included emergency physicians, oto-neurologists, neuro-otologists, and patient advocates.
Dizziness Background
- Acute dizziness represents ~1-3% of ED visits and has a disproportionately high cost, resource use, and length of stay, largely due to imaging (much of which is unnecessary).
- Only about 3.2-6% of patients presenting with dizziness had central causes whereas the rest had cardiac, orthostatic, peripheral vestibular, otological processes.
- Roughly 9-10 times as many patients with dizziness get a CT as those who get an MRI, even though CT is likely only about 10% sensitive in diagnosing a stroke, while MR is up to 95% sensitive.
- The subjective-description paradigm taught in medical school, e.g., “world-spinning” vs. “lightheadedness” vs. “imbalance,” developed in the early 1970s, while commonly used today, is a poor predictor of central vs. peripheral cause. Studies have shown that patients’ descriptions of their symptoms can frequently switch between these categories every few minutes.
GRACE-3 Population of Interest
- Adult ED patients with dizziness present less than 2 weeks and without an apparent medical or neurological cause of dizziness.
GRACE-3 Methodology: GRACE-3 team consisted of 18 members, including emergency physicians, otoneurologist, neuro-otologist, and patient advocates.
- All team members were trained on the Grading of Recommendations Assessment Development and Evaluation (GRADE) framework.
- This framework assesses literature and provides a systematic review and recommendations on a clinical subject.
- Based on the GRADE framework, recommendations are assigned direction “for, against, or either” and strength “strong or weak”.
- Medicare data was reviewed to assess direct costs for tests and procedures.
- The authors came up with 15 recommendations based on timing and triggers of dizziness.
GRACE-3 recommended paradigm for dizziness
The GRACE committee recommends a ‘’timing and triggers’’ categorization
- Acute vestibular syndrome (AVS) = acute onset of persistent and continuous dizziness lasting >24 hours
- Spontaneous episodic vestibular syndrome (s-EVS) = episodes of dizziness without a clear trigger
- Triggered episodic vestibular syndrome (t-EVS) = episodes of dizziness triggered by something, such as moving head
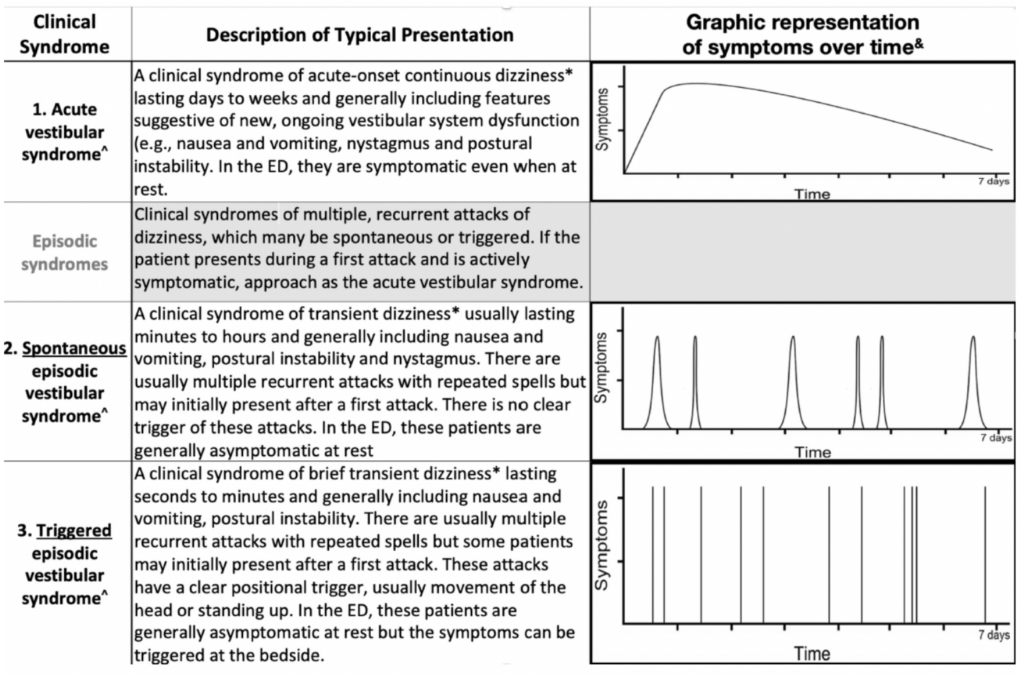
Figure 1 from cited article.
These clinical syndromes have been endorsed by experts over the last 15 years or so and lend itself to a convenient breakdown of differential diagnoses:
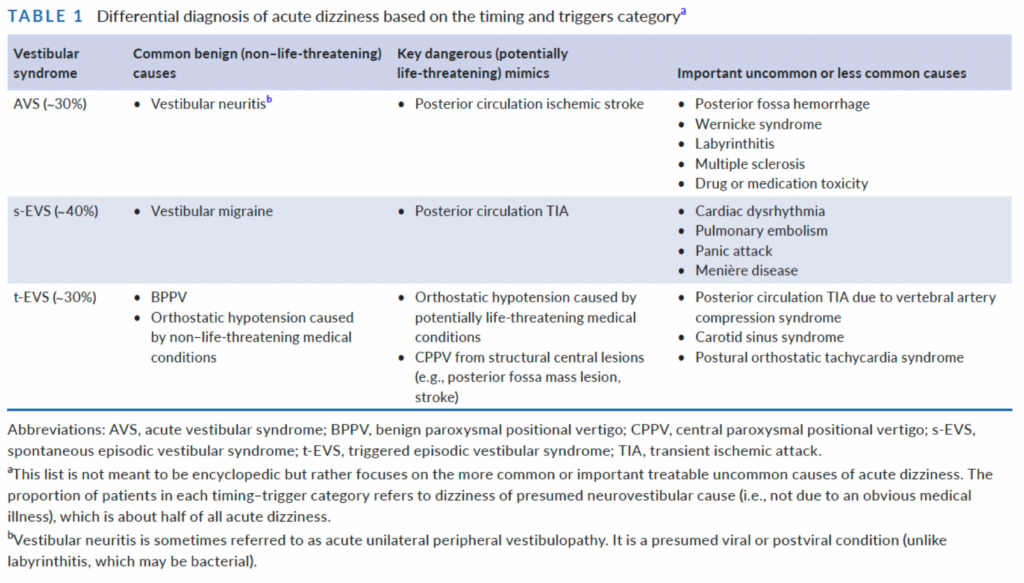 Table 1 from cited article.
