10 Can’t Miss Diagnoses of the Red Eye
- Acute angle-closure glaucoma (AACG)
- Bacterial keratitis/ulcer
- Endophthalmitis
- Hyphema
- Hypopyon
- Iritis
- Infectious keratitis (bacterial and viral)
- Orbital cellulitis
- Scleritis
- Uveitis
HPI
- Age
- Especially neonate vs >50 years old
- Timing
- Nature of onset, duration of symptoms
- Exposures
- Ask about chemicals, allergens, etc.
- Associated signs and symptoms
- Headache
- Neurological symptoms
- Systemic symptoms
- Consider asking about infectious symptoms especially recent URI symptoms such as cough, congestion, or runny nose
- Recent trauma
- Remember to consider patients coming from high-risk work environments (e.g., power-saw users) who are at increased risk of foreign bodies (FB)
- If painful, obtain specific characteristics of pain[1]
- Up-front, scratchy, ‘sand-in-the-eye’ type of pain often refers to anterior structures such as the eyelid, conjunctiva, and cornea, as well as foreign bodies
- Deep, boring, ‘behind-the-eye’ pressure-type pain relates to posterior structures
- Photophobia
- This may indicate involvement of the uveal tract (iris, ciliary muscles, choroid)
- Vision changes
- Less commonly associated with eye redness, but should prompt concern for our urgent/emergent diagnoses or refer to your vision-loss differential
- Contact use
- These patients are at higher risk for infections, which tend to be rapidly progressive
- For all ophthalmologic pathology, recommend using glasses instead of contact lenses until follow up and/or resolution of symptoms
Differential Diagnoses
A brief differential for a PAINFUL red eye based on symptom description:
- Itching => allergies
- Burning => lid disorders, dry eye
- FB sensation => FB, corneal abrasion
- Localized lid tenderness => hordeolum, chalazion
- Deep, intense pain => corneal abrasion, scleritis, iritis, acute glaucoma, sinusitis, orbital cellulitis
- Photophobia => corneal abrasions, iritis, acute glaucoma (think about ciliary body muscle spasm or other problems from the anterior segment of the eye)
- Halo vision => acute glaucoma, uveitis (resulting from corneal edema)
A brief differential for a PAINLESS red eye based on location:
- Diffusely red: conjunctivitis or episcleritis, but also consider eyelid abnormalities that may have an associated conjunctivitis (e.g., blepharitis, ectropion, entropion, eyelid lesion like tumor or stye)
- Localized redness: subconjunctival hemorrhage, pterygium, corneal foreign body (usually painful), ocular trauma (usually painful)
reference: Overview of Uveitis by Kara LaMattina, MD (https://www.merckmanuals.com/professional/eye-disorders/uveitis-and-related-disorders/overview-of-uveitis)
Examination Toolbox (in order of real-time usage)
- Penlight examination
- Take a direct look using a penlight (or your phone light) to examine the eyelids and conjunctivae
- Visual acuities
- Should be performed on every patient with an eye complaint
- Know where your department’s Snellen chart is or have a handheld version (physical or digital) for quick use
- Visual fields
- Less useful for the red-eye complaint, but can be useful when assessing visual disturbances
- Pupillary assessment
- Need to assess pupillary response to light, including a swinging light test to assess for an afferent pupillary defect (APD)
- If having photophobia, must determine if direct or consensual photophobia: consensual photophobia is highly suggestive of iritis
- Extraocular movements
- Testing CN III, IV, and VI
- A quintessential portion of the exam in traumatic complaints and in those concerning for infection posterior to the globe
- Pain with eye movement is concerning for extraocular muscle (EOM) entrapment (potentially in a fractured orbital wall) or infection causing irritation of the EOMs
- Fluorescein uptake
- Apply a topical anesthetic first (such as tetracaine), followed by application of a fluorescein strip to the lower eye lid (palpebral conjunctiva) and allow time for it to spread throughout
- Examine the superficial aspects of the eye using a blue light to identify multiple forms of keratitis, abrasions, and evidence of FBs
- Phenylephrine testing
- Induces constriction of superficial blood vessels, thus can be helpful differentiating between redness causes by hemorrhage vs conjunctival vessels vs scleral vessels
- Intraocular pressure measurements
- Apply your topical anesthetic prior to performing a pressure assessment
- Measure the unaffected eye as well for control
- Normal IOP = 12 to 22 mmHg
- Used primarily to identify or rule out AACG and other etiologies that may increase pressures behind the eye (e.g., orbital cellulitis, cavernous sinus thrombosis, retrobulbar hematoma)
- Do NOT perform if there is a suspicion for globe rupture
- Slit lamp examination of the anterior segment
- Used primarily for evaluation of the anterior chamber (AC), but also provides a magnified look at all superficial structures (lids, conjunctivae, etc.).
