Background
Acute congestive heart failure (AHF) results in nearly 1 million emergency department (ED) visits in the US per year and is associated with high morbidity, mortality, and cost. It is increasingly clear that ED management of these patients may determine later in-hospital mortality and ultimate prognosis.
Clinical Question
Does time from ED arrival to furosemide administration have an impact on in-hospital mortality in patients presenting with acute heart failure (AHF) exacerbation?
Population
Consecutive patients presenting to 9 university hospitals and 11 non-university teaching hospitals in Japan for first AHF exacerbation during August 2014 to December 2015. Patients were 20 years of age or older and received a diagnosis of AHF within three hours of arrival. AHF was diagnosed by the Framingham Criteria.
Outcomes
Primary: All-cause in-hospital mortality
Design
Prospective Multicenter Observational Cohort Study
Excluded
Patients who received treatment with IV medication prior to ED arrival, with previous heart transplantation, on dialysis (both peritoneal and hemodialysis), with acute myocarditis, with acute coronary syndrome requiring urgent or emergent revascularization. Missing B-type natriuretic peptide (BNP) or N-terminal-proBNP (NT-proBNP) or BNP < 100 pg/mL or NT-proBP < 300 pg/mL. Furthermore, while providers could select any diuretic medication, only patients who received IV furosemide were included in the present study. Patients must have received IV furosemide within 24 hours of ED arrival: door to furosemide (D2F) time of less than 24 hours in order to delineate patients treated for acute exacerbation vs decompensation after acute exacerbation.
Primary Results
- n = 1,682 patients met inclusion and passed exclusion criteria
- n = 1,291 (76.8%) patients with a D2F time of less than 24 hours
- n = 481 patients with a D2F time < 60 minutes
- n = 810 patients with a D2F time >= 60 minutes
Critical Findings
Percent In-Hospital Mortality of entire cohort and by Guidelines-Heart Failure Score Quartile
| Entire Cohort | Q1 | Q2 | Q3 | Q4 | |
| Early | 2.3%* | 1.3% | 0.9% | 0.9% | 6.5% |
| Late | 6.0%* | 1.8% | 3.5% | 4.7% | 14.2% |
*significant difference p = 0.002
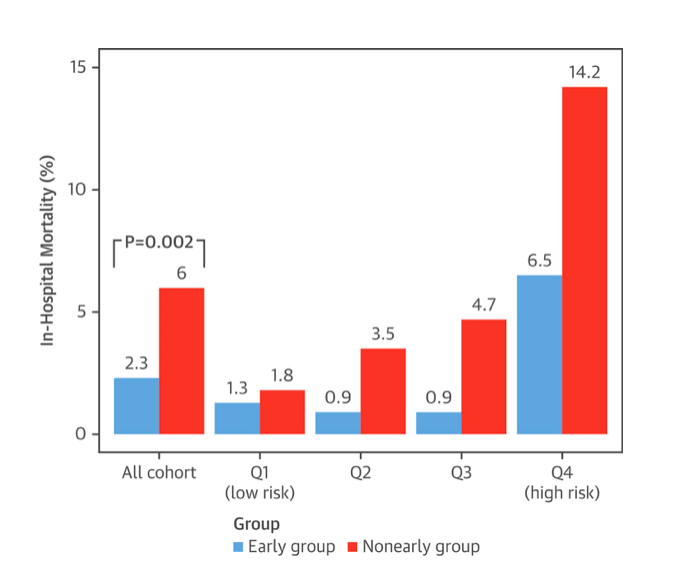
Trend across quartiles was significant for both groups p < 0.05
Strengths
- Multicenter: university hospitals as well as teaching community hospitals
- No patients were lost to follow up
- Investigators attempted to stratify patients by severity of illness in order to avoid confounder influence
- There was no difference in oral diuretic use between populations
Limitations
- The study is an observational study and not an RCT and so only associations and not causality may be gleaned from the results
- An RCT trial may not be ethically possible as patient’s treatment may not be reasonably delayed given risk of mortality
- The early treatment and late treatment groups are significantly different at baseline with early treatment patients demonstrating more concerning pathology. Early treatment patients were more likely to arrive by ambulance, had more acute onset of symptoms, higher blood pressure and heart rates, more often received a new diagnosis of HF, and had a higher NYHA functional class with more pronounced physical signs
- Furthermore, prescription of a loop diuretic or aldosterone blocker were more prevalent in the non-early group
- Early treatment and lower in-hospital mortality was associated only on univariate analysis. However, in multivariate analysis, there was no interaction between the early treatment group, the AHF HF score, and in-hospital mortality
- Finally, D2F may be associated with institutional quality as opposed to actual prognosis, although this study accounts for it in models
- Only one third of the study population received the intervention
Other Issues
Framingham Criteria for AHF (2 major OR 1 major plus 2 minor)
| MAJOR | MINOR |
| Acute pulmonary edema | Ankle edema |
| Cardiomegaly | Dyspnea on exertion |
| Hepatojugular Reflux | Hepatomegaly |
| Neck vein distention | Nocturnal cough |
| Paroxysmal Nocturnal Dyspnea | Pleural effusion |
| Pulmonary rales | Tachycardia > 120 |
| Third heart sound (S3 gallop) | |
| Weight loss > 4.5 kg in 5 days in response to treatment |
McKee PA et al. The Natural History of Congestive Heart Failure: The Framingham Study, NEJM 1971; 285: 1441-1446. PMID: 5122894
Author's Conclusions
“In this prospective multicenter, observational cohort study of patients presenting at the ED for AHF, early treatment with intravenous loop diuretics was associated with lower in-hospital mortality.”
Our Conclusions
The authors structured a rigorous prospective observational study evaluating optimal treatment timing for a prevalent condition. However, as the authors acknowledge, these results are at best associations and not causative and so can be used to generate hypotheses going forward in the literature.
While rigorous, the study was limited by the ethical boundaries of delaying treatment. As such, the study fails to convincingly demonstrate a causative relationship because significant differences in the cohorts could also drive the D2F time. Because of the substantial differences in the background of the cohorts, there is a high concern for confounding by indication.
Finally, as the authors acknowledge, the intervention group was one third of the population studied. Given the small sample size, there is a large possibility for Type I error.
Potential Impact To Current Practice
The study design did not capture the complexity of acute heart failure diagnosis and management in the ED. Based on this observational data with unequal baseline characteristics, no change in management is recommended at this time.
Bottom Line
This study demonstrates the intuitive: patients with a clear diagnosis of AHF on arrival to the ED will receive appropriate treatment sooner and do better in the hospital. When the diagnosis is more subtle, delays will occur. The standard care still stands: patients should receive IV furosemide as soon as the diagnosis of AHF with volume overload is made. It is critical to note that not all patients with AHF will require furosemide as many (~ 50%) are not volume overloaded.
Read More
EM Lit of Note: The Door-to-Lasix Quality Measure
EMS MED: When It’s More Complicated Than A Tweet: Door-To-Furosemide And EMS
REBEL EM: Door to Furosemide (D2F) in Acute CHF . . . Really?
emDocs.net: Furosemide in the Treatment of Acute Pulmonary Edema
Fonarow GC, The Acute Decompensated Heart Failure National Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure, Rev Cardiovasc Med 2003; 4 Suppl 7:S21-30. PMID: 14668697
McKee PA et al. The Natural History of Congestive Heart Failure: The Framingham Study, NEJM 1971; 285: 1441-1446. PMID: 5122894