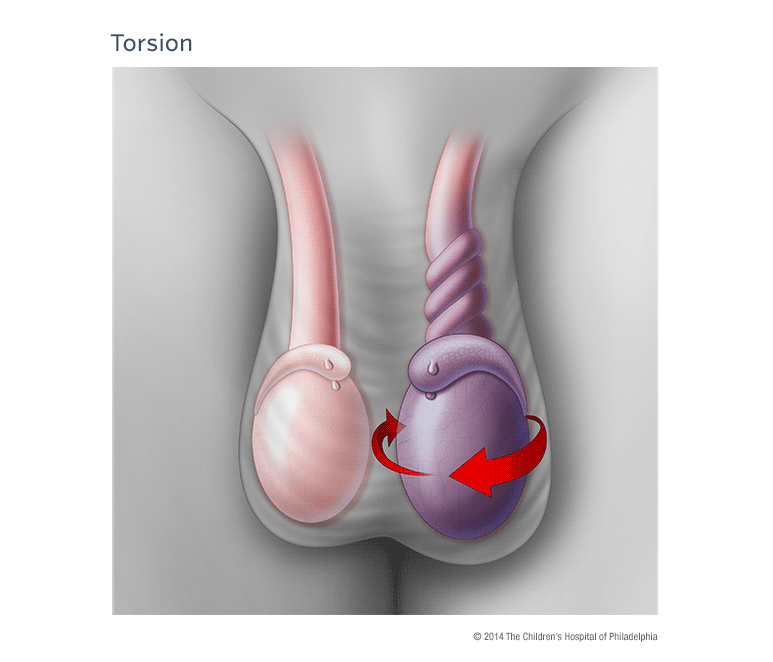
Definition: Twisting of the spermatic cord leading to decreased blood flow to the testicle resulting in ischemia, infarction and potentially, tissue necrosis.
Epidemiology:
- Most common cause of acute scrotal pain in prepubertal boys
- Torsion present in 3.2% of all children presenting to the ED with scrotal pain (Ben-Israel 2010)
- Bimodal frequency: peaks in 1st year of life and again at puberty
- Risk factors: History of cryptorchidism, horizontal testicular lie, increased spermatic cord length
- Anatomical defect in the tunica vaginalis allowing the testicle to rotate when the cremasteric muscle contracts
- Twisting of the testicle initially causes compromised venous return and can lead to arterial obstruction, ischemia and tissue necrosis
- Testicle can rotate from 180o to 720o
- Longer duration of torsion increases the risk of tissue necrosis
- Torsion recognized within 6 hours has an 80-100% salvage rate
- Persistent symptoms > 24 hours has a nearly 0% salvage rate
Differential Diagnosis
- Hydrocele
- Epididymitis
- Epididymorchitis
- Trauma
- Inguinal hernia
- Testicular tumor
Clinical Presentation
“No discriminating features, in either history or examination conclusively differentiate the correct diagnosis”(Sidler 1997)
History
- Sudden onset of scrotal pain
- Up to 20% of patients will have abdominal or flank pain alone (Mellick 2012)
- Nausea and vomiting
- History of blunt trauma (~ 10% of patients)
- History of similar pain in the past
- Presentation is often delayed (mean time to presentation 9.5 hours) (Rosen’s)
- Duration of symptoms should NOT guide management
- Historically, believed that symptoms > 24 hours inconsistent with salvageable tissue
- However, testicle may torse + detorse making it difficult to know how long ischemia present
Physical Examination
- Unilateral tender, firm testicle
- Scrotal erythema, edema and swelling
- Affected testicle typically higher than the unaffected one. OR = 58.8 (Ben-Israel 2010)
- Loss of cremasteric reflex
- Previously thought to be 100% sensitive and highly specific
- 30% of males with normal testicles will have an absent cremasteric reflex
- Studies report varying sensitivities as low as 60% (Mellick 2012)
- Horizontal (instead of vertical) testicular lie
Diagnosis
- The diagnosis of testicular torsion should be pursued in any patient with acute scrotal pain. Physical exam, history and imaging all have significant limitations.
- In patients with a high suspicion for torsion, emergent surgical consultation should not be delayed by diagnostic imaging as “time is testicle”
- Scrotal Ultrasound
- Standard imaging technique
- Diagnostic characteristics
- Sensitivity: 88 – 100% (+ Lr = 8.8 – 10)
- Specificity: 90%
- (+) LR = 8.8-10, (-) LR = 0.13
- Findings
- A torsed testicle will be hypoechoic, heterogeneous and enlarged
- Color doppler will demonstrate decreased or absent blood flow
- A partially-torsed testicle may have arterial flow but no venous flow, or may show an abnormal high-resistance pattern of arterial flow
- A testicle that has recently de-torsed will appear enlarged and hyperemic
- Due to the relatively low sensitivity, a negative color doppler ultrasound does not always rule out the disease
- Examination of the spermatic cord for twisting increases the false negative rate improving the utility of ultrasound to rule out the diagnosis
Ultrasound Images of Torsion
Management:
- ALL patients with suspicion for testicular torsion should have immediate consultation with a urologist for potential operative exploration and repair.
- Establish IV access and provide analgesia
- Manual detorsion
- Can be attempted if urology consultation is not immediately available
- May be successful in 25-80% of testicular torsion cases (Rosen’s 2014)
- Procedure
- Place patient supine
- Provider stands at the patients feet
- Apply “open book” rotation: rotate affected testicle away from midline
- Rotation required may be anywhere from 180o – 720o
- Up to 1/3 of patients will be torsed in the “opposite” direction (Mellick 2012)
-
- Regardless of the success of manual detorsion, all patients will require surgical evaluation
Take Home Points
- Consider the diagnosis of testicular torsion in all patients with acute testicular pain
- Testicular torsion is a surgical emergency that requires immediate urologic consultation to increase the rate of tissue salvage.
- History, physical examination and ultrasound are all flawed in making the diagnosis. The gold standard is surgical exploration
- Consider manual detorsion in patients where consultation will be delayed
References
Ben-Israel T et al. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med 2010; 28:786-789. PMID: 20837255
Sidler D et al. A 25-year review of the acute scrotum in children. S Afr Med J. 1997;87(12) 1696-8. PMID: 9497837
Mellick LB. Torsion of the testicle: It is time to stopping tossing the dice. Pediatric Emer Care 2012; 28: 80-6. PMID: 22217895
Ban KM, Easter JS: Selected Urologic Problems; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 99: p 1326-1356.