- Examine for cell or flare within the AC, pinpoint or dendritic lesions, corneal abrasions, foreign body, and perform lid eversion
- Fundoscopy of the posterior segment
- Rarely needed for evaluation of the red eye, but often useful when prompted with vision changes

Approach to the PainFUL Red Eye
- Obtain your history and basic bedside examination
- Itching => allergy
- Burning => lid disorders, dry eye
- FB sensation => FB, corneal abrasion
- Localized lid tenderness => hordeolum, chalazion
- Deep, intense pain => corneal abrasion, scleritis, iritis, acute glaucoma, sinusitis, orbital cellulitis
- Photophobia => corneal abrasions, iritis, acute glaucoma (consider ciliary body muscle spasm or other problems from the anterior segment of the eye)
- Halo vision => corneal edema (acute glaucoma, uveitis)
- Perform fluorescein uptake testing
- Branching = viral keratitis
- Round = bacterial keratitis
- Neither = corneal abrasion
- Pinpoint/punctate = UV keratitis
- Measure intraocular pressures
- If elevated, consider AACG
- Slit lamp examination
- Cell and flare represent an acute infection of the anterior chamber
- Differentiate based on history:
- Consider uveitis if underlying autoimmune/rheumatologic conditions
- Consider endophthalmitis if severe symptoms or risk factors (e.g., recent eye surgery, trauma within 24hr, FB, recent keratitis, or systemic infection)
- If exam is negative to this point, consider scleritis without uveitis
Approach to the PainLESS Red Eye
- Obtain your history and basic bedside examination
- Diffusely red: consider conjunctivitis or episcleritis, but also eyelid abnormalities that may have an associated conjunctivitis (e.g., blepharitis, ectropion, entropion, eyelid lesion like tumor or stye)
- Localized redness: subconjunctival hemorrhage, pterygium, corneal foreign body (usually painful), ocular trauma (usually painful)
- Apply phenylephrine
- Consider subconjunctival hemorrhage and scleritis if no improvement
- Consider conjunctivitis and episcleritis if there is improvement
- Conjunctivitis often has diffuse redness with tarsal involvement (+/- URI symptoms)
- Episcleritis often has focal redness
Diagnosis Index and Management
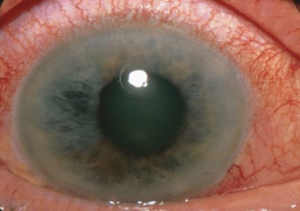
Acute Angle Closure Glaucoma
- Definition: Closure/narrowing of the AC angle, causing elevated intraocular pressure and eventual optic nerve damage[1]
- Risk factors: Increased age, female gender, Asian ethnicity, hyperopia (farsightedness)
- Symptoms: HA, n/v, photophobia, blurred vision, “deep” pain (no improvement with topical anesthetics)
- Exam/Diagnostics: Diffuse redness and characteristic ciliary flush, elevated IOP, can also see a shallow anterior chamber (AC), mid-sized or dilated and non-reactive pupils, decreased visual acuities (VA), no fluorescein uptake
- Management Pearls: lower IOP in preparation for definitive treatment by ophthalmology
- Topical parasympathomimetics to facilitate outflow of aqueous humor (e.g., pilocarpine 1-2% 1drop in affected eye every 15 minutes x2-4 doses, then every 4-6 hours)
- Topical beat-blocker (e.g., timolol 0.5% 1 drop in affected eye, repeat in 1 hour if needed) – caution in asthmatics, COPD, and patients in heart block
- Carbonic anhydrase inhibitors (e.g., acetazolamide 500mg IV or PO) – avoid in sickle cell patients and possibly in sulfa-allergic patients
- Alpha agonists to increase trabecular outflow (e.g., brimonidine 0.2% or apraclonidine ophthalmic 1%, 1 drop in affected eye) – avoid in patient’s on MAOI’s
- Ophtho Consult? Emergent
Allergic Conjunctivitis
- Definition: A sudden-onset hypersensitivity reaction caused by environmental exposure, usually a known allergen. Can be acute or seasonal
- Risk factors: Prior exposure
- Symptoms: Ocular pruritus, possible burning sensation, diffuse redness, eyelid edema, +/- mild photophobia. Should not be painful. May be associated with allergic rhinitis (edema of nasal turbinates and rhinorrhea). Symptoms usually bilateral, although on eye can be affected more than the other
