Background: Laceration repair is a common procedure in the Emergency Department (ED). The techniques of wound management and closure are well-covered as a part of any EM rotation, but this often focuses on the technical aspects of irrigation and closure. When it comes to suture selection, this is the scene frequently encountered:

Bellevue Suture Supplies
This post will provide an overview of the most common types of sutures available in the ED as well as some suggestions for how to select the correct material for a given repair.
Terminology
- Suture material
- Absorbable (e.g. Vicryl (polygalactin 910), chromic gut)
- Degraded in tissue in less than 60 days
- Traditionally used for closure of subcutaneous tissues or injuries to the tongue or nailbed
- Non-absorbable (e.g. Ethilon (nylon), silk, Prolene (polypropylene)
- Lasts longer than 60 days
- Traditionally used for skin closure
- Monofilament (e.g. Prolene (polypropylene), plain gut)
- Made of one strand of material
- Multifilament (e.g. Vicryl Rapide (polygalactin 910), silk)
- Made of multiple strands woven together in a braid
- More friction when pulled through tissues, however this adds greater security to knots than monofilament
- Greater risk for inflammation and infection than monofilament (Masini 2011)
- Natural (e.g. silk, chromic gut)
- Made of organic materials
- Traditionally more inflammatory than synthetic materials
- Synthetic (e.g. Ethilon (nylon), Vicryl (polyglactin 910))
- Made of laboratory manufactured material
- Absorbable (e.g. Vicryl (polygalactin 910), chromic gut)
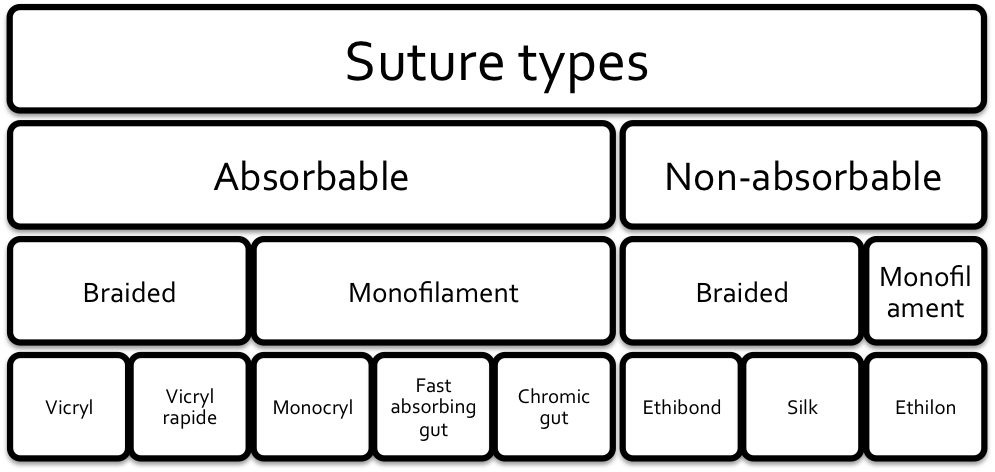
Suture Types (CanadiEM)
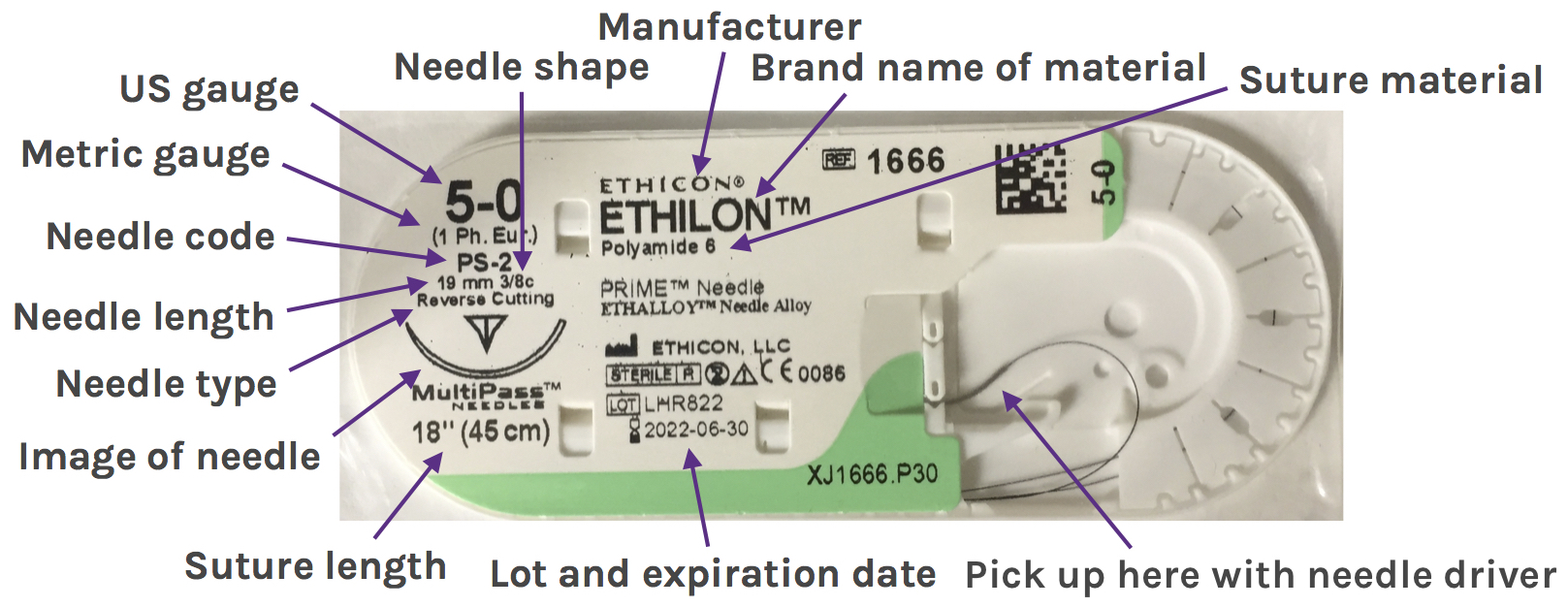
- Gauge: Size of suture
- Strength of suture proportional to square of the diameter of the thread
- Usually best to select smallest suture that provides adequate tensile strength as more material increases tissue reaction
- Standardized by United States Pharmacopedia
- Scale runs from 11-0 (smallest) to 7 (largest)
- Sizes are a number or a zero
- #2>#1>0>2-0 (00)
- Zero sizes are pronounced with the number of zeros first
- Eg. 7-0 is pronounced “seven-oh”
- Metric system used in other parts of the world
- Sized in tenths of a millimeter
- Eg. 5-0 is 0.1mm in diameter and size 1 metric
- Needles
- Size
- Measured from thread attachment to needle tip in mm
- Usually sized to correspond with suture gauge
- Shape
- eg. Straight, sections of a circle, double curved
- 3/8ths and 1/2 circle are most common for skin closure
- Types
- Cutting and reverse cutting most common for skin closure
- Cutting: sharp edge of needle on inside of curve
- Reverse cutting
- Sharp edge of needle on outside of curve
- Theoretically reduces chances of suture pulling through tissue
- Taper point: used for surgical applications in soft tissue
- Size
Needle types (From Ethicon Catalog)
Understanding Suture Packaging
Suture Description
Suture Examples
Commonly Used Suture Types in ED
- Both brand and generic names are used, which can be confusing
- Most common manufacturer in the US is Ethicon. Their brands are discussed in this post, but the same principles should apply to other brands
| Brand Name | Material | Strength Retention | Full Absorption | Applications | ||
|---|---|---|---|---|---|---|
| Absorbable | Multifilament | Vicryl | Polygalactin 910 | 50% at 21d | 56-70d | Subcutaneous closure, oral surgery |
