Written by: Sadakat Chowdhury MD
Edited by: Mak Sarich MD, Jay Lin MD, Jonathan Kobles MD
Background:
Ultrasound (US) guided nerve blocks offer an applicable option for achieving analgesia in the emergency department. As an alternative to parenteral or oral analgesia, nerve blocks have the potential for improved pain control, decreased risk of harm (hypoventilation, compromised airway or perfusion, potential for addiction), and decreased length of hospital stay.1 2 3 4 This article will focus on three lower extremity (LE) nerve blocks commonly used for acute lower extremity pain in the ED.
Anatomy:
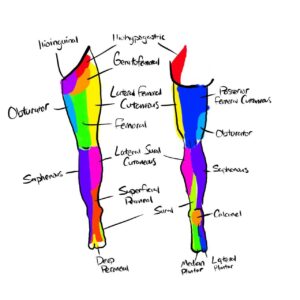
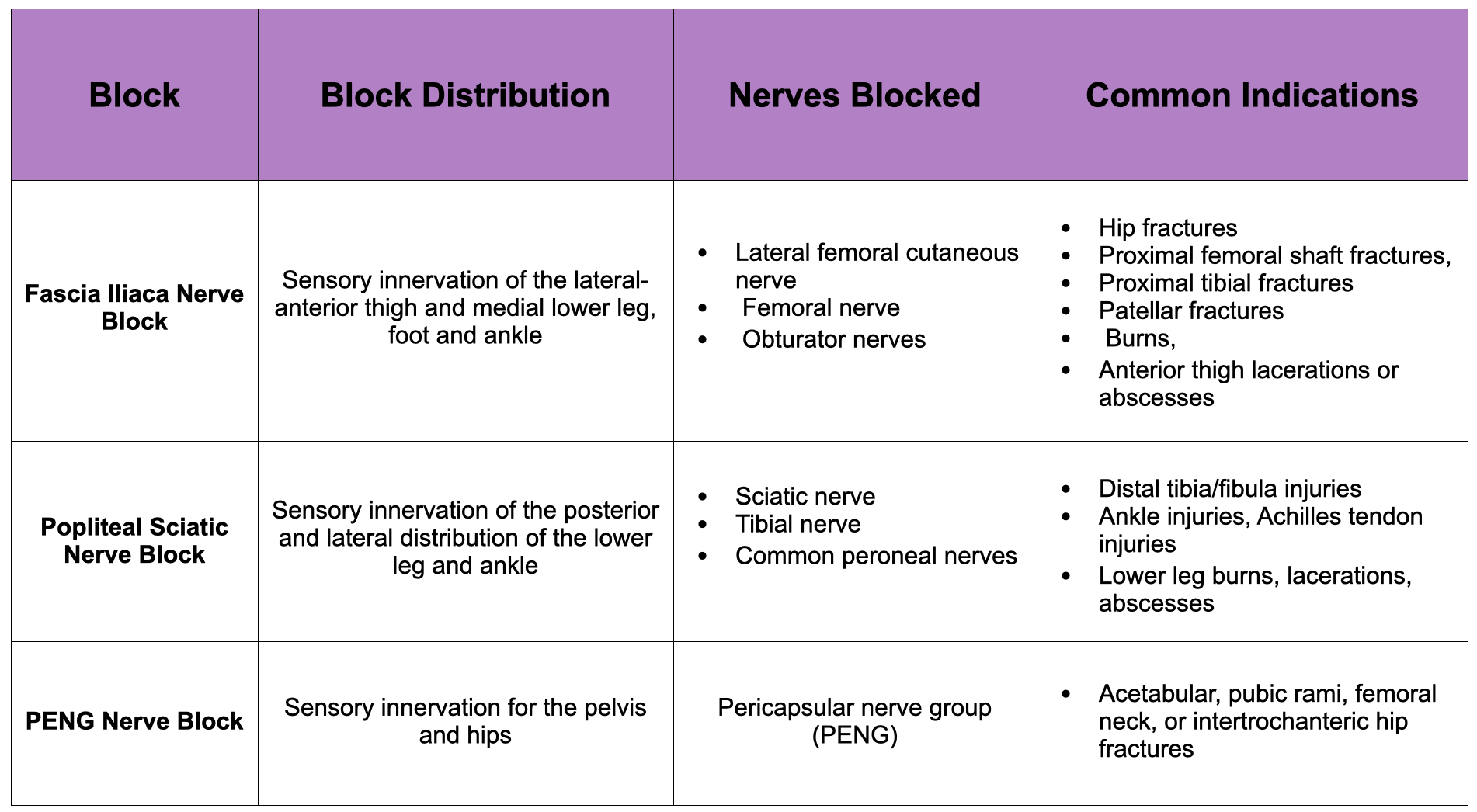
- The lumbar plexus (T12-L4) breaks off into the femoral, lateral femoral cutaneous, obturator, genitofemoral, ilioinguinal, and iliohypogastric nerves which are the main sources of sensory and motor innervation in the anterior LE.
