 Definition: A life-threatening, pathologic state in which the body manifests a myriad of symptoms ranging from high-output cardiac failure to severe alterations of mental status in response to excess circulating thyroid hormone
Definition: A life-threatening, pathologic state in which the body manifests a myriad of symptoms ranging from high-output cardiac failure to severe alterations of mental status in response to excess circulating thyroid hormone
- Hyperthyroidism: Disorders resulting from overproduction of thyroid hormone
- Thyrotoxicosis: Disorders resulting from any cause of excess thyroid hormone
Epidemiology (Nayak 2006)
- Rare condition that is more common in women (80/100,000 per year) than in men (8/100,000 per year)
- Extremely rare in children (0.9/100,000 per year)
- Most cases are due to Graves’ disease
Hyperthyroidism Etiologies
- Graves’ disease
- Toxic adenoma (single responsible nodule)
- Toxic multinodular goiter
- Thyrotoxicosis with thyroiditis
- Hashimoto’s thyroiditis
- Subacute thyroiditis
- Postpartum thyroiditis
- Exogenous thyroid hormone abuse
- Iatrogenic (i.e.) Amiodarone induced thyroiditis
- Oncologic
- TSH-producing pituitary tumor
- Metastatic follicular thyroid carcinoma
- hCG-mediated thyrotoxicosis
- Hydatidiform mole
- Metastatic choriocarcinoma
Precipitants of Thyroid Storm
- Untreated/undertreated thyroid disease (i.e. medication non-compliance)
- Trauma (direct trauma or as a result of stress to body)
- Thyroid or non-thyroid surgery
- Iodinated contrast (typically in susceptible patients with Graves’ disease or multi nodular goiter)
- Myocardial infarction/ischemia
- Infection
- Diabetic Ketoacidosis/Hyperosmolar Nonketotic Coma
- Ingestion of thyroid hormone
Pathophysiology
- T4 produced by the thyroid is deiodinated to the more active T3 form
- Most (> 99%) of thyroid hormone is protein bound and, thus inactive. Only free thyroid hormone is metabolically active
- Thyroid hormone affects metabolism in all tissues in the body via a variety of mechanisms
- Thyroid hormone increases the expression and sensitivity of beta-adrenergic receptors resulting in an increased response to endogenous catecholamines (this accounts for many of the symptoms seen in thyroid storm)
- Wolff-Chaikoff Effect: Excess iodide transiently inhibits thyroglobulin iodination and release of thyroid hormone
- Jod-Basedown Effect: Iodide load induces hyperthyroidism in susceptible subgroups (i.e. Graves’ disease, multi nodular goiter)
Clinical Manifestation
- Classic presentation: fever, tachycardia and altered mental status
- See below for common additional symptoms and signs
| Organ System | Symptoms | Signs |
| CNS | Anxiety
Confusion |
Delirium
Psychosis Lethargy Seizures Coma Hyperreflexia |
| Cardiovascular | Palpitations
Chest Pain Dyspnea on exertion |
Sinus Tachycardia
Atrial fibrillation Widened pulse pressure Heart failure |
| Gastrointestinal | Abdominal pain
Nausea Vomiting Diarrhea |
Jaundice |
| Thyroid Gland | Neck fullness | Tenderness over thyroid
Diffuse enlargement Bruit |
Diagnosis
- Diagnosis is made based on clinical evaluation not serum testing
- Serum testing results are often delayed or unavailable in many institutions
- TSH, T3/T4 are unreliable in acute decompensated states
- Burch-Wartofsky Scale (Burch 1993)
- Most commonly used system for diagnosing thyroid storm
- Does not rely on any laboratory values allowing for rapid recognition and diagnosis
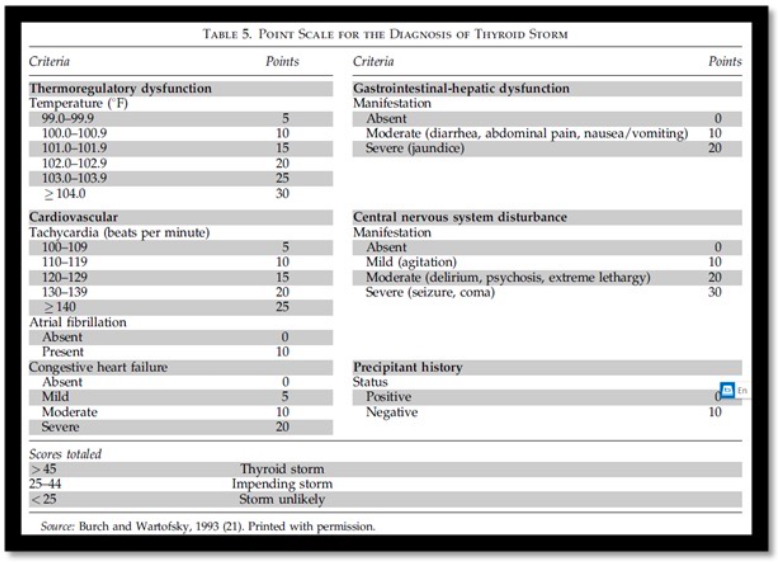
Burch Wartofsky Scale (adapted from Burch 1993)
- Common laboratory findings
- Low (or non-detectable) TSH and elevated T3/T4
- Hyperkalemia + hyponatremia (in concomitant adrenal insufficiency)
- Anemia
- Thrombocytopenia
- Low serum creatinine
- Hypercalcemia
Management Basics
- Evaluate and address airway and breathing
- Establish IV access
- Place patient on cardiac monitor
- Active cooling measures including ice packs and cooling blankets may be necessary if patient with severe hyperthermia
- Consider empiric fluid administration
