Definitions
- Sialolithiasis: presence of stones in a salivary gland and/or salivary duct.
- Sialadenitis: inflammation of a salivary gland which may result from obstruction or infection.
Epidemiology and Risk Factors
- Most cases occur between the ages of 30 and 60. Sialolithiasis is more common in men than women and rare in children, whereas sialadenitis affects both genders equally and can occur in newborns.
- Risk factors for sialolithiasis include dehydration, smoking, anticholinergic medications, diuretics, history of kidney stones, hypovolemia.
- Risk factors for sialadenitis include the above as well as immunocompromised status and malnutrition.
Pathogenesis
- Not clearly known, but currently thought that reduced salivary flow and salivary concentration of calcium are contributing factors.
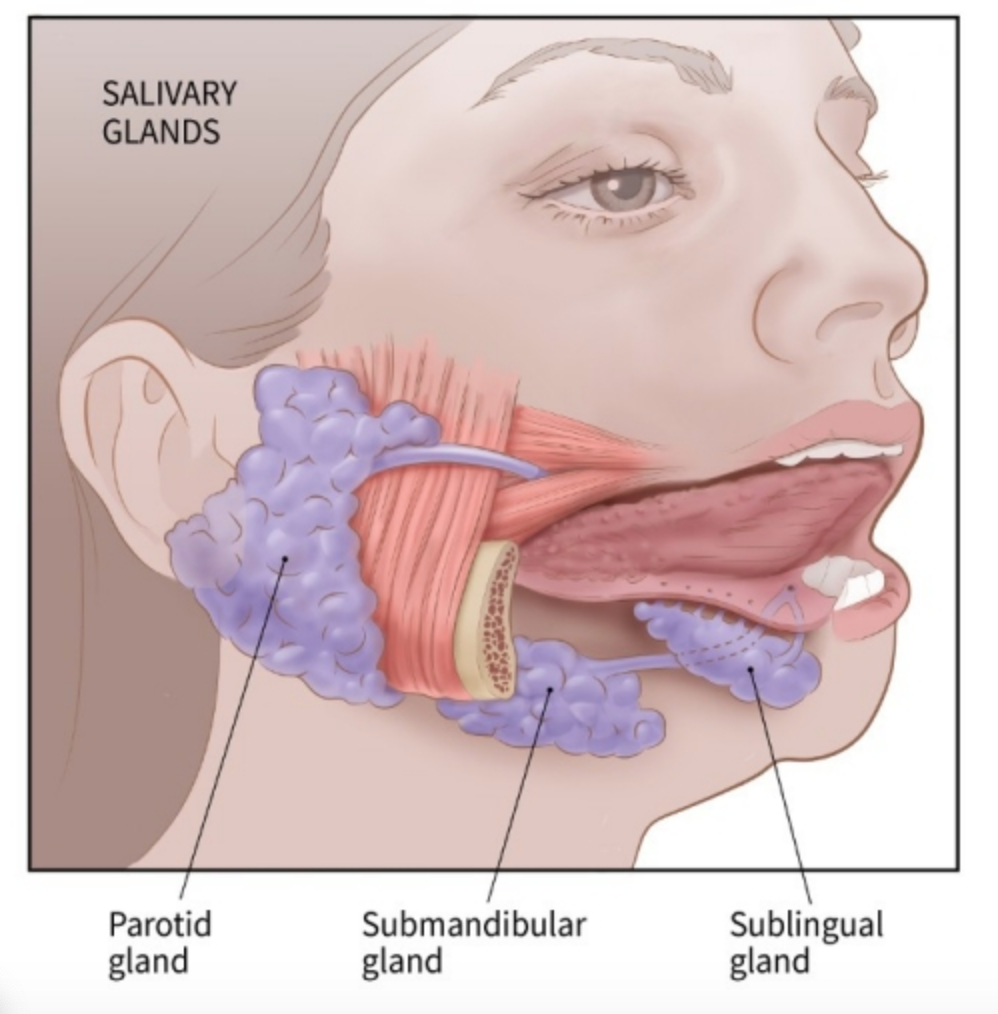
- Almost all (80-90%) stones occur in the submandibular glands, while 10-20% occur in the parotid glands. Sublingual stones can also occur, but are rare.
Clinical Findings
- Classically presents as both pain and swelling in affected area worsened by eating.
- May also present as painless swelling or as pain without swelling.
- Decreased saliva production.
- Xerostomia (dry mouth).
- If there is worsening pain, erythema, +/- fever, consider an infection.
Physical Exam
- Examine the symptomatic area for erythema, crepitus, induration, fluctuance, or swelling.
