Definition: Salicylate toxicity is characterized by a constellation of symptoms caused by acute or chronic overdose of salicylate containing compounds. The most common salicylate is aspirin, but the group also includes topical forms of salicylates, methyl salicylate (Oil of Wintergreen), and bismuth subsalicylate (such as in Pepto-Bismol).

Aspirin Metabolism (Goldfrank’s Toxicology)
Pathophysiology of Salicylate Toxicity
- Basics
- Aspirin is rapidly converted to salicylic acid.
- The therapeutic range of salicylate concentration for anti-inflammatory effects is between 15 and 30 mg/dL.
- Concentrations higher than 30mg/dL can be associated with signs and symptoms of toxicity.
- Detailed Pathophysiology
- Salicylic acid acts to uncouple oxidative phosphorylation, leading to accumulation of lactic acid and pyruvic acid, causing a primary elevated anion gap metabolic acidosis.
- Salicylic acid also directly stimulates the respiratory drive in the medulla, leading to a primary respiratory alkalosis.
- Salicylic acid is a weak acid: exists mostly in charged/ionized state at physiologic pH. As pH decreases, shifts more towards uncharged/ non-ionzed state and can cross blood-brain barrier to worsen neurotoxicity.
- Neuroglycopenia (Thurston 1970)
- Even at normal plasma glucose levels, salicylate toxicity causes decreased brain glucose due to uncoupling ofoxidative phosphorylation and compensatory stimulation of brain glycolysis.
- This can cause CNS effects of hypoglycemia at normal plasma glucose levels.
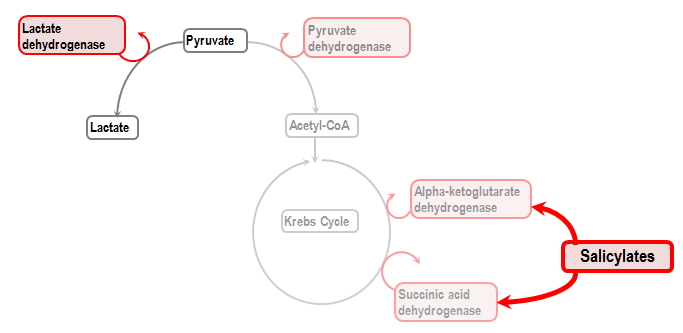
Salicylate Effect on Oxidative Phosphorylation (www.derangedphysiology.com)
Clinical Presentation
- Tachypnea and hyperpnea: due to central stimulation of respiratory drive
- Tinnitus: not completely understood mechanism, inhibition of COX and Na/K ATPase in ear. In the elderly, may see decreased hearing instead of tinnitus
- Nausea/vomiting: disruption of mucosal barrier, local gastric irritation
- CNS: uncoupling of neuronal oxidative phosphorylation and neuroglycopenia lead to confusion, altered mental status, seizures, coma
- Hyperthermia, due to uncoupling of oxidative phosphorylation (this may represent a peri-mortem presentation)
Acute Toxicity
- Often present with known / intentional ingestion
- Often younger patients without medical problems
- Co-ingestants are common
Chronic Toxicity
- Often unintentional and not initially obvious overdose, older patients, salicylate usually used for chronic medical problem
- Increased mortality, likely due to delay in diagnosis and underlying medical comorbidities
Differential Diagnosis
- Anion gap metabolic acidosis (AGMA)
- KULTS
- Ketoacidosis (DKA, alcoholic ketoacidosis)
- Uremia
- Lactic acidosis
- Toxins (ethylene glycol, methanol, metformin)
- Salicylates
- Consider the diagnosis in any elderly patient with altered mental status that is taking aspirin. Chronic salicylate toxicity is often confused with a simple UTI leading to delayed diagnosis
Diagnostics
- Blood Gas (VBG or ABG)
- Classical finding: primary metabolic acidosis with primary respiratory alkalosis
- Winter’s Formula: In patient with primary metabolic acidosis, you must determine if decrease in CO2 is a compensation, or if there is another primary acid/base disturbance
