Background
- Tricyclic antidepressants (TCA) are a class of medications traditionally used to treat depression
- Currently being more widely prescribed for pain syndromes, peripheral neuropathy, migraine prophylaxis, panic and phobic disorders, and obsessive-compulsive disorder
- TCA toxicity may be fatal
- Mortality rate of ~15% (though has been lower in recent years)
- Overdoses are on the rise given expanding use of TCAs beyond depression
Pharmacokinetics
- Rapidly absorbed in the gastrointestinal tract and reach peak concentrations in the serum at 2-6 hours
- Half-lives of TCAs have a wide range depending on the mediation ingested, anywhere from 7-58 hours
- Note: Half-life does not dictate duration of toxicity. Duration of action and half-life are not the same
Pathophysiology
- TCAs act on a number of different receptors leading to toxicity
- Inhibition of the presynaptic reuptake of serotonin and norepinephrine aid in the treatment of depression
-
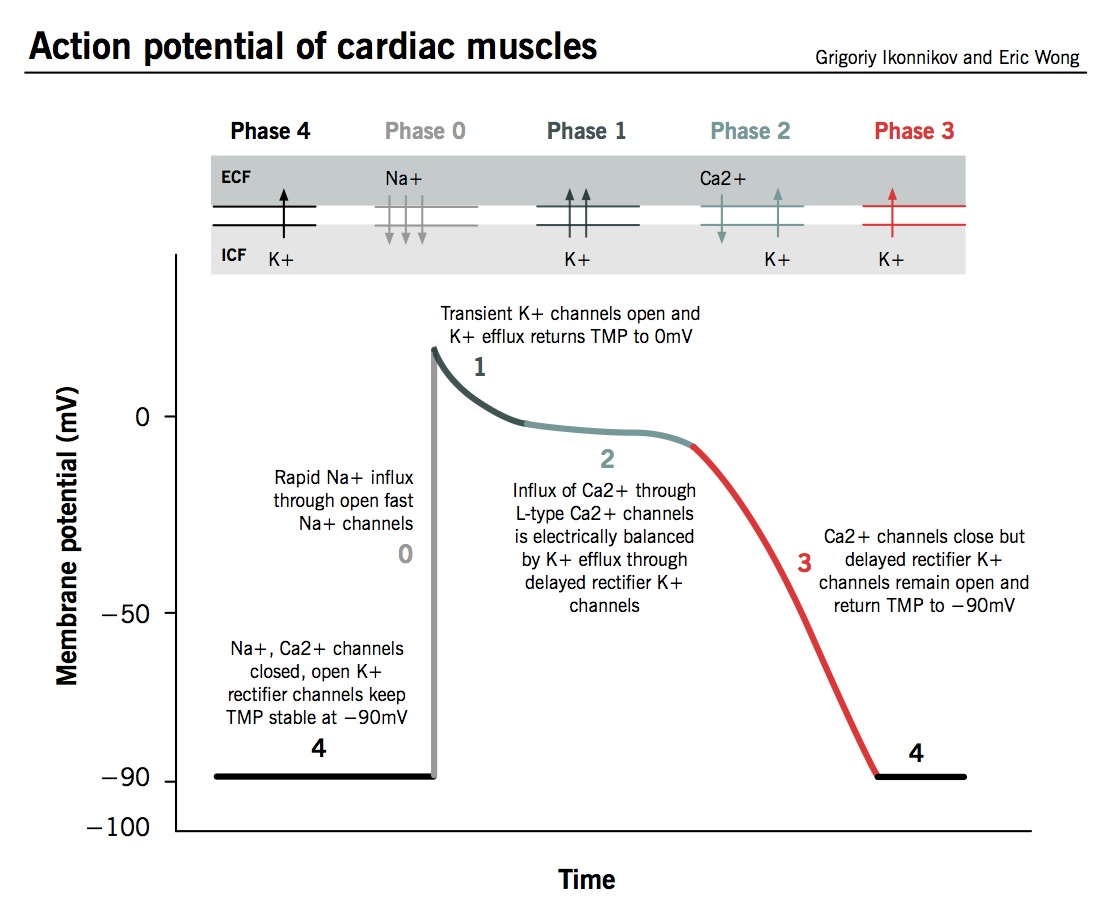