- Exam/Diagnostics: Redness, tearing or clear watery discharge, conjunctival edema, conjunctival papillae underneath eyelid (but no cobblestoning or giant papillae). Diagnosis is made clinically
- Management Pearls: Symptomatic treatment, avoid contact lenses, and most importantly, hand hygiene; if painful, unilateral, or severe symptoms, consider alternative diagnoses
- Ophtho Consult? None
Anterior Uveitis
- Definition: Inflammation of the iris, choroid, and/or ciliary body
- Risk factors: idiopathic systemic diseases (spondyloarthropathies), infectious (syphilis, Lyme’s, toxoplasmosis, CMV), drug induced
- Symptoms: Pain (no improvement with topical anesthetics), redness, photophobia (direct and consensual), tearing, decreased vision
- Exam/Diagnostics: Diffuse redness with ciliary flush, “cell and flare” in AC, constricted pupil, normal or decreased VA, possible +fluorescein (in viral uveitis)
- Management Pearls: can treat specific etiology if suspected; dilating drops, +/- steroids in conjunction with ophtho
- Ophtho Consult? Urgent (within 24 hours)
Bacterial Keratitis/Ulcer
- Definition: Corneal epithelial defect with “stromal” haze due to microorganism[2]
- Risk factors: Contact lens users[3], agricultural work[4], eye trauma, history of corticosteroid use, systemic diseases (e.g., DM), prior ocular surgery, chronic ocular surface disease
- Symptoms: Significant pain (may improve with topical anesthetic), tearing, and discharge, photophobia
- Exam/Diagnostics: Diffuse redness, normal VA (may be decreased if involving visual axis), normal pupils, possible cell and flare on AC examination; +Fluorescein uptake (large, over area of ulceration)
- Management Pearls: Fortified topical antibiotics (Tobramycin 14 mg/ml 1 drop q1h, can alternate with fortified cefazolin 50mg/ml 1 drop q1h). Smaller corneal ulcers may be treated with moxifloxacin or gatifloxacin ophthalmic.
- Ophtho Consult? Emergent
Conjunctivitis
- Definition: Infectious or non-infectious inflammation of the bulbar and palpebral conjunctiva
- Risk factors: Exposure to infectious viruses or bacteria
- Symptoms: Tearing and discharge, often associated with viral symptoms, may have mild burning pain (that improves with topical anesthetics) without photophobia (if present, should consider alternative diagnoses)
- Exam/Diagnostics: Diffuse redness (tarsal/palpebral conjunctiva SHOULD be involved), usually +discharge, normal VA, normal pupils, clear AC, no fluorescein uptake
- Management Pearls: Artificial tears, consider topical abx for suspected bacterial conjunctivitis (ciprofloxacin 0.3% 1-2 gtt q1-6h for contact lens wearers); avoid contact lenses; recommend contact precautions and increased hygiene due to highly contagious nature of viral/bacteria conjunctivitis; consider Neisseria gonorrhoeae conjunctivitis in patients with severe discharge and obtain conjunctival swab for routine culture and sensitivity
- Ophtho Consult? None – can follow up with PCP as needed
Corneal Abrasion/Foreign Bodies
- Definition: Defect or FB of the corneal epithelium causing irritation, pain, tearing, and photophobia[5]
- Risk factors: History of trauma, contact lens use, male gender, young adults, construction or manufacturing job w/o eye protection (FB)
- Symptoms: Pain (improves with topical anesthetic), photophobia, watering/teary eyes, sensation of FB
- Exam/Diagnostics: Diffuse redness, usually normal VA but may be decreased if within visual axis (if decreased, consider alternative diagnoses), pupils normal, AC clear; +Fluorescein uptake at corneal abrasion or site of FB
- Management Pearls: If abrasion, eval for FB (including lid eversion), lubricating drops, topical abx (erythromycin ointment q4h; pseudomonal coverage for contact lens wearers with tobramycin, ofloxacin, or ciprofloxacin drops QID). If corneal FB, remove by EP or ophtho, topical abx. Update tdap