- Patients will often present with normal pH to slightly alkalemic
- Patients who are acidemic on presentation are more likely to be critically ill
- BMP
- Look for elevated anion gap metabolic acidosis
- However, salicylate can interfere with lab assay for chloride, causing falsely elevated chloride and making it appear as though anion gap is normal
- Acute kidney injury
- Hypokalemia secondary to acidemia
- Salicylate concentration: can give you an indication of how severe toxicity is and influence management considerations
- Acetaminophen level (concomitant acetaminophen ingestion common in all overdoses)
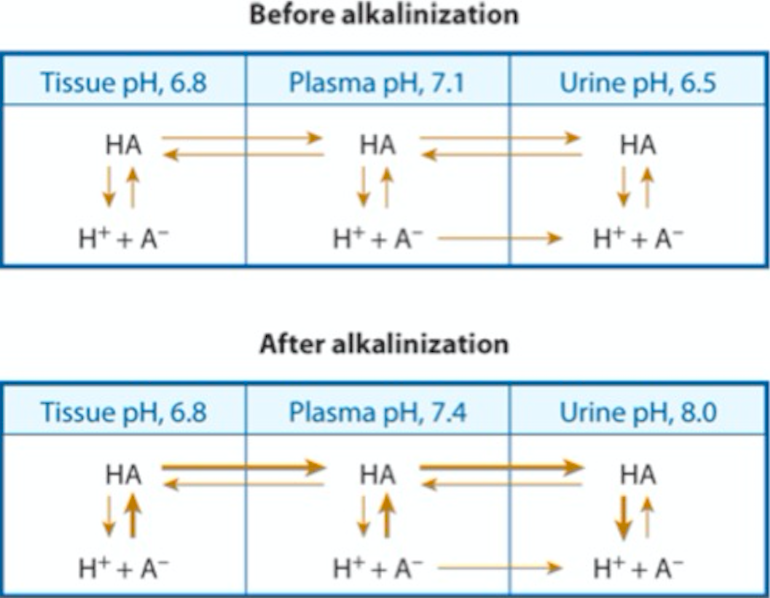
Alkalinization (Goldfrank’s Toxicology)
Management
- Initial Management
- Basics: ABC’s, IV, O2 (if hypoxic), cardiac monitor
- GI decontamination: activated charcoal if patient awake and alert to tolerate
- Alkalinization with Sodium Bicarbonate
- Goal in treatment is to increase pH of both serum and urine to shift towards charged state to prevent neurotoxicity and enhance elimination through the urine. (Goldfrank 2015)
- Start with a bolus of 1-2 mEq/kg followed by a drip
- “1 amp” of bicarbonate is equal to 50mL of 8.4% sodium bicarbonate 1mEq/mL, or 50mEq of NaHCO3–
- Bicarb drip can be made with 3 ampules of NaHCO3– (150 mEq) in one liter of D5W
- Do not make bicarb drip with normal saline because this will be hypertonic solution due to sodium in sodium bicarbonate
- Run bicarb drip at 1.5-2X maintenance fluid rate. These patients are fluid down and need to replace losses
- Goal serum pH around 7.55, urine pH 8.0
- No benefit of forced diuresis
- Treat hypo or normoglycemia to prevent neuroglycopenia (Thurston 1970, Kuzak 2007)
- No human studies showing a “goal” serum glucose concentration
- If patient is altered, consider glucose supplementation regardless of serum glucose concentration
- Treat hypokalemia to goal K of 5.5 mEq
- If hypokalemia, renal tubules will reabsorb potassium ions in exchange for hydrogen ions
- This prevents alkalinization of the urine
- Airway and Respiratory Management (Mosier 2015)
- Tachypnea alone is not an indication for intubation
- Tachypnea and hyperpernea leads to respiratory alkalosis
- This is necessary compensation for the metabolic acidosis
- Avoid intubation if possible
- Hypoventilation during the apneic period causes respiratory acidosis
- Associated with peri-intubation period morbidity and possible cardiac arrest (Stolbach 2008)
- Indications for airway management include hypoxia, pulmonary edema, hypoventilation/tiring out, worsening acidosis despite appropriate therapy
- Give bicarb 1-2 mEq/kg bolus peri-intubation
- Consider awake intubation or ketamine facilitated intubation to minimize or eliminate apneic time
- Ventilator settings very important post-intubation
- Need to match minute ventilation of patient pre-intubation to prevent respiratory acidosis
- High tidal volumes and high rate needed
- Frequent blood gas monitoring post-intubation, as well as need for frequent BMP, salicylate concentrations. Consider A-line placement
- Tachypnea alone is not an indication for intubation
- Hemodialysis (HD) (McCabe 2017)
- If unable to appropriately alkalinize and eliminate salicylate with bicarbonate, HD may be indicated
- Consult nephrology early to be able to ensure prompt HD
