Definition: Accumulation of blood within the pleural space resulting from blunt or penetrating injury to thoracic structures including the heart, mediastinum, lungs, great vessels, lung vasculature and chest wall.
Epidemiology:
- Associated with pneumothorax 25% of the time
- Associated with extra thoracic injuries 73% of the time
Signs + Symptoms:
- Shortness of breath, chest pain (pleuritic), dyspnea
- Decreased (or absent) breath sounds (high false-negative rate)
- Decreased tactile fremitus
- Depending on the volume of bleeding, patient may exhibit signs of hemorrhagic shock
Bleeding Sources
- Low pressure: lung parenchyma
- High pressure: intercostal artery, pulmonary artery, internal mammary artery
- Extra-thoracic: intraabdominal injuries with associated diaphragmatic injury
Diagnostic Imaging

Chest X-Ray Demonstrating Hemothorax – cardiothoracicsurery.org
- Chest X-ray (CXR)
- Blunting of the costophrenic angle
- Limitations: Requires 200-300 cc of fluid before blunting is visible
- Upright CXR remains the most frequent imaging modality for diagnosis
- Supine CXR less sensitive due to posterior layering of blood
- Findings
- Ultrasound (Carmody 2011)
- High sensitivity and specificity for detecting the presence and quantification of fluid in the pleural space
- Hemorrhage usually contains echogenic swirling material that moves in response to respiratory movement or the heart beat
- Best identified using a coronal view of the abdomen (RUQ and LUQ) with a low-frequency probe
- Twice as accurate as Xray in predicting the volume of a pleural effusion
- Higher sensitivity for detecting concomitant pneumothorax than CXR
- CT Scan
- Highest sensitivity and specificity for detecting blood within the pleural space
- Can distinguish between pleural effusion and hemothorax (US and CXR cannot)
- Excellent at diagnosing concomitant thoracic injuries (rib fractures, pulmonary contusions, great vessel injury etc)
- Limitations: May detect small hemothoracies that are clinically insignificant or of questionable significance, may not be appropriate for the unstable patient
Management:
Basics:
- ABCs, IV, O2, Cardiac Monitor, 12-lead EKG
- Make sure to examine the patient for all associated injuries as 73% of patients will have extrathoracic injuries
- Consider replacement of clotting factors in coagulopathic patients who are stable
- Analgesia as needed
Tube Thoracostomy
- Dual role: Treatment of the hemothorax and evaluation for additional intervention
-
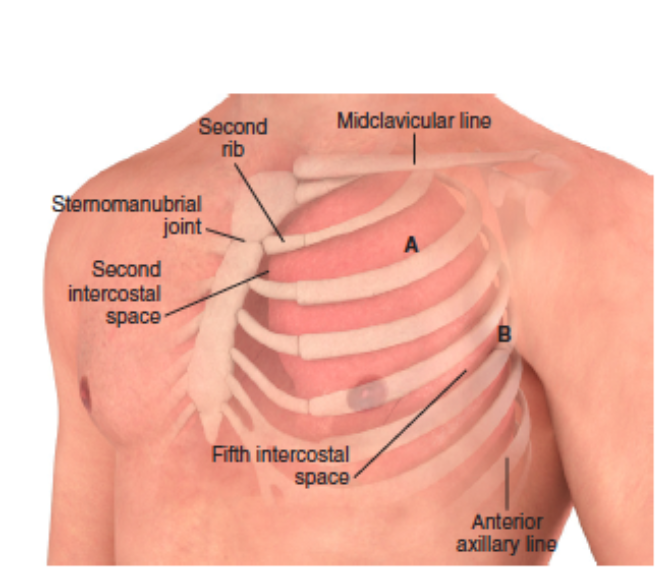
Chest Wall Anatomy – Roberts + Hedges
Procedure (see video below)
- Use standard precautions for personal protection and sterile technique as permitted by the situation
- Patient preparation
- If possible, position the patient with the head of bed up at 30-45 degrees. This position will lower the diaphragm
- Abduct the patient’s arm and place the hand behind the patient’s head
- Provide adequate analgesia with both local infiltration of anesthetic and systemic analgesics if needed. Local anesthetic should be administered over the rib
- Consider procedural sedation
- Identify 4th or 5th intercostal space in the midaxillary to anterior axillary line
- Estimate required tube depth: hold tube against chest wall with tip of tube at the level of the clavicle. Place clamp on tube to mark insertion length
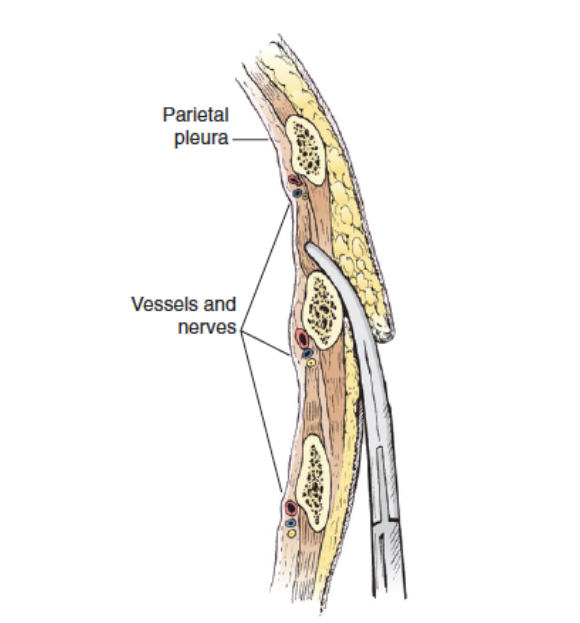
Placement Over the Rib – Roberts + Hedges
- Incision
- Make incision lateral to the edge of the pectoralis muscle, along the plane of the rib and over the superior surface of the rib
- Incision length should be 3-5 cm
- Place a Kelly clamp through the incision, over the rib (so as to avoid the neurovascular bundle) and push through the intercostal muscles and into the pleural space. Spread the clamp to move deeper tissue out of the way.
