Background
Acute Aortic Dissection (AD) is an uncommon, but potentially fatal cardiovascular disorder with a mortality of 1-2% per hour. This requires rapid identification and diagnosis, however, there are a limited number of screening tools available. Currently three diagnostic studies are employed: CT, MRI and TEE. Unfortunately, these modalities are time consuming, carry the risk of radiation and contrast reactions (in the case of CT) and are not always accessible (i.e. MRI and TEE). This introduces the need for a quick, inexpensive and safe alternative screening tool that could exclude the diagnosis of AD.
The D-dimer, a product of fibrinolytic degradation, is a well-studied AD as well. Over the past decade, many studies have been published evaluating the use of D-dimer assays to rule out AD. These studies have been limited in their ability to draw accurate conclusions due to poor study design, small sample sizes, and variations in D-dimer cut-off levels.
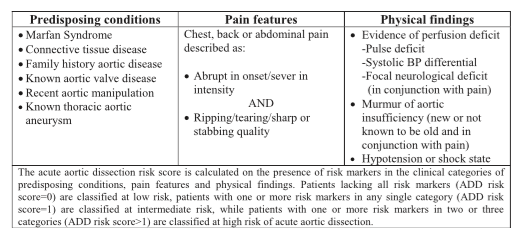
In 2010, the American Heart Association released the Aortic Dissection Risk Score to risk stratify patients based on predisposing conditions, pain features and examination findings. Patients were stratified into low (score = 0), intermediate (score = 1) and high (score >1). Further studies have supported the use of this score to identify low-risk populations. However, no study has effectively proven the use of a diagnostic strategy to rule-out Aortic Dissection in this low risk population.
Clinical Question
In patients presenting to the hospital with suspected acute AD, can a negative D-dimer result rule out this diagnosis?
Design
Systematic Review and Meta-analysis of cross sectional studies.
Literature Search
Computer search of MEDLINE, EMBASE, Medion database and Google Scholar. Authors then conducted a hand search of reference lists of all articles, systematic reviews and meta-analysis identified. Two reviewers independently screened the titles and abstracts, resolving any disagreements by consensus.
Outcomes
Negative D-dimer (<0.50 μg/mL) in patients without AD.
Inclusion
Original research that addressed the use of D-dimer as a diagnostic test for acute AD, cross- sectional study design, prospective enrollment of participants before confirmation of the diagnosis, D-dimer was measured, diagnosis confirmed or refuted with an acceptable reference standard, absolute markers of true positive, true negative, false positive and false negative were reported or could be derived
Excluded
Retrospective enrollment, case control or case series, nonhuman studies, research only in the form of a conference abstract (no peer review process)
Primary Results
Primary Results
- 4 studies with 1,557 patients included
- Sensitivity: 98.0% (95% CI = 96.3% to 99.1%)
- Specificity: 41.9% (95% CI = 39.0 to 44.9%)
- Negative Likelihood Ratio: 0.05 (95% CI 0.03 to 0.09)
- Positive Likelihood Ratio: 2.11 (95% CI = 1.46 to 3.05)
Critical Findings
- Using a D-dimer cut-off of 0.50 mg/mL applied to the AHA defined low risk population, the post-test probability is 0.3%.
- 1 missed case for every 333 low risk patients evaluated.
Strengths
- High quality studies included with methodological quality assessed by authors
- Low heterogeneity between studies
- High inter-rater reliability
Limitations
- Small number of studies included (n=4)
- Given the high disease prevalence (29%), results may be weighted towards patients with classic symptoms and may not be generalizable to populations where the prevalence is lower.
- Did not address publication bias or use a funnel plot due to limited number of studies.
- Possible selection bias given the exclusion of patients without D-dimer measurements
Author's Conclusions
“This meta-analysis suggests that a negative D-dimer result may be useful to help rule out acute aortic dissection in low-risk patients.”
Our Conclusions
This high quality, well-organized study used the best literature available to date, however still lacks the appropriate clinical context in which to apply these results. Prospective observational or randomized trials comparing outcomes of the two diagnostic strategies (D-dimer vs diagnostic imaging) is needed for external validation. Furthermore, the use of the Aortic Dissection Risk score limits the number of patients applicable for this diagnostic scheme. Based on the scoring principles, patients must lack most of the clinical characteristics that raise the suspicion for Aortic Dissection. Clinicians must be careful when applying this to patients with nonspecific symptoms, in there is no suspicion for AD as this could increase the use of diagnostic studies. The use of a D-dimer cut-off of 0.50 μg/mL, although cited often in the literature, has not been proven to be the best cut off level for the detection of AD. A study comparing the sensitivity and specificity of various D-dimer levels is also needed to establish a standard cut-off for further studies. Finally, different D-dimer assays are used across a variety of hospitals, thus the results of this study may not be applicable to clinical settings employing different D-dimer assays.
Potential Impact To Current Practice
As the results still require further validation, this should not change current clinical practice, but may be something to consider in the future.
Bottom Line
A negative D-dimer (< 0.50 μg/mL) in a low risk patient may be helpful in ruling out AD. The number of patients identified as low risk is limited. Further studies are required to validate the use of D-dimer in AD evaluation.
Read More
- Boring EM: Could My Patient Have an Aortic Dissection
- emDocs.net: D-Dimer in Aortic Dissection Workup
- LITFL: EBM Aortic Dissection
- EM: RAP: Paper Chase 2 – D-dimer and Aortic Dissection
Great study but I think the conclusion is better stated as: ddimer is useful to rule out aortic dissection in people so low risk they should not be tested for aortic dissection.
…which is essentially never. The scenario I find it useful: patient being admitted for chest pain without any concerning features for dissection, has a negative ddimer from a PE workup, and the team asks about whether dissection is a consideration.
Initially, upon seeing this study I too felt that the number of patients this low risk score would apply to where there was real concern for AD was negligible, however, in a prospective validation of the Acute Aortic Dissection Risk Score (Diagnostic performance of the aortic dissection detection risk score in patients with suspected acute aortic dissection.) 33.1% of patients were classified in the low-risk group. Patients were included in the study if they demonstrated symptoms concerning for aortic dissection and if the physician was sufficiently concerned to order a definitive imaging study specifically to rule in or rule out aortic dissection. My understanding is that this study would suggest that were d-dimer to be validated as a means for ruling out AD, a significant number of patients might benefit from reduced imaging.
If it’s validated, sure. But until validation (and maybe an update to the ACEP clinical policy)…
DD may be normal in Penetrating ulcer and intramural heamatoma (5 and 15% of total acute aortic syndromes, respectively)