Table 1 from cited article.
Strengths
- Assembles cohesive expert recommendations on a familiar yet confusing and contentious chief complaint.
- Gives strong recommendations, based on the evidence, that can be implemented at the systems level, i.e., additional training.
Author's Conclusions
Overarching GRACE-3 recommendation:
1. EM physicians should receive training in the HINTS exam, Epley, and Dix-Hallpike maneuvers.
Key official GRACE-3 recommendations regarding patients with AVS:
2. In patients with AVS with nystagmus, use HINTS to evaluate for peripheral vs. central causes.
- If HINTS exam suggests a central cause, obtain a Neurologic consult and initiate stroke evaluation.
- If HINTS exam suggests a peripheral cause, there is no need for further imaging.
- Recommend MRI if no clinician is available who is trained for HINTS
- Do not pursue CT/CTA; they have inferior sensitivity for posterior fossa abnormalities.
3. In patients with AVS, add on the “finger-rub” test for unilateral hearing loss.
4. In patients with AVS without nystagmus, do NOT do HINTS. Assess the degree of gait instability to help differentiate between peripheral(mild) and central(severe) etiologies
5. In patients with AVS with or without nystagmus, do NOT pursue CTs or CTAs to distinguish between central and peripheral etiologies.
6. In patients with AVS with nystagmus, HINTS (by a trained person) should be used before MRI for distinguishing central and peripheral etiologies
7. If the HINTS exam is equivocal in these patients or indicates a central etiology, use a stroke protocol MRI.
Comments: These recommendations are based on extensive data showing that the HINTs and Dix-Hallpike exams are better than any imaging available, and the Epley maneuver is better than medication. Furthermore, several studies show that EM physicians can perform these maneuvers with high sensitivity/specificity and efficacy if trained. HOWEVER, untrained EM physicians perform them incorrectly and use them in the incorrect clinical scenarios. They also recommend videos on acep.org/dizzy, and an iphone app from Hopkins developed specifically for GRACE-3 to assist with these exam maneuvers and in interpreting nystagmus.
Key official GRACE-3 recommendations regarding patients with s-EVS:
8. In patients with s-EVS, perform a thorough history and physical, focusing on the cranial nerves, (especially visual fields and eye movements), limb coordination, and gait to distinguish between central and peripheral etiologies.
9/10. In patients with s-EVS we should NOT use CT to distinguish between central and peripheral causes, but instead should use CTA or MRA to rule out posterior circulation vascular pathology if there is concern for TIA.
Comments: Even though symptoms of many TIAs may have already resolved on arrival, diagnosis is important since, if untreated, ~5% of patients will have a stroke in the coming days. Of the peripheral etiologies on the differential, vestibular migraine sufferers are about 5 times more common than patients with Meniere’s disease (Neuhauser 2009).
Key official GRACE-3 recommendations regarding patients with t-EVS:
11. EM physicians should receive training in the Dix-Hallpike and Epley maneuver since they work very well.
12. Do NOT use CT or CTA on these patients
13. In patients with t-EVS, use the Dix-Hallpike to diagnose BPPV. If the Dix-Hallpike is positive, do NOT obtain MRI or MRA.
15. In patients diagnosed with BPPV, use the Epley maneuver to treat them.
Comments: Central causes of positional / triggered vertigo AKA “CPPV” are very rare compared to BPPV. There are (at least) two types of BPPV, with posterior-canal being the most common. If the Dix-Hallpike maneuver is negative or evokes the wrong type of nystagmus in a patient with a strong suspicion for BPPV, they may have horizontal canal BPPV and require the Lempert “barbeque” roll instead of the Epley.
Key official GRACE-3 recommendations regarding patients with vestibular neuritis:
14. Use shared decision-making on whether or not to use steroids if patients present within 3 days of symptom onset.
Comments: All comparative studies have been underpowered and of limited quality. If given at all, the prescription should be for a short duration.
Bottom Line
- Forget about “What do you mean, ‘dizzy’?”. Instead, focus on timing and triggers of symptoms.
- Brush up your physical exam and maneuvers.
- Educational videos about dizziness and vertigo on Dr. Peter Johns channel (https://www.youtube.com/ c/peterjohns).
- Smartphone app on diagnosis and treatment of patients with acute dizziness created by GRACE-3 committee (https:// www.hopkinsmedicine.org/armstrong_institute/centers/center_for_ diagnostic_excellence/resources.html).
- HINTS exam is instrumental as an aid for dizziness diagnosis but is currently still not standard of care. Additional training is needed for EM physicians in how to accurately perform the HINTS exam.
- Stop obtaining non-contrast CT brain imaging for dizziness – if you’re concerned about a central cause of vertigo, obtain an MRI.

Nice summary!
And I agree with your gentle edits of the recommendations.
That is, in recommendation 4, and 6 to not use HINTS in patients without nystagmus.