The Case
An elderly male with a past medical history of hypertension and diabetes presents to the emergency department with a chief complaint of diarrhea and shortness of breath. His vital signs are: HR 60, BP 105/65, RR 30, O2 100% on room air, oral T 98.6 F, and FSG 120.
Show Details
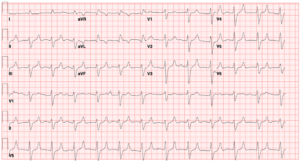
EKG Characteristics
-
Rate
60 BPM
-
Rhythm
Regular, no discernible P-waves
-
Intervals
PR na; QRS complex > 160 ms; QT Prolonged
-
Axis
LAD
-
ST Segments
Wide QRS complexes slurring into very large pointed T waves
Diagnosis
Diagnosis:
Junctional Wide-Complex Bradycardia secondary to Hyperkalemia
Consider a secondary etiology of intraventricular conduction delay (prolonged QRS) in patients who demonstrate:
- Significant QRS widening
- RBBB morphology with QRS > 140
- LBBB morphology with QRS > 160
- Lack of pacemaker spikes
- Lack of hypothermia
- V1 and V6 QRS complex morphology not consistent with a bundle branch block.
Questions
-
What is your differential for a non-tachycardic wide-complex rhythm?
Hyperkalemia, Sodium-channel blockade (ex: tricyclic acid overdose), Pre-excitation syndromes (ex: Wolff-- Parkinson-White syndrome), Aberrant conduction (ex: bundle branch blocks), Ventricular-Paced beats, Hypothermia, Ventricular ectopy
-
What immediate interventions should be considered based off of this initial ECG?
IV Calcium, Sodium Bicarbonate
Discussion
Case Discussion
On exam, the patient was ill-appearing. He had a regular heart rate with no murmur, rapid and deep breathing with clear lungs, a non-distended, non-tender abdomen, and warm and well-perfused extremities. He was alert but groaning and unable to answer questions. His family provided further history, explaining that he had had diarrhea for several days and today was noted to be more lethargic and breathing quickly, which prompted their emergency department visit. His only medications were lisinopril and metformin. He had no history of kidney disease.
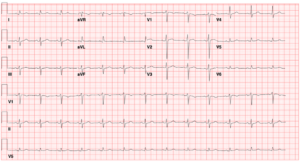
The patient was immediately placed on a cardiac monitor, and an IV was placed. Labs were drawn, and one ampule of sodium bicarbonate and one gram of calcium gluconate were given. The QRS complex on the cardiac monitor was noted to narrow, and the following EKG was obtained.
Note the narrowing of the QRS complex and ST segment. You can now clearly observe “peaked” T-waves. Also, note that P-waves are still not discernible.
The patient’s labs returned and were notable for a pH of 7.0, a lactate of 8, a potassium of 7.5, and a creatinine of 13. Acute Kidney Injury was likely secondary to insensible losses and poor oral intake combined with the use of an ACE inhibitor. The patient was admitted to the medical intensive care unit and emergent underwent dialysis. His EKG on discharge is shown below.
Hyperkalemia
Cardiac conduction partially depends on a gradient of lower extracellular (plasma) potassium levels and higher intracellular potassium levels. A change in this gradient as a result of higher extracellular potassium levels leads to abnormal repolarization (resulting in peaked T waves), abnormal excitability at the sinoatrial node (resulting in a slower heart rate), and abnormal conduction through the AV node and His-Purkinje system (resulting in PR and QRS prolongation). The final result is often called a “sine wave,” which can progress to asystole. Note that ECG changes in the setting of hyperkalemia may not occur linearly or have a direct association with potassium levels.
Initial management of hyperkalemia is with calcium, which stabilizes the cardiac membrane for up to 60 minutes. Calcium gluconate, 1000 mg (10 mL of a 10 percent solution) infused over two to three minute, is often first-line because it can be safely administered with peripheral IV access. Calcium chloride provides 3x the calcium calcium compared to calcium gluconate and is often reserved for patients in extremis, including persistent arrhythmia or cardiac arrest.
Sodium bicarbonate is an acute treatment option that raises the serum pH, resulting in hydrogen ion release from cells and potassium influx into cells. Sodium bicarbonate has several drawbacks, such as often being in a hypertonic solution (which is the case with sodium bicarbonate ampules found in most code carts) and not being compatible with calcium chloride (using both of these can precipitate calcium carbonate). It may be reasonable to trial Sodium Bicarbonate in patients with an acute prolongation of QRS in whom a secondary etiology of intraventricular conduction delay is considered (hyperkalemia or sodium channel blocker toxicity).
Potassium can be shifted from the plasma into cells with insulin and beta-agonists, which lower serum potassium by enhancing the activity of the Na-K-ATPase pump in skeletal muscle, resulting in the influx of potassium into cells. Regular insulin can be given as 5-10 units, followed immediately by 50 mL of 50 percent dextrose (25g of glucose). Caution should be given as insulin is renally cleared, and patients with acute kidney injury have an increased risk of hypoglycemic episodes. Nebulized albuterol can be given as 10mg in 4 mL of saline over 10 minutes (about four times the dose used for bronchodilation).
For further discussion on Hyperkalemia and the Hyperkalemic ECG, see Core EM Podcast Episode 189:
Pearls
- Consider a secondary etiology of intraventricular conduction delay (prolonged QRS) in patients who demonstrate significant QRS widening, including a RBBB morphology with QRS > 140 or LBBB morphology with QRS > 160
- Consider a large differential for a slow, wide-complex rhythm including hyperkalemia, sodium-channel blockade, WPW syndrome, bundle branch blocks, hypothermia, ventricular ectopy or ventricular arrhythmia, ventricular pased rhythms
- Stabilize undifferentiated sick patients with slow, wide-complex rhythms with 1000 mg calcium gluconate and sodium bicarbonate ampules. Acutely shift potassium into cells with 10u insulin with 25 g glucose and 10 mg nebulized albuterol. Assess for appropriate measures to remove potassium from the body (kaliuresis, fluid resuscitation, GI resin, dialysis).



Wonderful rewiew. Thank you