- Ophtho Consult? Urgent for contact wearers; Emergent if concerning for corneal ulcer (i.e., obvious ulcer present on exam or +hypopyon or pain not improving after 24h)
Dry Eye
- Definition: Multifactorial disease of tears and ocular surface resulting in discomfort and visual impairment
- Risk factors: Advanced age, female gender, hormonal changes, systemic diseases (e.g., DM, Parkinson’s, Sjogren’s), contact lens user, ophthalmic surgeries, low-humidity environments
- Symptoms: Eye irritation, redness, dryness, burning
- Exam/Diagnostics: Conjunctival injection, possible reduced blink rate. Visual acuities normal or decreased; may improve with increased blink rate or lubricants; may be permanently decreased in severe cases. Fluorescein may show punctate staining from epithelial erosions. AC should be otherwise normal
- Management Pearls: Artificial tears for all patients, environmental coping strategies, warm compresses. If no improvement or with history of neuropathy (e.g., diabetic), should follow up with ophthalmology
- Ophtho Consult? Non-emergent
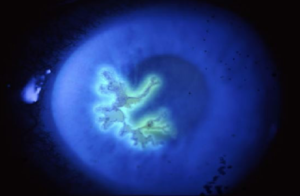
Endophthalmitis
- Definition: Bacterial or fungal infection involving the vitreous and/or aqueous humor
- Risk factors: Recent eye surgery, penetrating ocular trauma, corneal infection, intravitreal injections, recent hospitalization with central access, TPN, or broad spectrum abx
- Symptoms: Pain (no improvement with topical anesthetics) and decreased vision, +photophobia
- Exam/Diagnostics: Diffuse redness, commonly associated with hypopyon, likely decreased VA, possible APD in severe cases, +fluorescein if penetrating injury
- Management Pearls: Emergent Ophtho consult for gram stain/culture and definitive treatment via intravitreal injection of antibiotics vs surgery
- Ophtho Consult? Emergent
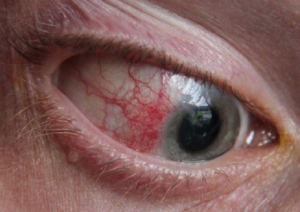
Episcleritis
- Definition: Inflammation of the episcleral, which is vascularized tissue between conjunctiva and sclera7
- Risk factors: 70% female, fifth decade of life, 1/3 related to systemic autoimmune conditions7
- Symptoms: Ocular redness w/o irritation or slight tenderness; may have mild irritating pain (may improve w/ topical anesthetics) without photophobia
- Exam/Diagnostics: Commonly with redness diffusely (interpalpebral zone = area between eyelids), VA normal, pupils normal, AC clear, no fluorescein uptake. Inflamed vessels CAN be moved with cotton tipped applicator
- Management Pearls: Topical lubricants[6], oral NSAIDs, return precautions related to scleritis
- Ophtho Consult? None – PCP follow up and recommend workup for possible autoimmune disease
Foreign Body
See “Corneal Abrasion/Foreign Bodies” above
Hordeolum/Chalazion
- Definition: A pustule of the eyelid due to blockage and infection of sebaceous or sweat glands (external) or from blockage of the meibomian glands (internal)
- Risk factors: Skin conditions affecting the eyelids (e.g, rosacea and seborrheic dermatitis)
- Symptoms: Hordeolum will have focal pain, edema, and erythema of the eyelid; chalazion often appears similar but tend to be painless and less erythematous and angry appearing
- Exam/Diagnostics: Focal area of swelling +/- redness and tenderness to the eyelid, either internal or external
- Management Pearls: Warm compresses (15 min QID), avoid eye makeup and contact lenses, oral antibiotics if there is concurrent periorbital cellulitis (rare). There is little evidence to suggest topical antibiotics are helpful
- Ophtho Consult? None – can be referred routinely if persistent
Orbital Cellulitis
- Definition: Infection of soft tissues of the eye socket, difficult to distinguish from periorbital cellulitis
- Risk factors: Ethmoid sinusitis, recent orbital trauma, endophthalmitis, or infections from teeth/middle ear
- Symptoms: Pain, swelling, and redness of eye and surrounding tissue. May note proptosis.
