The Case
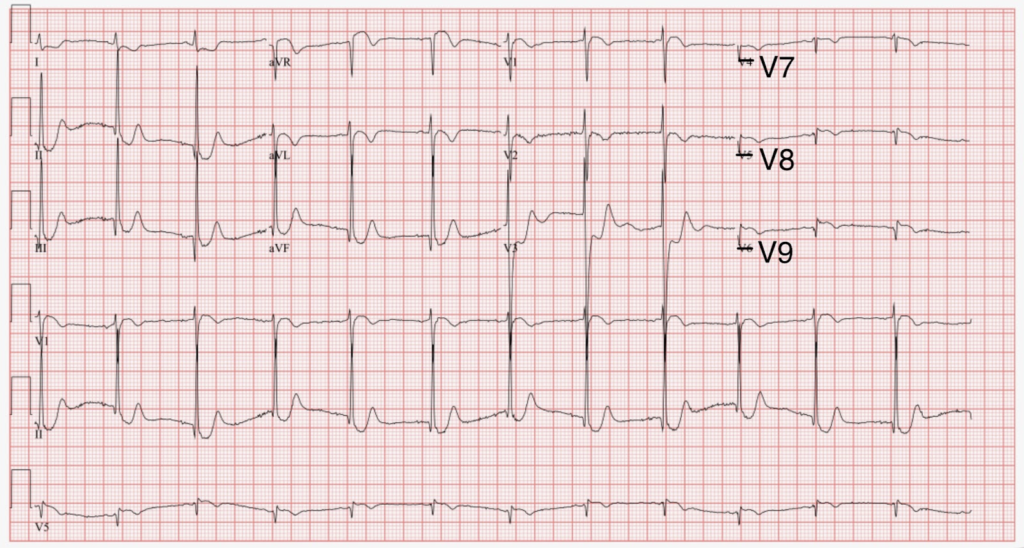
A 71-year-old male with a history of chronic obstructive pulmonary disease, hyperlipidemia, and peptic ulcer disease presents to the emergency department with substernal chest pain radiating down the right arm and dyspnea that began acutely while “running” up the stairs from the subway. The following ECG is obtained upon arrival to the emergency department.
Show Details
EKG Characteristics
-
Rate
54
-
Rhythm
Sinus Bradycardia
-
Intervals
Normal PR, QRS, QT Intervals
-
Axis
Normal
-
ST Segments
ST Depression in Leads V2-V6
Diagnosis
Diagnosis: Posterior STEMI
Questions
-
What is the next test that should be obtained in the management of this patient?
Posterior ECG
-
What is the differential diagnosis of the acute ECG changes in the context of the patient’s presenting symptoms?
Posterior STEMI, Reciprocal changes of inferior or lateral STEMI, NSTEMI (subendocardial infarction)
Discussion
Posterior Myocardial Infarction (PMI) represents 15-21% of occlusive myocardial infarction (OMI) and is often accompanied by inferior or lateral MI. Isolated posterior MI is less common (3-8% of OMI) and presents with isolated ST-depressions in the anterior precordial leads (V1-V4), representing reciprocal changes to posterior left ventricular wall myocardial infarction as a result of distal occlusion of either the left circumflex or right coronary artery. ECG features suggestive of Posterior MI include:
- Horizontal or downsloping ST-depression in precordial leads
- Tall R waves in precordial leads
- Upright T-waves in precordial leads
Lack of ST-elevation on initial standard ECG may lead to providers to miss this etiology of STEMI, resulting in a delay to reperfusion therapy. A posterior ECG should be obtained and emergent cath lab activation should be pursued with evidence of STEMI on posterior ECG.
Posterior ECG can be obtained with the following lead placement:
- V7 – Left posterior axillary line, in line with the inferior angle of the left scapula, at the same level as V6
- V8 – Tip of the left scapula, at the same level as V6
- V9 – Left paraspinal region, at the same level as V6

Hospital Course:
The patient’s symptoms and acute ST-depressions on initial ECG were concerning for an acute coronary syndrome. A 12-lead Posterior ECG revealed 1-2 mm ST elevation in leads V7-V9, meeting the criteria for a STEMI.
The cath lab was activated and the patient was emergently taken for left heart catheterization. He was found to have severe multi-vessel coronary artery disease involving a 95% occlusion in the distal left main to proximal LAD, 80% occlusion in the ostial RCA, and 100% occlusion in the mid-RCA. Initial high-sensitivity troponin came back at 1,495 ng/L. The patient underwent balloon angioplasty to the ostial-mid RCA, right femoral intra-aortic balloon pump (IABP), and complex PCI with placement of 5 drug-eluting stents (DES). The patient did well during his hospital stay and was subsequently discharged home in good condition on hospital day 7 on aspirin, ticagrelor, and atorvastatin.
Pearls
- Consider Posterior STEMI as an etiology of acute ST-depressions in the anterior precordial leads (V1-V4). Posterior ECG should be performed to rule in the diagnosis of Posterior STEMI.
- Acute anterior ST depressions in the precordial leads with evidence of inferior or lateral wall OMI is representative of posterior ventricular wall involvement and is associated with increased size of infarction with increased risk of dysrhythmia, left ventricular dysfunction and death.
- Posterior STEMI should undergo emergent catheterization for identification of OMI and subsequent reperfusion therapy.
Sources
Burns, E., Cadogan, M., & Cadogan, E. B. and M. (2023, June 8). Posterior myocardial infarction. Life in the Fast Lane • LITFL. https://litfl.com/posterior-myocardial-infarction-ecg-library/