- Insensible fluid losses from fever can be high in these patients
- High output cardiac failure is common and preload should be maintained in these patients
- Add dextrose to fluids (patients often have depleted glycogen stores)
- Consider empiric broad spectrum antibiotics
- Signs and symptoms in thyroid storm mimics sepsis and distinguishing the two can be difficult
- Infection is a leading precipitant for thyroid storm
Directed Management
-
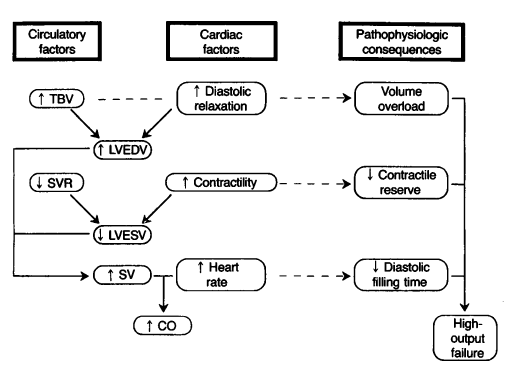
Cardiovascular Effects of Thyrotoxicosis – Woeber 1992
Block peripheral effects of thyroid hormone with beta blocker (Woeber 1992)
- Propranolol most commonly used
- Non-selectvie beta blockade effectively treated systemic effects
- Additional benefit of blocking conversion of T4 to T3
- Dose: 0.5 – 1 mg IV over 3-5 minutes
- Can repeat dose q5-10 minutes
- Titrate to HR < 100
- Keep a close eye on blood pressure
- Esmolol
- Can be substituted if concern for hemodynamic collapse
- Dose
- Load: 250-500 mcg/kg
- Infusion: 50-100 mcg/kg/min
- Role of beta blocker with signs of heart failure
- Heart failure typically high-output and beta blockade will still be beneficial
- Start slow with test dose and follow response prior to additional doses
- Propranolol most commonly used
- Inhibit thyroid hormone synthesis
- Propylthiouracil (PTU)
- Dose
- Load: 600-1000 mg PO
- 300 mg PO Q6
- Impairs conversion of T4 to T3
- Preferred in pregnancy
- Dose
- Methimazole: 20-30 mg Q6 hours
- Both drugs can be given PO, NG or PR
- Propylthiouracil (PTU)
- Administer corticosteroids
- Function
- Block conversion of T4 to T3
- Block release of hormone from the thyroid gland
- Concomitant adrenal insufficiency is common
- Hydrocortisone: 100 mg IV Q8 hours
- Dexamethasone
- Dose: 2-4 mg IV Q6 hours
- Preferred if unsure if adrenal insufficiency present and will be doing cortisol stimulation testing later
- Function
- Inhibit thyroid hormone release with inorganic iodine
- Mechanism of action
- Blocking synthesis does not stop release of preformed thyroid hormone
- Blocks release of stored thyroid hormone
- Can increase synthesis of thyroid hormone so should be held for at least 1 hour after initiation of PTU
- Medication options
- Potassium Iodide (SSKI): 5 gtt Q6 hours
- Lugol’s solution: 4-8 gtt Q6 hours
- Lithium 300 mg Q6-8 hours (alternative if SSKI/Lugol’s contraindicated)
- Mechanism of action
- Additional interventions
- Cholestyramine
- Blocks enterohepatic recirculation of thyroid hormone
- Dose: 4 g PO Q6 hours
- L-Carnitine
- Blocks entry of thyroid hormone into cells
- Dose: 1 g PO Q12 hours
- Cholestyramine
- Disposition: Admit to ICU or other highly monitored unit
Take Home Points
- Thyroid storm is a clinical diagnosis and should be suspected in any patient with fever, altered mental status
- Diagnosis can be rapidly made using the Burch-Wartofsky scale. This allows for rapid initiation of treatment and reduction of morbidity and mortality
- Strongly consider covering all thyroid storm patients with broad spectrum antibiotics because of the frequency of concomitant infection
- Directed management starts with beta blockade to reduce the peripheral effects of thyroid hormone. This should be followed by corticosteroids, thionamides and inorganic iodine
Read More
EM: RAP: Episode 105 – Hyperthyroidism
ALiEM: Diagnosing hyperthyroidism: Answers to 7 common questions
ALiEM: Thyroid Storm – Treatment Strategies
LITFL: Thyroid Storm
WikeEM: Burch and Wartofsky Diagnostic Criteria for Thyroid Storm
Sharma AN, Levy DL: Thyroid and Adrenal Disorders; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 128: p 1676-94.
References
Nayak B, Burman K. Thyrotosicosis and thyroid storm. Endocrinol Metab Clin N Am 2006; 35: 663-686. PMID: 17127140
Burch HB, Wartofsky L: Life-threatening thyrotoxicosis: Thyroid storm. Endocrinol Metab Clin North Am 22:263-277, 1993. PMID: 8325286
Woeber KA. Thyrotoxicosis and the heart. NEJM 1992; 327(2): 94-8. PMID: 1603141
Franklyn JA. The management of hyperthyroidism. NEJM 1994; 330: 1731-8. PMID: 7910662