- Exam/Diagnostics: Swelling and erythema AND proptosis, chemosis, globe displacement, limitation of EOM’s, pain w/ eye movements, double vision, decreased visual acuities, possible CN III, IV, VI palsies in cases w/ cavernous sinus involvement. CT Orbit w/ IV contrast is preferred imaging modality.
- Management Pearls: Vancomycin 15-20 mg/kg IV BID plus one of the following:
- Ampicillin/Sulbactam 3 g IV q6hr OR
- Ticarcillin/Clavulanate 3.1 g IV q4h OR
- Piperacillin-Tazobactam 4.5 g IV q6h OR
- Ceftriaxone 2 g IV q12hr OR
- Cefotaxime 2 g IV q4h
- Consider fungal infections with mucor or aspergillus in DM or immunocompromised
- Amphotericin B IV 0.3 mg/kg/day initially
- May require supplemental intra-orbital catheter delivery
- Ophtho Consult? Emergent and admit patient for IV abx
Hyphema
- Definition: Blood visible within the anterior chamber of the eye
- Risk factors: Blunt trauma to the orbit. Non-traumatic causes include sickle cell disease, ocular or laser surgery, HSV/VZV uveitis, neoplastic, blood thinners
- Symptoms: Eye pain, vision loss, nausea/vomiting
- Exam/Diagnostics: Blood w/in AC, direct and consensual photophobia, vision loss or VA changes, may find co-existing corneal abrasion, assess for ruptured globe in traumatic cases then check IOPs, inquire about blood thinners
- Management Pearls: Elevate head of bed (HOB), eye shield, control pain/nausea, consider discontinuation of NSAIDs/ASA/anticoagulants. If IOPs elevated, treatment is similar to glaucoma including beta-blockers, alpha adrenergics, and CA inhibitors. Consider cycloplegic for comfort (decreases pupillary constriction/dilation movements which may cause irritation and further bleeding) such as tropicamide (1-2 drops of 0.5-1%, may repeat in 5m), homatropine (1-2 drops of 2-5% q3-4h), or cyclopentolate (1-2 drops of 0.5-2%, may repeat in 5-10 min if needed). Treat underlying coagulopathy.
- Ophtho Consult? Urgent in ER to determine dispo based on examination
Hypopyon
- Definition: A leukocytic exudate within the anterior chamber
- Risk factors: corneal ulcer, Behcet’s disease, endophthalmitis, uveitis, recent eye surgery or trauma
- Symptoms: Exudate within AC accompanied by redness of conjunctiva
- Exam/Diagnostics: Slit lamp exam notable for exudate within the AC
- Management Pearls: Should not be drained. If long-standing, can cause glaucoma. Consider intravitreal antibiotics (via ophthalmology consult) if endophthalmitis is suspected
- Ophtho Consult? Emergent
Scleritis
- Definition: Painful, sight-threatening cause of acute red eye
- Risk factors: 50% autoimmune systemic disease (rheumatoid arthritis, Wegener’s granulomatosis), 4-10% infectious[7]
- Symptoms: Gradual onset, severe boring pain (no improvement with topical anesthetic), typically worse at night