- The femoral nerve branches into its terminal sensory portion, the saphenous nerve.
- The sciatic nerve (L4-S3) courses posteriorly along the thigh and divides into the tibial (which subdivides into the sural nerve) and common peroneal (which subdivides into the superficial and deep peroneal) nerves. These nerves serve most of the sensory and motor innervation for the posterior LE. The sensory distributions of each nerve are depicted in the figure below.
Preparation:
Probe Selection: The linear transducer is ideal for most patients; the curvilinear transducer can be used for patients with larger body habitus where greater depth is needed to visualize the anatomy.
Materials Needed:
- 10 cc sterile saline
- IV tubing
- US-guided nerve block needle or 18-22 gauge Quincke spinal needle
- 60 mL syringe
- US probe cover
- Antiseptic wipes
- Local anesthetic (LA) of choice
- Ensure that your ED has easily assessable intralipid in the case of systemic toxicity
Procedures should be carried out by two operators:
- Primary operator utilizing sterile technique to operate ultrasound and needle-guidance to nerve
- Second operator to flush and aspirate syringe
Commonly Used Local Anesthesia:
| Local Anesthesia | Maximum Dose (mg/kg) with and without Epinephrine | Onset (min) | Duration of analgesia (hours) |
| Lidocaine 1% | 4/7 | 10-20 | 3-8 |
| Bupivacaine 0.5% | 2/3 | 15-20 | 6-30 |
| Ropivacaine 0.5% | 3/3.5 | 15-30 | 5-24 |
Adverse effects:
- Infection
- Vascular injury including hematoma or pseudoaneurysm formation
- Nerve damage
- Local anesthesia systemic toxicity (LAST) – confusion, anxiety, headache, drowsiness, hypotension, arrhythmias including ventricular tachycardia or fibrillation.
-
-
- Blocks with larger volumes of anesthetic carry higher risk of LAST.
- Treatment of LAST is supportive care and administration of intralipid
-
- Intralipid 20% 1.5 mL/kg over 1 min, then 0.25 mL/kg/min for 20 mins is suggested is case of LAST
-
-
- Bupivacaine carries a higher risk of cardiotoxicity.
Contraindications:
- Inability to safely cooperate with procedure
- Allergy to local anesthetic
- Overlying infection
- Anticoagulation and coagulopathies are relative contraindications
General Setup and Technique:
- Obtain appropriate consent from the patient.
- Perform a neurovascular assessment of the patient before and after the procedure.
- Ensure all your supplies are at the bedside with your IV tubing connected to the nerve block needle.
Fascia Iliaca Nerve Block:
- Blocks the lateral femoral cutaneous nerve, femoral nerve, and obturator nerve by spreading anesthetic across a fascial plane. This will affect sensory innervation to most of the anterior thigh and medial lower leg.
- Indications include hip fracture, proximal femoral shaft fractures, proximal tibial fractures, patellar fractures, burns, anterior thigh lacerations, or abscesses.