Cardiac Action Potential (www.pathophys.org)
Block cardiac fast acting sodium channels leading to cardiovascular effects
- Prevents rapid ventricular depolarization during phase 0 of the ventricular action potential (Figure 1)
- Effect on the EKG
- Prolonged Ventricular Depolarization: QRS > 100ms
- QRS > 100 msec predicts impending seizures (Boehnert 1985)
- QRS > 160 msec predicts impending ventricular dysrhythmia (Boehnert 1985)
- Rightward Deviation of the terminal 40msec QRS complex
- Deep S wave in I and aVL
- Large R wave in aVR (>3mm) with R:S ration >0.7 (Niemann 1986)
- Antagonism of muscarinic acetylcholine receptors
- Antagonism of peripheral alpha-1 adrenergic receptors
- Peripheral vasodilation
- Can cause marked hypotension
- Antagonism of H1 receptors
- Similar effects of anticholinergic activity
- Can also see delirium and confusion
- Antagonism of CNS gamma-aminobutyric acid (GABA) receptor
- Potential cause of seizure activity
Physical Exam
- Anticholinergic Toxidrome may be present
- Physical exam findings include: mydriasis, dry and hot skin, urinary and bowel retention, hyperthermia, xerostomia, tachycardia and AMS (disorientation, confusion)
- Pulmonary: Coarse breath sounds in the setting of ARDS
- Cardiovascular
- Hypotension secondary to direct myocardial depression from blockade of fast-acting sodium channels AND antagonism of peripheral alpha-1 receptors (eg vasodilation)
- Tachycardia: initially sinus tachycardia and in cases of severe overdose patients develop wide-complex tachycardia as a result of QRS prolongation and/or refractory hypotension
- Abdomen: hypoactive or absent bowel sounds, suprapubic fullness secondary to urinary retention
- Neuro: Initially altered mental status including delirium and agitation followed by lethargy and stupor, seizure activity, myoclonus, dystonia, akathisia, rigidity, myoclonus
- Skin: dry, flushed, hot skin
- Psych: hallucinations, picking at objects that are not there
Diagnostics
- EKG