- Palpate the course of the symptomatic gland and associated duct from the posterior part and move anteriorly, feeling for a mass or tenderness.
- Ask the patient to elevate their tongue and massage the symptomatic gland; observe for expression of pus from the duct.
- Perform a thorough exam of all oral structures to ensure patent airway.
Differential Diagnosis
- Viral sialadenitis: glandular swelling and pain commonly preceded by viral prodrome (myalgias, headache, malaise, low-grade fever). May sometimes be bilateral. Mumps is most classically associated with sialadenitis, but other pathogens include parainfluenza, EBV, adenovirus, enterovirus, parvovirus, and HHV-6.
- Bacterial sialadenitis: most often involves parotid gland. Is often unilateral, and purulent drainage may be expressed. Pathogens include S. aureus (most common), S. pneumoniae, S. viridans, H. influenzae, Bacteroides.
- HIV: Pt’s can develop lymphoepithelial cysts in parotid gland—usually diffuse and symmetric.
- Ludwig’s Angina: bilateral diffuse cellulitis of the submandibular space that can lead to severe airway complications. Always examine underneath the tongue.
- Sjogren’s Syndrome: typically bilateral swelling and associated symptoms of dry eyes and mouth.
- Salivary gland tumor: often presents subacutely and unilaterally, as a firm, nontender mass.
Imaging
If diagnosis is unclear from history and physical exam, imaging may be pursued.
- Ultrasound: requires an experienced user, but is cheaper, faster, and effective in diagnosing stones. Recent data suggests that a transoral approach is superior to transcutaneous.
- CT: standard of care as it allows for better assessment of other findings such as abscesses, tumors, or strictures. Request fine cuts to make sure not to miss small stones.
Management
Stone without infection—conservative management:
- Adequate hydration, topical heat packs, massaging of gland, and sialagogues (sour candy/lemonade) to stimulate the gland.
- Treat underlying risk factors if possible (i.e. discontinue anticholinergic meds, smoking cessation, etc.).
If infection present, treat with antistaphylococcal antibiotics:
- Cephalexin or dicloxacillin 500mg QID for 7-10 days.
- If no improvement in pain, purulent drainage, or fever in 5 days, obtain culture and broaden coverage (Augmentin or clindamycin) until results obtained.
- Consider imaging (ultrasound and/or CT with contrast) and ENT consultation if concern for abscess.
Referral to ENT for:
- Failure of conservative management
- Complicated infection with abscess
- Recurrence of symptoms/chronic sialadenitis
- Finding of salivary gland tumor
Editor’s submandibular gland stones s/p manual removal (penny for scale):

References
- Williams MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32(5):819. PMID 10477789
- Huoh KC, Eisele DW. Etiologic factors in sialolithiasis. Otolaryngol Head Neck Surg. 2011;145(6):935. PMID: 21753035
- Burke CJ, Thomas RH, Howlett D. Imaging the major salivary glands. Br J Oral Maxillofac Surg. 2011;49(4):261. Epub 2010 Apr 9. PMID: 20381221
- Alyas F, Lewis K, Williams M, Moody AB, Wong KT, Ahuja AT, Howlett DC. Diseases of the submandibular gland as demonstrated using high resolution ultrasound. Br J Radiol. 2005;78(928):362. PMID: 15774602
- Schapher M, Goncalves M, Mantsopoulos K, Iro H, Koch M. Transoral Ultrasound in the Diagnosis of Obstructive Salivary Gland Pathologies. Ultrasound Med Biol. 2019 Sep;45(9):2338-2348. PMID: 31227261
- Koch M, Zenk J, Iro H. Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin North Am. 2009 Dec;42(6):1173-92. PMID: 19962014
- Yiu AJ, Kalejaiye A, Amdur RL, Todd Hesham HN, Bandyopadhyay BC. Association of serum electrolytes and smoking with salivary gland stone formation. Int J Oral Maxillofac Surg. 2016;45(6):764. Epub 2016 Mar 8. PMID: 26969301
- Davidkin I, et al. Etiology of mumps-like illnesses in children and adolescents vaccinated for measles, mumps, and rubella. J Infect Dis. 2005 Mar 1;191(5):719-23. Epub 2005 Jan 19. PMID: 15688285
- Diagram from: https://www.cancer.org/cancer/salivary-gland-cancer/about/what-is-salivary-gland-cancer.html
- Image: Micrograph of chronic sialadenitis, with a patchy lymphocytic infiltrate and fibrosis. From: https://commons.wikimedia.org/wiki/File:Chronic_sialadenitis.jpg