Set up:
- Have the patient on monitors and in a supine position.
- Prepare a 60 cc syringe filled with 15-20 mL of LA mixed with 15 mL of sterile saline. Calculate the maximum safe local anesthetic dosage for the patient.
- Don a set of sterile gloves, and using sterile technique, drape and prep the patient’s infra-inguinal area with antiseptic wipes. Use an assistant to apply a sterile probe cover over the US transducer.
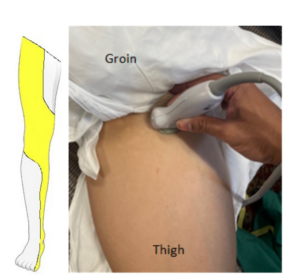
Identification of landmarks:
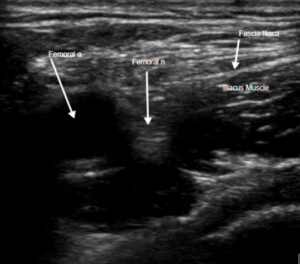
Identify the femoral vein and artery in a transverse orientation. The femoral nerve should be a hyperechoic triangle-shaped structure coursing laterally and housed under the fascia iliaca,the fascial plane above the iliacus muscle.
- Using the in-plane technique, identify the location where you will insert your needle lateral to the femoral nerve and coursing towards the fascia iliaca. Insert the needle through the skin with visualization of the needle tip at all times.
- Advance the needle until entering the fascia iliaca space. You should feel two distinct popping sensations, one when breaking the fascia lata and another when breaking the fascia iliaca.
- Have your assistant aspirate, and then hydrodissect the fascial place with sterile saline. After confirming appropriate location in the fascia iliaca, have your assistant inject your preparation of LA and sterile saline in 5 mL aliquots with gentle aspiration between injections. You should visualize the femoral nerve being pushed medially and an anechoic spread of the fascia iliaca.
- Repeat a neurovascular assessment of the patient after the procedure.
Popliteal Sciatic Nerve Block:
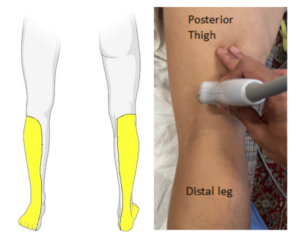
- Blocks the sciatic nerve, tibial nerve, and common peroneal nerve. This will affect sensory innervation to the posterior and lateral distribution of lower leg and ankle.
- Indications include: Distal tibia/fibula injuries, ankle injuries, achilles tendon injuries, lower leg burns, lacerations, abscesses.
Set up:
- Place the patient in a prone position. If the patient cannot lie prone, you may elevate their ankle using sheets while they lie supine.
- Prepare a 60cc syringe with 10-15m LA and 10 mL sterile saline. Calculate the maximum safe local anesthetic dosage before performing this procedure.
- Don a set of sterile gloves, and using sterile technique, drape and prep the patient’s popliteal area with antiseptic wipes. Use an assistant to apply a sterile probe cover over the US transducer.
Identification of landmarks:
Identify the popliteal vein and artery in the popliteal fossa using a transverse orientation. The sciatic nerve will be a hyperechoic structure coursing superficially and medially. The sciatic nerve splits into the tibial and common peroneal nerve as you move the transducer distally. The target will be the perineurium between the tibial and common peroneal nerve.
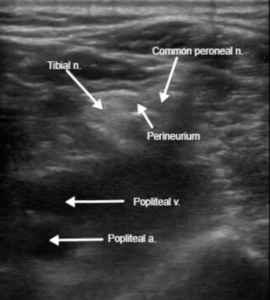

- Using the in-plane technique, identify where you will insert your needle lateral to the nerve bundle. Insert the needle through the skin. Maintain visualization of needle tip through the entirety of the procedure.
- Once you have entered the perineurium, have your assistant aspirate, and then hydrodissect with sterile saline. After confirming that the tibial and common peroneal nerves are moving peripherally, have your assistant inject your local anesthetics and sterile saline preparations in 5 mL aliquots with gentle aspiration between injections.