- Exam/Diagnostics: Diffuse or localized redness, may have bluish hue. Pain worse w/ EOMs, possible photophobia, normal/decreased VA, normal pupils, possible associate anterior uveitis on AC examination. On fluorescein, may have keratitis. Inflamed vessels cannot be moved with cotton tipped applicator
- Management Pearls: Systemic NSAIDs or immunosuppressive therapy[8], workup for systemic disease
- Ophtho Consult? Emergent
Subconjunctival Hemorrhage
- Definition: Blood under the conjunctiva secondary to ruptured conjunctival blood vessel (can be from coughing, straining, trauma)
- Risk factors: Recent trauma, excessive straining (e.g., coughing, sneezing, vomiting), conjunctivitis, chronic health conditions (e.g., DM, HTN, coagulopathy)[9]
- Symptoms: None
- Exam/Diagnostics: Focal redness, remainder exam normal (including VA, pupils, AC, and fluorescein); rule out penetrating injury to globe
- Management Pearls: Supportive care. If 360 degrees of hemorrhage, should be concerned for globe rupture
- Ophtho Consult? None – can follow up with PCP as needed
UV Keratitis
- Definition: Acute keratitis syndrome that occurs after UV irradiation of the eyes. Can have latent period of 6-12 hours and patient may be unaware of exposure (e.g., snowblindness)
- Risk factors: Recreational or occupational activities associated with UV exposure in conjunction with unprotected eyes
- Symptoms: Significant pain (may improve with topical anesthetic), tearing, and discharge, photophobia
- Exam/Diagnostics: Diffuse redness with tearing and edema (chemosis). No involvement in tarsal conjunctiva (differentiates this from conjunctivitis). Possible swelling/erythema of face and lids. +Fluorescein uptake (diffuse punctate staining). Normal VA (may be decreased if involving visual axis), normal pupils, normal AC exam
- Management Pearls: Supportive care with oral analgesics (pain is severe so may require opioids) and lubricant antibiotic ointments (for comfort and prophylaxis for superinfection[10])
- Ophtho Consult? Routine follow up as outpatient or sooner if new or worsening symptoms
Uveitis/Iritis
See Anterior Uveitis above
Viral Keratitis
- Definition: Corneal inflammation caused by HSV, VZ, or adenovirus characterized by pain, tearing, photophobia, and corneal defects
- Risk factors: HSV-1 (most common), HSV-2, VZV, and adenovirus[11]
- Symptoms: Pain (no improvement w/ topical anesthetic), tearing, photophobia. VZV may have Hutchinson’s sign (vesicular lesion on nose)[12]. HSV may also have vesicular rash elsewhere
- Exam/Diagnostics: Diffuse redness with ciliary flush, normal/decreased VA, normal pupils. Possible cell and flare on AC examination. Fluorescein with variable findings – HSV w/ branching pattern w/ terminal bulbs; VZV w/ branching pattern w/ tapered ends; EKC w/ diffuse find keratitis
- Management Pearls: Topical and/or oral antivirals. +/- topical steroids in conjunction with ophthalmology ONLY
- Ophtho Consult? Emergent
Images
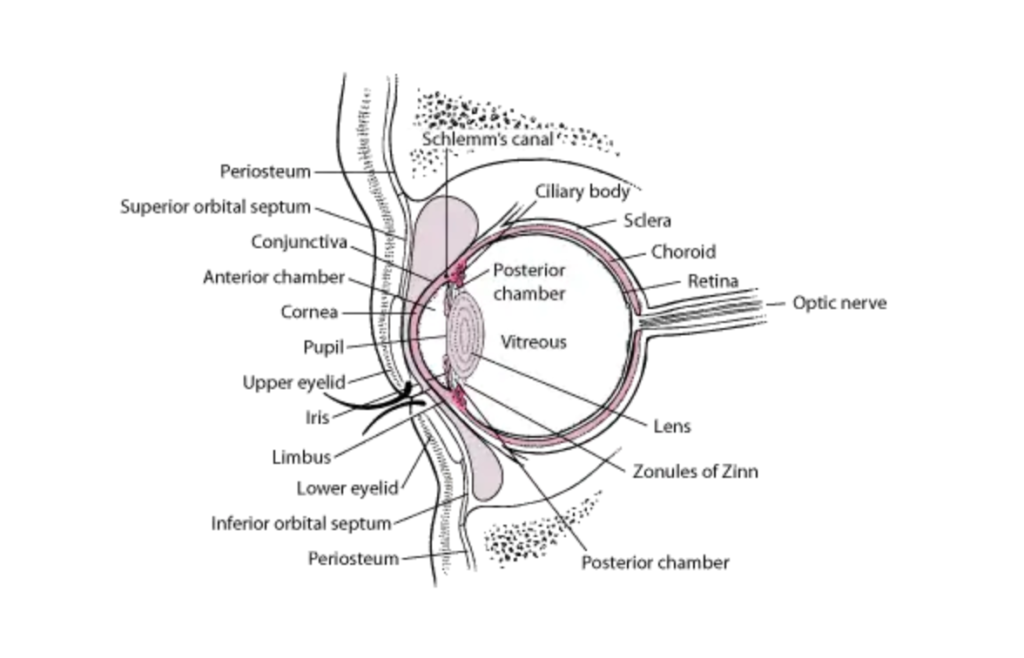