| Vicryl Plus | Polygalactin 910 treated with antimicrobial | 50% at 21d | 56-70d | Subcutaneous closure, oral surgery | ||
| Vicryl Rapide | Polygalactin 910 gamma irradiated to speed absorption | 50% at 5d | 42d | Tongue lacerations, oral injuries, skin closure on trunk and extremities | ||
| Monofilament | Plain Gut | Beef serosa or sheep submucosa | 7-10d | 70d | Suturing fatty tissues, oral repairs, nailbed repairs | |
| Fast Absorbing Gut | Beef serosa or sheep submucosa heat treated to speed absorption | ~7d | 21-42d | Skin closure on the face | ||
| Chromic Gut | Beef serosa or sheep submucosa treated with chromium to slow absorption and tissue reaction | 21-28d | 90d | Tongue lacerations, nailbed repair, subcutaneous closure | ||
| Non-absorbable | Multifilament | Ethibond | Polyester/Dacron | Indefinite | N/A | Tendon repair |
| Perma-hand Silk | Silk | Gradual loss over time | N/A | Securing drains, lines, and tubes | ||
| Monofilament | Ethilon | Nylon 6 | Gradual loss over time | N/A | Most common material for skin closure | |
| Prolene | Polypropylene | Indefinite | N/A | Alternative choice for skin closure | ||
(Data in table from Ethicon Website)
Selecting the Right Material
- Limited data to guide decision
- Most choices based on physician preference, experience, and local standard practice
- General Guidelines
- Careful evaluation of the wound is essential to assess for wound tension and whether deep layer closure will be required
- Wound tension is the amount of perpendicular force that must be applied to a wound to approximate the edges
- Higher tension = more force
- Wounds under higher tension require a larger gauge suture that will tolerate a greater amount of force
- Deep layer closure and other advanced repair techniques can be used to reduce wound tension
- Lower tension repairs are ideal as they result in a better cosmetic outcome
- Anatomic region tends to determine amount of tension on a wound
- Facial wounds are often lower tension than wounds on trunk or extremities
- Within these areas, there are regions of higher tension, like the chin or flexor surfaces which may require different material
- Nonabsorbable monofilament commonly used for skin closure
- Nylon (Ethilon) tends to be favored over polypropylene (Prolene) for its lower cost and its slightly easier handling
- Polypropylene (Prolene) may be favored in infected or inflamed tissues (Lammers 2014)
- Prolene is often colored blue, so may be chosen in areas with hair to help identify sutures for removal
- Absorbable materials
- Reasons to select
- Suture will not be accessible for later removal
- Oral injuries
- Suture removal may be difficult (i.e. pediatric patients, patients with poor follow-up)
- Polygalactin 910 (Vicryl)
- Useful in deep layer closures
- Provides long-term tensile strength and mid range absorption time (50% at 21d), minimizing tissue reaction (Lammers 2014)
- Chromic gut
- Plain gut treated with chromic salts to slow absorption (50% at 21-28d) and minimize tissue reaction
- Useful in oral repairs, nailbed laceration repair (Lammers 2014, Brown 2007)
- Fast absorbing gut
- Heat treated plain gut for more rapid absorption (50% at ~7d)
- Growing trend towards use in repair of facial lacerations in pediatric patients or patients with poor follow-up