- Repeat a neurovascular assessment of the patient after the procedure.
PENG Nerve Block:
- This block will target the pericapsular nerve group (PENG), which innervates the pelvis. These are branches of the femoral and obturator nerve. This is a motor sparing block – so it will allow your patients to ambulate.8
- This nerve block is typically performed with a curvilinear probe, though a linear probe can be used for patients with a smaller body habitus.
- Indications includeacetabular, pubic rami, femoral neck, and intertrochanteric hip fractures.
Set up:
- Place the patient in a supine position.
- Prepare a 60cc syringe with 10mL LA and 10 mL sterile saline. Calculate the maximum safe local anesthetic dosage before performing this procedure.
- Don a set of sterile gloves, and using sterile technique, drape and prep the patient’s inguinal area with antiseptic wipes. Use an assistant to apply a sterile probe cover over the US transducer.
Identification of landmarks:
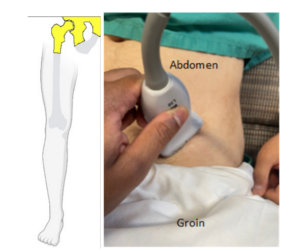
Place your transducer in a transverse orientation (rotated 45 degrees) on the proximal thigh directly adjacent to the inguinal ligament. Identify the femoral head and the femoral artery coursing superficially to it. Move the transducer superiorly and medially, and you will be able to identify the anterior inferior iliac spine (AIIS), the ilium, the ileopubic eminence (IPE), and the psoas tendon (PT).

- Using the in-plane technique, identify where you will insert your needle in a lateral to medial direction course. Insert the needle through the skin, with visualization of the needle tip at all times. Advance the needle past the AIIS and directly lateral to the bony surface of the ilium under the PT.
- Once under the PT, have your assistant aspirate and then hydrodissect with sterile saline. After confirming that the tendon is moving superficially above the ileum, have your assistant inject your preparation of LA and sterile saline in 5 mL aliquots with gentle aspiration between injections.
- Repeat a neurovascular assessment of the patient after the procedure.
References:
[1] Bhoi S, Sinha TP, Rodha M, Bhasin A, Ramchandani R, Galwankar S. Feasibility and safety of ultrasound-guided nerve block for management of limb injuries by emergency care physicians. J Emerg Trauma Shock. 2012;5(1):28-32. doi:10.4103/0974-2700.93107
[2] Nagdev A. Ultrasound-Guided Nerve Blocks. EMRA. Published June 2020. https://www.emra.org/books/pain-management/ultrasound-guided-nerve-blocks/
[3] Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58(1):76-81. doi:10.1093/gerona/58.1.m76
[4] Johnson B, Herring A, Shah S, Krosin M, Mantuani D, Nagdev A. Door-to-block time: prioritizing acute pain management for femoral fractures in the ED. Am J Emerg Med. 2014;32(7):801-803. doi:10.1016/j.ajem.2014.03.027
[5] Jeng C. Lower extremity nerve blocks: Techniques. UpToDate. Published February 4, 2022. Accessed September 29, 2022, https://www-uptodate-com/contents/lower-extremity-nerve-blocks-techniques
[6] Pepe J, Ausman C, Madhani NB. Ultrasound-guided Fascia Iliaca Compartment Block. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 31, 2021.
[7] Gulec, Nazey. Popliteal Sciatic Nerve Block. American Academy of Emergency Physicians, Published 31 Jan. 2022, Accessed September 29, 2022, https://www.acep.org/emultrasound/newsroom/january-2022/popliteal-sciatic-nerve-block/.
[8] Luftig J, Dreyfuss A, Mantuani D, Howell K, White A, Nagdev A. A new frontier in pelvic fracture pain control in the ED: Successful use of the pericapsular nerve group (PENG) block. Am J Emerg Med. 2020;38(12):2761.e5-2761.e9. doi:10.1016/j.ajem.2020.05.085