- Sinus tachycardia
- Intraventricular conduction delay
- Prolonged QRS >100ms
- Rightward shift of the T40-msec QRS axis
- Wide Complex Tachycardia (non-VT)
- Note: The EKG should be reviewed in any patient with an anticholinergic toxidrome and, a QRS > 100 msec should preclude the use of physostigmine
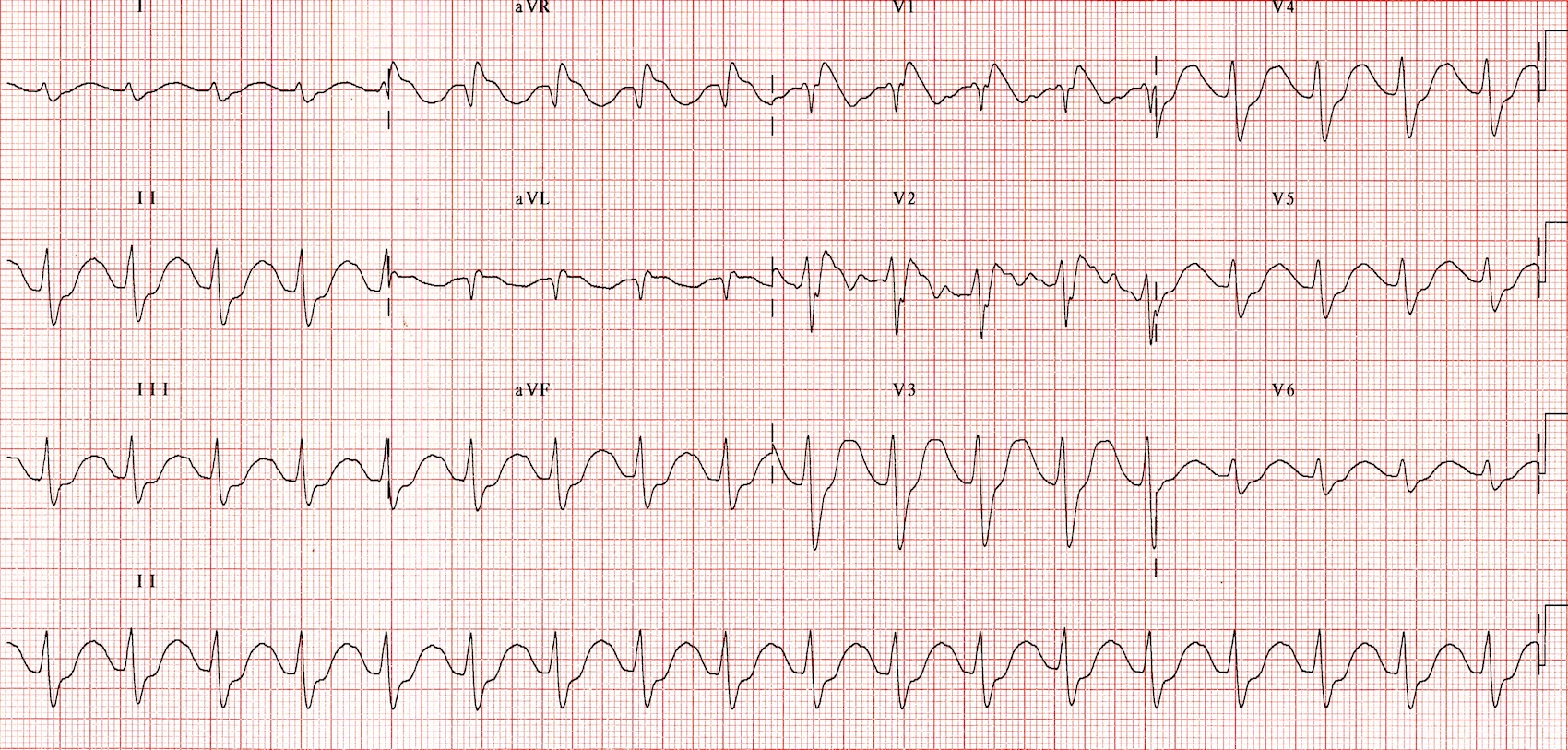
TCA Toxicity (LITFL) – Broad QRS, Sinus Tachycardia, Terminal R Wave in aVR
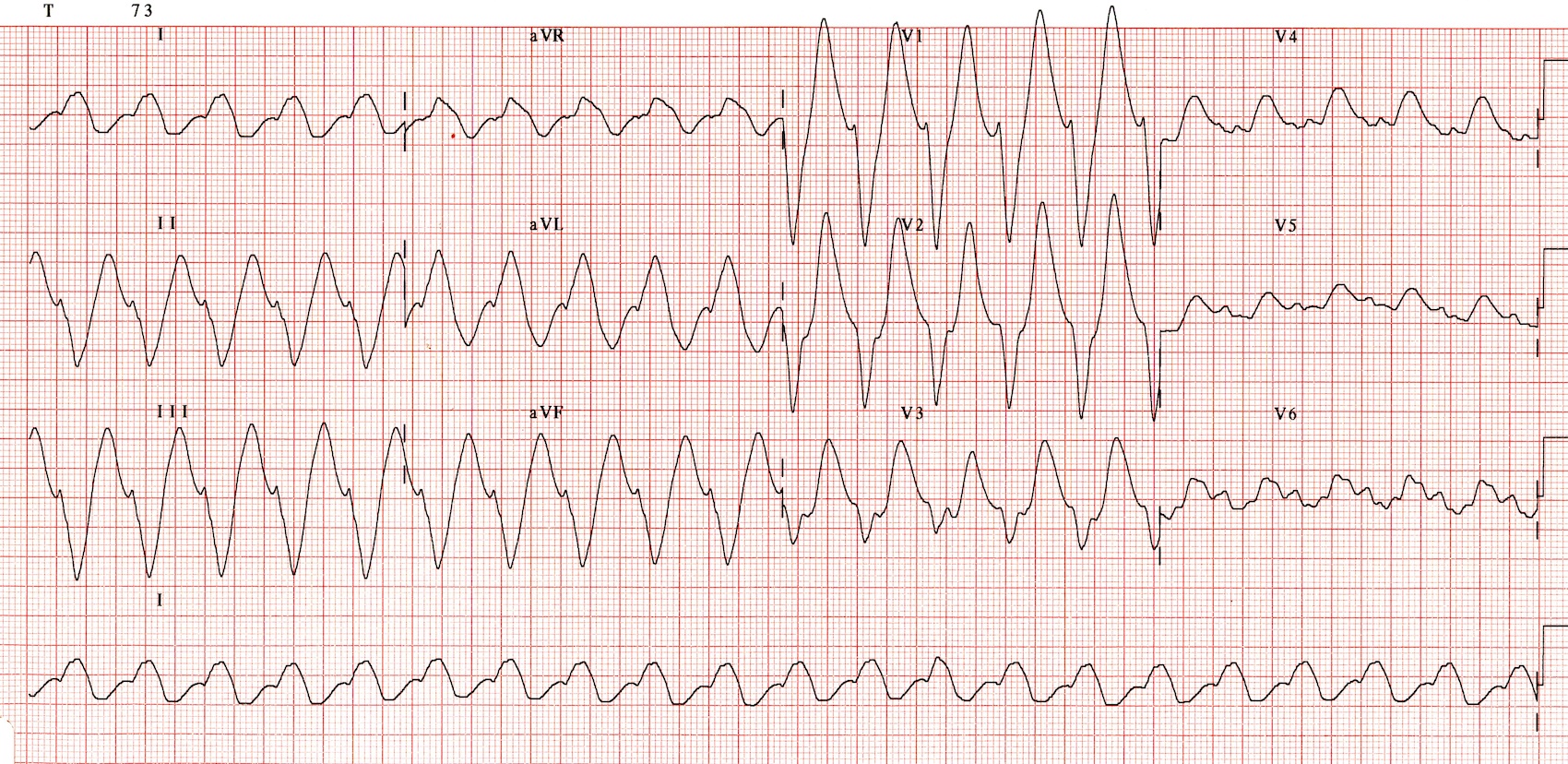
TCA Toxicity (LITFL) – Broad QRS
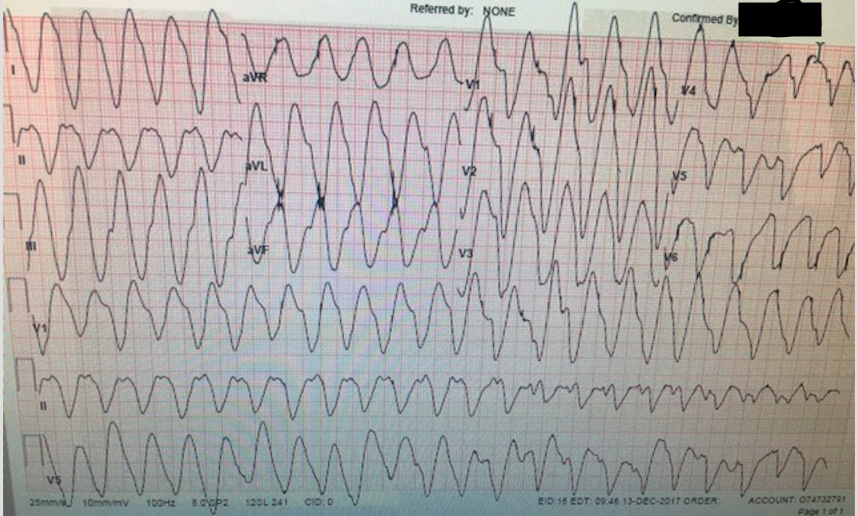
TCA Toxicity – Wide QRS/Sine Wave
- Labs
- Blood gas: pH status while giving sodium bicarbonate, lactate as a marker of hypoperfusion
- Check for concomitant ingestions: salicylate and acetaminophen levels
- Basic metabolic panel: evaluate electrolytes, renal function
- Hepatic panel: evaluate liver function
- Obtaining a TCA concentration is not necessary as they are delayed and, patients aren’t treated based on concentration but rather on effect of the drug.