- When the clamp enters the pleural space, you will feel a “pop” as well as a rush of fluid and/or air
- Before removing the clamp, place your index finger over the clamp and into the pleural cavity so that the tract will not be lost. Your finger can be used to confirm that you are in the pleural cavity
- Place the thoracostomy tube (36-40 French) under your index finger (the one in the pleural space) and use this digit as a guide for the tube to follow into the pleural space.
- The tube should be directed posteriorly, medially and superiorly in the pleural space. Ensure that all drainage holes are in the pleural space
- Attach the tube to the water seal device.
- Secure the tube with sutures and place an occlusive dressing
- Pearls + Pitfalls
- External landmarks can be misleading – err towards the side of a more superior location to avoid penetration of the abdominal cavity
- Always place the chest tube over the rib so as to avoid the neurovascular bundle
- All drainage holes must be within the thoracic cavity in order for the tube to drain effectively
- Make a large enough incision (at least 3-5 cm) to accommodate a hemostat and your fingers. If the incision is too small, it is easy to lose the track
- Always have a clamp or finger in the pleural space so as not to lose the tract that you created
- Beware of sharp edges associated with rib fractures
Post-Tube Thoracostomy Management
- Prophylactic antibiotics
- Inadequate literature to support use but is recommended by the Eastern Association of Surgeons of Trauma (EAST)
- Antibiotic Choice: 1st generation cephalosporin
- Broader coverage if suspected thoraco-abdominal/bowel injury
- Tube Placement Confirmation
- Bedside:
- Check for free flow of blood in the tube
- Check that tube can freely rotate 360o
- CXR offers definitive assessment
- Bedside:
Complications
- Infection
- Iatrogenic injury to the lung parenchyma or intercostal arteries
- Inadvertent placement into the abdominal cavity leading to solid organ injury
- Residual/retained hemothorax (from inadequate drainage) can provide a nidus for infection and development of empyema
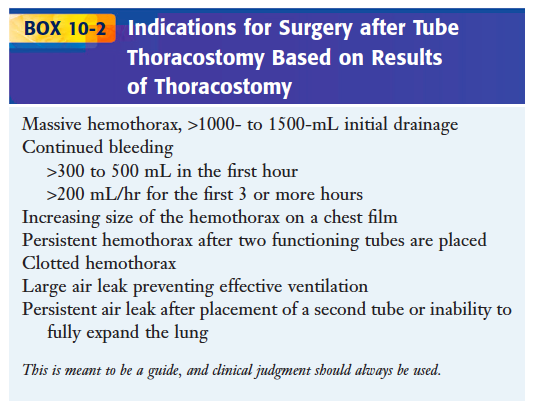
Indications for Surgery After Chest Tube – Roberts + Hedges
Additional Management
- Blood transfusion to maintain hemodynamic stability
- Correction of coagulation factor deficiencies as needed
- A select group of patients with traumatic hemothorax will require further surgical intervention (>1000 cc immediate drainage or continued bleeding 200cc/hr post-tube thoracostomy)
- Procedures include thoracotomy and video-assisted thoracoscopic treatment (VATS)
Take Home Points
- Always look for concomitant extra-thoracic trauma in patients with hemothorax
- Hemothoracies should be emergently drained by performing a tube thoracostomy
- Tube thoracostomies should be placed in the 4th or 5th intercostal space over the rib with care to ensure entry into the thorax and not the abdomen
- If initial drainage is > 1000-1500 mL or their is continued brisk output (> 300-500 mL in the first hour or > 200 mL every hour for the next 3 hours) consult trauma surgery for emergent OR management
References:
Kirsch TD, Sax J: Tube Thoracostomy, in Roberts JR, Hedges JR, Custalow CB, et al (eds): Clinical Procedures in Emergency Medicine, ed 6. Philadelphia, Saunders, 2013, Ch 10:p 189-203.
Eckstein M, Henderson SO: Thoracic Trauma; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 45: p 431–460.
Carmody, K., Moore, C., Feller-Kopman, D. “Thoracic Ultrasound.” Handbook of Critical Care and Emergency Ultrasound. New York: McGraw-Hill Medical, 2011.
University of Maryland Emergency Medicine: Tube Thoracostomy

Hello Dr. Swaminathan,
I am an emergency medicine resident in British Columbia and am preparing a talk on hemothorax treatment in the context of trauma. There has been some recent literature on whether a 28F chest tube is an adequate size from Dr. Inaba. In the above discussion it mentions using a 36-40 F chest tube. Are you still recommending this practice or encouraging smaller 28 F chest tubes now?
Cheers,
Derek – Great question. I think moving to a smaller tube is going to be site dependent and really rely on your trauma team and what they are comfortable with. Our surgeons at this time are more comfortable with larger chest tubes but I think it’s very reasonable to go with a smaller one and see how the patient does. You can always consider putting in a larger one if you’re not happy with drainage. All of this would be in stable patients. In unstable ones, I’d reach for the larger tube.
Well-illustrated and organized contribution, thanks