- Available literature suggests noninferiority to nonabsorbable materials in cosmeses and patient satisfaction (Xu 2016)
- Gamma irradiated Polygalactin 910 (Vicryl Rapide)
- Preferred by some oral surgeons for mucosal and dental injuries as may lead to more rapid healing over chromic gut (Gazivoda 2015)
- Increasingly popular in repair of lacerations on the torso and extremities in patients whom suture removal may be difficult
- Available data suggests noninferiority to polypropylene (Prolene) in cosmetic outcome with a nonsignificant greater incidence of infection with absorbable material (Tejani 2014)
- Reasons to select
- Careful evaluation of the wound is essential to assess for wound tension and whether deep layer closure will be required
Specific Recommendations Based on Anatomic Region
- Generalized recommendations from Brian Lin of Closing the Gap of what material to start with in a particular region with a particular amount of tension
| Anatomic Region | High Tension | Low Tension | Without Removal | Deep Layer |
|---|---|---|---|---|
| Face | 5-0 nylon (Ethilon) | 6-0 nylon (Ethilon) | 6-0 fast absorbing gut | 5-0 polygalactin 910 (Vicryl) |
| Extremities/Trunk | 4-0 nylon (Ethilon) | 5-0 nylon (Ethilon) | 4-0 and 5-0 gamma irradiated polygalactin 910 (Vicryl Rapide) | 4-0 polygalactin 910 (Vicryl) |
| Tongue Lacerations | 3-0 chromic gut | 4-0 chromic gut | N/A | N/A |
| Nailbed Lacerations | 4-0 and 5-0 chromic gut | 6-0 chromic gut | N/A | N/A |
| Hair-Bearing Areas | 4-0 and 5-0 colored polypropylene (Prolene) | 5-0 and 6-0 colored polypropylene (Prolene) | See above | See above |
Take Home Points
- An understanding of the properties of a given suture material helps guide rational selection for a particular application
- All materials have advantages and disadvantages. Selection must be guided by careful evaluation of any wound prior to repair
- “The best suture for a given laceration is the smallest diameter suture, which will adequately counteract static and dynamic tension forces on the skin.” – Brian Lin
- Consider using absorbable materials for epidermal closure in patients where suture removal may be difficult
Read More
CanadiEM: Nice Threads: a Guide to Suture Choice in the ED
Closing the Gap: Stock and Simplify Your Suture Cart Part 1
ALiEM: PV Card: Laceration Repair and Sutures
Ethicon: Wound Closure Overview
References
Masini BD et al. Bacterial adherence to suture materials. J Surg Educ. 2011;68(2):101-4. PMID: 21338964
Lammers RL, Smith ZE. Methods of Wound Closure. Robers and Hedges’ Clinical Procedures in Emergency Medicine, Chapter 35, 644-689.e2. Saunders; 2014.
Brown DJ, Jaffe JE, Henson JK. Advanced laceration management. Emerg Med Clin North Am. 2007;25(1):83-99. PMID: 17400074
Xu B et al. Absorbable Versus Nonabsorbable Sutures for Skin Closure: A Meta-analysis of Randomized Controlled Trials. Ann Plast Surg. 2016;76(5):598-606. PMID: 25643187
Gazivoda D, Pelemiš D, Vujašković G. A clinical study on the influence of suturing material on oral wound healing. Vojnosanit Pregl. 2015;72(9):765-9. PMID: 26554107
Tejani C et al. A comparison of cosmetic outcomes of lacerations on the extremities and trunk using absorbable versus nonabsorbable sutures. Acad Emerg Med. 2014;21(6):637-43. PMID: 25039547







Thank you very much