ED Management
- Supportive Care
- Assess airway, breathing and circulation
- Large bore IV X 2, supplemental O2 if needed and continuous cardiac monitoring
- Intravenous crystalloid fluids
- Always consider co-ingestants
- Avoid physostigmine (Pentel 1980)
- Despite the presence of an anticholinergic toxidrome, physostigmine should not be given to these patients
- Small case series showed worse outcomes in TCA toxic patients treated with physostimine
- Contact your local poison control center for expert consultation
- Directed Management
- Sodium Bicarbonate (NaHCO3)
- Bolus 1-2mEq/kg with additional boluses every 3-5 minutes until the QRS narrows to <100ms and hypotension improves
- Aim for a pH below 7.55
- If patient is intubated, can use mechanical ventilation to control pH
- Effects of NaHCO3
- Increases the sodium gradient across the cardiac fast acting sodium channels which overwhelms blockade by the TCA allowing for return of the rapid rise of phase 0 of the ventricular action potential
- Raises serum pH which removes the TCA from the binding site on the sodium channel as the majority of drug binding to sodium channels occurs in the ionized state
- Alternative to NaHCO3 – 3% hypertonic saline
- 1 liter of 3% saline has 513 mEq of Na = 51.3 in 100mL. Equivalent sodium content as 50mL of 8.4% sodium bicarbonate (1 ampule)
- Dose: 100mL bolus of 3% hypertonic saline, repeat 100mL boluses until QRS narrows
- Gastrointestinal Decontamination
- Activated charcoal for awake and alert patients following commands
- Orogastric lavage for intubated patients
- Benefit not proven in a controlled trial
- Delayed gastric emptying from anticholinergic properties may increase benefit of lavage
- Sodium Bicarbonate (NaHCO3)
- Management of Hypotension (Niemann 1986)
- Perform POCUS Cardiac Assessment
- Good Ejection Fraction
- Indicates vasodilation as source of hypotension
- 1st Line Pressor: Norepinephrine
- Poor Ejection Fraction
- Cardiac +/- peripheral vasodilation as source of hypotension
- Epinephrine – provides inotropy + vasopressor effects
- Dobutamine
- Inodilator – increases contractility while causing vasodilation
- Can consider as adjunct to inopressor if cardiac output
Take Home Points
- TCA toxicity can be fatal. Prompt recognition and treatment can significantly reduce mortality
- EKG findings can be pathognomonic and include QRS widening (> 100 msec) and rightward deviation of the terminal 40ms
- Do not administer physostigmine in an anticholinergic toxidrome until an EKG has been reviewed and the QRS is determined to be < 100 msec
- First line treatment is NaHCO3 1-2 mEq/kg
- In patients with significant hypotension, beside echocardiogram to evaluate for cardiac contractility can help guide pressor and inotrope treatment
References
Boehnert MT, Lovejoy FH. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after ran acute overdose of tricyclic antidepressant. N Engl J Med 1985; 313:474. PMID: 4022081
Jancin, B. Tricyclic Antidepressant Overdoses are on the Rise. ACEP News, Clinical and Practice Management. December 2007.
Liebelt EL. Chapter 73: Cyclic antidepressants. In: Goldfrank’s Toxicologic Emergencies, 9th ed, Nelson LS (Ed), McGraw-Hill, New York 2011.
Niemann JT et al. Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol. 1986;57:1154–1159. PMID: 3706169
TCA overdoses rarely seen these days as not used much for depression anymore, but don’t forget Cyclobenzaprine (Flexeril), probably the most useless “muscle relaxer” out there is a TCA and still being prescribed (and OD’d–with classic TCA toxicity). Also carbamazepine (Tegretol) has TCA properties…