Background
The advent of percutaneous coronary intervention (PCI) led to a decrease in morbidity and in-hospital mortality for patients presenting with ST-elevation myocardial infarctions (STEMI). In 1999 the American College of Cardiology and American Heart Association updated their guidelines with the benchmark door-to-balloon time (DTB) to be less than 90 minutes. It has since been adopted as a measure of quality with many hospitals attempting to achieve faster times with the thought that shorter times will improve clinical outcomes.
However, the process of achieving faster DTB times can come with an increase in activations for false-positive STEMI (FP-STEMI) diagnoses, leading to patients being triaged inappropriately to catheterization labs. Any time spent in less ideal settings with patients receiving inappropriate procedures, can be detrimental for these critical patients.
Clinical Question
During the initiation of an aggressive campaign to reduce DTB times what was the incidence and in-hospital mortality rate of FP-STEMI patients?
Population
Patients who presented to the hospital with a presumed STEMI and confirmed ST elevations on EKG who underwent emergent cardiac catheterization
Intervention
“Aggressive Protocol”
– Immediate contact with interventionalist via cell phone upon activation of STEMI by the Emergency physician (<5 minutes)
- Electrocardiography within 5 minutes of arrival
- During “after-hours”, staff were expected to arrive to the catheterization laboratory within 30 minutes
Quality Improvement(QI)Initiative
– Emphasis on the profile of patients most likely to have a FP-STEMI
– Teaching intervention for caregivers involved in the activation for a FP-STEMI
– Monthly QI meetings to review FP-STEMI cases
– Reviewing diagnostic algorithms for pulmonary embolism and catastrophic intracerebral events
Outcomes
DTB time, incidence of FP-STEMI, incidence of in-hospital mortality in patients with TP-STEMI and FP-STEMI within 12 months before and 12 months after the initiation of the “aggressive protocol”.
Design
Retrospective, single center trial
Excluded
Patients who did not meet the ECG criteria for ST-segment elevation
Primary Results
Critical Findings
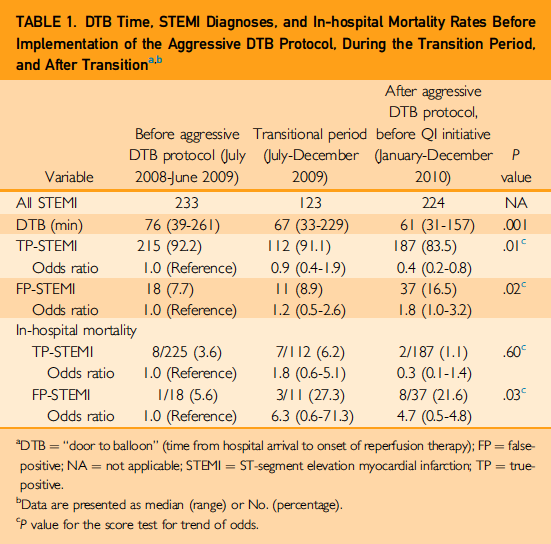
After initiation of Aggressive Protocol
- Median DTB time 76 minutes vs. 61 minutes (absolute change 15 minutes, p < .001)
- In-hospital mortality for TP-STEMI 3.6% vs. 1.1% (absolute change 2.5% p 0.60)
- In-hospital mortality for FP-STEMI 5.6% vs. 21.6% (absolute change 16% p < .03)
After initiation of QI Initiative
- Median DTB time 61 minutes vs. 59 minutes (absolute change 2 minutes, p < .03)
- In-hospital mortality for TP-STEMI 1.1% vs. 1.2% (absolute change 0.1% p 0.90)
- In-hospital mortality for FP-STEMI 21.6% vs. 4.5% (absolute change 17.1% p < .03)
Strengths
- Development of QI initiative
- Follow up was complete and appropriately long
Limitations
- Single center, retrospective study
- Small sample size
- Non-standardized QI initiative making it more difficult to reproduce
Other Issues
- These results do not include 12 month transition periods between the initiation of the “Aggressive Protocol” or the “QI initiative”
Author's Conclusions
“Aggressive measures to reduce an already acceptable DTB time can increase the incidence of FP-STEMI. Efforts to reduce DTB time should be monitored systematically to avoid unnecessary procedures and the associated delay in appropriate care for life-threatening noncardiac conditions because FP-STEMI may be associated with poor outcome. Achieving some balance by addressing both FP-STEMI and DTB times may be optimal.”
Our Conclusions
The implementation of more aggressive protocols to achieve faster DTB times will undoubtedly increase the number of FP-STEMI patients. Though the rates of in-hospital mortality secondary to increased FP-STEMI’s may be tempered by QI initiatives, it may be unnecessary to achieve faster times if they don’t show a mortality benefit.
Potential Impact To Current Practice
As Emergency Medicine providers, we are often encouraged to have a low threshold for activating STEMI’s early in order to achieve appropriate DTB times. However, it is prudent to realize that there are risks of sending patients with FP-STEMIs to the catheterization laboratory. Often spending more time taking an efficient history may help us to better distinguish between a TP-STEMI and a FP-STEMI. Identification of STEMI mimics (i.e. sepsis, aortic dissection, pulmonary embolism, intracranial hemorrhage) is likely to improve patient outcomes.
Bottom Line
Protocols to achieve DTB times less than already acceptable times can be detrimental to patients.
Read More
REBEL Cast: December 2015 All Cardiology REBEL Cast