- Indications include: persistent altered mental status, renal/hepatic/cardiac failure, persistent acidemia, and requiring intubation
- No definite cutoff for salicylate concentration requiring HD, however acute toxicity patients with concentrations greater than 80 or 100 mg/dL will likely require HD
- In chronic salicylate toxicity, may require HD at much lower levels
Take Home Points:
- Always consider salicylate toxicity
- In patients with tachypnea, hyperpnea, AMS and clear lungs
- In the presence of an anion gap metabolic acidosis with a respiratory alkalosis
- Treat salicylate toxicity by alkalinizing the blood and urine to increase excretion
- Avoid intubation until absolutely necessary. If you do have to intubate, minimize apneic time and consider awake intubation and nake sure your ventilator settings match the patient’s necessary high minute ventilation
- Think about chronic salicylate toxicity in unexplained altered mental status, tachypnea or metabolic acidosis in elderly
- Know indications for hemodialysis in salicylate toxic patients
Read More:
- LITFL: Salicylates
- Wiki EM: Salicylate Toxicity
- Rebel EM: Acute Salicylate Toxicity, Mechanical Ventilation, and Hemodialysis
- Boyer, EW. Weilbrecht, KW. Salicylate (aspirin) poisoning in adults. UpToDate. Mar 2018. Link
References:
- Anderson, RJ et al. Unrecognized adult salicylate intoxication. Ann Intern Med 1976; 85: 745-748. PMID 999110
- Goldberg, MA. Barlow, CF. Roth, LJ. The Effects of Carbon Dioxide on the Entry and Accumulation of Drugs in the Central Nervous System. J Pharmacol Exp Ther. (1961) 131: 308-318. PMID 13706469
- Hoffman, RS. Howland, MA. Lewin, NA.. Nelson, LS. Goldfrank LR. Goldfranks’s Toxicologic Emergencies (10th ed.) New York: McGraw-Hill Education. 516-527.
- Kuzak N. Brubacher JR. Kennedy JR. Reversal of saliycate –induced euglycemic delirium with dextrose. Clinical Toxicology. 45:5; 526-529. PMID 17503260
- McCabe, D et al. The association of hemodialysis and survival in intubated salicylate-poisoned patients. Am J Emerg Med 2017; 35: 899-903. PMID 28438446
- Temple AR. Acute and Chronic Effects of Aspirin Toxicity and Their Treatment. Arch Intern Med 1981; 141: 364-369. PMID 7469627
- Thurston JH et al. Reduced brain glucose with normal plasma glucose in salicylate poisoning. J Clin Invest. 1970: 49 (11); 2139-45. PMID 4319971
- Stolbach, AI. Hoffman, RS. Nelson, LS. Mechanical Ventilation Was Associated with Acidemia in a Case Series of Salicylate-poisoned Patients. Soc Acad Emerg Med 2008; 866-869. PMID 18821862
- Mosier JM et al. The physiologically difficult airway. West J Emerg Med 2015; 16(7): 1109-17. PMID: 26759664

Question: Can these descriptions be applicable for salicylate sensitive individuals when they ingest salicylate food, drinks, or medications, or topically apply salicylate ingredients?
Great article! Thanks for really breaking ASA poisoning down. As a paramedic and educator I especially appreciate the mention of avoiding intubation if possible to avoid taking away their compensatory response. This is what I teach my students and a point that has been lost on a number of providers throughout my career.
One question. Since salicylates are mostly protein bound, what about the use of IV Lipid Emulsion Therapy as a treatment for severe toxicity?