Acute angle closure glaucoma. Take note of the steamy cornea and mid range pupil. [reference: Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)]
Anterior uveitis. [reference: Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)]
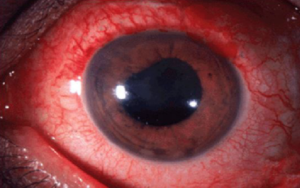
Endophthalmitis. [reference: Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)]

Episcleritis. [reference: Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)]
Viral keratitis. [reference: Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)]
References
[1] Helman, Anton, et al. “Nontraumatic Eye Emergencies.” Emergency Medicine Cases, 20 Aug. 2019, emergencymedicinecases.com/episode-9-nontraumatic-eye-emergencies/.
[2] Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle-closure glaucoma: an update. Acta Ophthalmol. 2016;94(3):217-225. doi: 10.1111/aos.12784
[3] Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113(1):109-116. doi: 10.1016/j.ophtha.2005.08.013
[4] Shah R, Shah M, Khandekar R, Al-Raisi A. Contact lens induced corneal ulcer management in a tertiary eye unit in woman – a descriptive study. Sultan Qaboos Univ Med J. 2008;8(3):283-290.
[5] Thomas PA, Geraldine P. Infectious keratitis. Curr Opin Infect Dis. 2007;20(2):129-141. doi: 10.1097/QCO.0b013e328017f878
[6] Prum BE Jr., Herndon LW Jr., Moroi SE, Mansberger SL, Stein JD, Lim MC, et al. Primary angle closure preferred practice pattern guidelines. Ophthalmology. 2016;123(1):1-40. doi: 10.1016/j.ophtha.2015.10.049
[7] Williams CP, Browning AC, Sleep TJ, et al. A randomised, double-blind trial of topical ketorolac vs artificial tears for the treatment of episcleritis. Eye (Lond). 2005;19(7):739-742. doi: 10.1038/sj.eye.6701632
[8] Diaz JD, Sobol EK, Gritz DC. Treatment and management of scleral disorders. Surv Ophthalmol. Epub June 15, 2016.
[9] Galor A, Thorne JE. Scleritis and peripheral ulcerative keratitis. Rheum Dis Clin North Am. 2007;33(4):835- 854.
[10] Dunlop AL, Wells JR. Approach to red eye for primary care practitioners. Prim Care. 2015;42(3):267-284. doi: 10.1159/000236038
[11] Upadhyay MP, Karmacharya PC, Koirala S, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol 2001; 85:388.
[12] Pihos AM. Epidemic keratoconjunctivitis: a review of current concepts in management. J Optom. 2013;6(2):69-74. doi: 10.1016/j.optom.2012.08.003
[13] Adam RS, Vale N, Bona MD, Hasanee K, Farrokhyar F. Triaging herpes zoster ophthalmicus patients in the emergency department: do all patients require referral? Acad Emerg Med. 2010;17(11):1183-1188. doi: 10.1111/j.1553-2712.2010.00875
Further Reading
- Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician by Gilani et al (West J Emerg Med. 2017;18(3)509-517)
- UpToDate Overview of the Red Eye
- Rosen’s or Tintinalli’s review chapters of the red eye
- Friedman, FD. Red Eye. In: Schaider J, Barkin R, Hayden S, Wolfe R, Barkin A, Shayne P, Rosen P. Rosen and Barkin’s 5-Minute Emergency Medicine Consult. 5th Edition. Philadelphia, PA: Wolters Kluwer; 2015; 956-957.