SCFE (http://www.chw.org/)
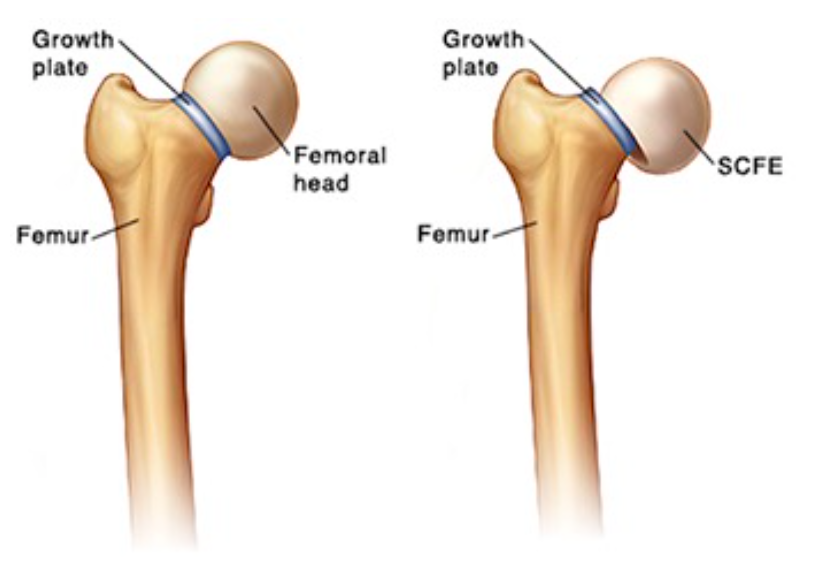
Definition: Slipped Capital Femoral Epiphysis (SCFE), also known as Slipped Upper Femoral Epiphysis (SUFE), is characterized by a displacement of the capital femoral epiphysis from the femoral neck through the physeal plate
Epidemiology
- Incidence: 1/1000 and 1/10,000 (Kelsey 1970).
- Mean age of presentation (Loder 1996)
- Girls: 12 yrs
- Boys: 13.5 yrs, respectively.
- More common in males, with a M:F ratio of about 1.5:1.
- Obesity is a significant risk factor
- Up to 60% of patients measure at or above the 90th percentile for weight and age (Loder 1993).
- SCFE can also be seen in tall, thin patients who have recently undergone a growth spurt, which results in shearing stress on the weak epiphysis (Kim 2006)
- Bilateral cases: 20 -40% of patients (Mick 2013).
- In children who present with unilateral disease, the contralateral hip eventually slips in 30- 60%.
- In patients with endocrine disorders, the contralateral hip slips in up to 100% of cases. (Loder 1993).
Mechanism
- Anatomy: The proximal femoral physis contributes to metaphyseal growth of the femoral neck and to appositional growth of the femoral head
- SCFE Development
- Shearing forces applied to the femoral head exceed the strength of the capital femoral physis.
- Results in anterior and superior displacement of the portion of the proximal femur that is distal to the growth plate. (Koop 1996)
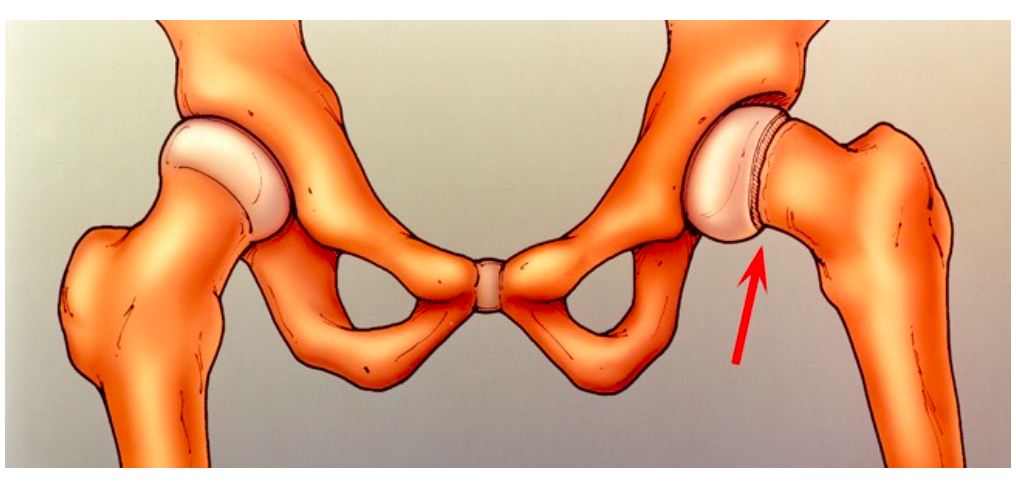
Anterior and superior displacement of proximal femur (orthoinfo.aaos.org)
- Factors that can contribute to weakening the growth plate include (Weiner 1996)
- Hormonal changes during puberty that lead to normal periosteal thinning/widening
- Trauma
- Obesity
- Inflammation
- Genetic predisposition
- Endocrine disorders
- Total body radiation
Clinical Presentation
- Most common features on presentation are pain and altered gait (Koop 1996).
- Assess for leg length discrepancy and any limitation in hip range of motion
- Hip may be held in external rotation
- Pain elicited by experiences pain with range of motion, especially abduction, flexion, and internal rotation (Kim 2006)
- Isolated thigh or knee pain (Matava 1999)
- Seen in 15% of cases
- Normal knee exam despite complaining of knee pain
- Gait Assessment
- May demonstrate Trendelenberg gait
- A waddling gait is seen in patients with bilaterally SCFE
- In severe cases, patient may be unable to bear weight and/or thigh and gluteal muscle atrophy may be present
- Passive flexion of the hip from extension may cause abduction and external rotation (highly suggestive of SCFE) (Kim 2006)
Classification Systems
- Three systems to classify SCFE
- Presentation patterns
- Preslip
- Pain without displacement
- X-Rays show widening of the proximal femoral growth plate compared to contralateral side
- Acute
- Symptoms for less than 3 weeks
- Effusion present
- Acute on chronic
- Symptoms for at least 3 weeks and present
- Acute worsening of symptoms including pain and decreased range of motion
- Joint effusion is present but unlike in acute cases, metaphyseal remodeling is present
- Chronic
- Intermittent symptoms for more than 3 weeks
- Metaphyseal remodeling is present but without a joint effusion.
- Preslip
- Stability
- Stable – patients are able to walk (+/- crutches)
- Unstable – patients are unable to bear weight, regardless of duration of symptoms.
- Severity
- Associated with prognosis
- Mild – displacement is less than 1/3 the diameter of the femoral neck
- Moderate – displacement is greater than 1/3 but less than ½ the diameter
- Severe – displacement is greater than ½ the diameter of the femoral neck
SCFE Severity Classification

Normal Hip Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8004

SCFE Pre-Slip Case (courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8004)

SCFE Mild Slip (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8004)

SCFE Moderate Slip (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8004)
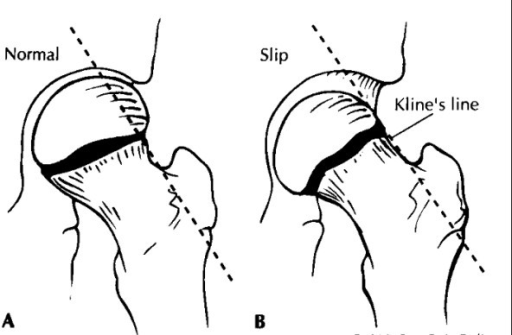
Klein’s Line (openi.nlm.nih.gov)
X-Ray Findings
- Required views
- Anterior-posterior (AP) and lateral hips
- Image both hips given incidence of bilateral involvement
- AP View
- Klein’s Line
- A line drawn along the superior aspect of the femoral neck that intersects with the femoral head in normal hips
- Suspect slippage (SCFE) if the line passes superiorly
- SCFE findings
- Widening of the femoral head physis
- Irregularity of the growth plate
- Slippage of the epiphysis “ice cream falling off of the cone”
- Klein’s Line
- Normal Hip AP X-ray (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 2715)
- SCFE AP X-ray (Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 7228)
- Lateral View
- Posterior displacement and step-off of the epiphysis on the femoral neck are better demonstrated on the lateral view
- The cross-table view is recommended in patients who have acute onset of symptoms, to prevent further displacement in patients with unstable slips
- SCFE Lateral Hip X-ray (Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 7228)
ED Management
- Provide analgesia
- Definitive treatment is operative and involves the stabilization of the diseased physis via percutaneous pinning
- All patients diagnosed with SCFE should be strictly non-weightbearing
- Disposition
- Refer to orthopedic surgeon for planned surgical correction, usually within 24-48hrs
- Consider admission to hospital, especially in acute or bilateral cases (Mick 2013)
- Atypical Presentations
- Should be considered in
- Children < 10 years of age or > 16 years of age
- Weight < 50th percentile for age
- Height < 10th percentile for age
- Diagnostic consideration: renal failure, history of radiation therapy, endocrine/metabolic disorders (Loder 2001)
- Workup: BMP, TSH, Urine studies (Wells 1993)
- Should be considered in
Prognosis
- Complications of SCFE include avascular necrosis of the femoral head, which is more common in acute and unstable slips
- Patients are also at slight risk for gait disturbances and leg-length discrepancies
- In patients without complications, osteoarthritis of the hip usually develops over a course of decades
- In instances of unilateral SCFE most contralateral cases occur within the first 2 years after the initial slip (Mick 2013)
- Prophylactic pinning is controversial and if this is not performed, patients with unilateral SCFE should be followed closely by an orthopedic surgeon
Take Home Points
- Image bilaterally as SCFE is often bilateral even in the absence of bilateral symptoms
- Patients may present with isolated knee or thigh pain without any hip pain, which can lead to delayed diagnosis and worse outcomes
- More than 50% of SCFEs can be missed when the chief complaint is knee pain. Always range the hip and note the presence or absence of pain in patients presenting with knee pain
- SCFE is usually seen in adolescent, obese patients. However, it can also be seen in tall, thin patients who have recently undergone a recent growth spurt
Read More
Radiopaedia: Slipped Upper Femoral Epiphysis
Davenport M et al. An Evidence –Based Approach to Pediatric Orthopedic Emergencies. Pediatric Emergency Medicine Practice. 2009;6(5). EB Medicine
References
Kelsey JL et al. The incidence and distrubition of slipped capital femoral epiphysis in Connecticut and Southwestern United States. J Bone Joint Surg Am. 1970;52(6):1203. PMID 5460281
Loder RT. The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop Relat Res 1996; 322: 8-27. PMID 8542716
Kim TY et al. Limping: Evaluation, Diagnosis, and Management in the Pediatric ED. Pediatric Emergency Medicine Practice. 2006;3(8). EB Medicine
Mick NW, Valasek AE. Pediatric orthopedic emergencies. in Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge University Press 2013: 165-177. DOI: 10.1017/CBO9781139199001.008
Loder RT et al. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993; 75(8): 1141-7. PMID 8354672
Egol KA et al. Handbook of Fractures 5th edition. Philadelphia, PA. Wolters Kluwer. 2015. pp. 662-669. ISBN-13: 978-1451193626
Koop S et al. Three common causes of childhood hip pain. Pediatr Clin North Am. 1996;43(5):1053. PMID 8858073
Weiner D. Pathogenesis of slipped capital femoral epiphysis: current concepts. J Pediatr Orthop B. 1996;5(2):67. PMID 8811532
Matava MJ et al. Knee pain as the initial symptom of slipped capital femoral epiphysis: an analysis of initial presentation and treatment. J Pediatr Orthop. 1999;19(4):455. PMID 10412993
Loder RT et al. Clinical characteristics of children with atypical and idiopathic slipped capital femoral epiphysis: description of the age-weight test and implications for further diagnostic investigation. J Pediatr Orthop. 2001;21(4):481. PMID 11433161
Wells D et al. Review of slipped capital femoral epiphysis associated with endocrine disease. J Pediatr Orthop. 1993;13(5):610. PMID 8376562



Thanks designed for sharing such a nice opinion, paragraph is nice, thats why i have read it entirely