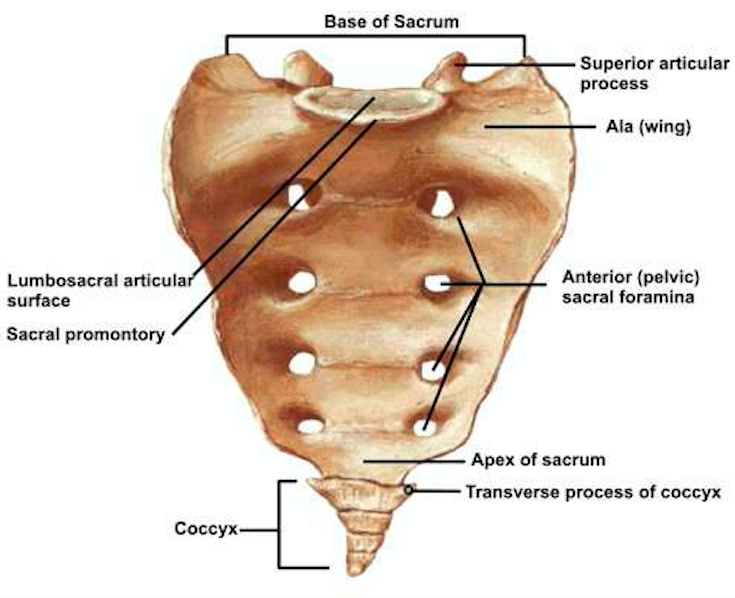
Sacrum Anatomy (orthbullets.com)
Definition: A fracture involving the sacrum, a structure located at the base of the lumbar spine formed by the fusion of five sacral vertebrae.
Mechanism
- In younger adults, the mechanism is typically a high-energy trauma
- In the elderly, the mechanism can be the result of low energy falls
Epidemiology
- The incidence follows the distribution as listed above: high-energy trauma (MVA, pedestrian struck, fall from height, motorcycle accident, crush injury) or low-energy trauma in patients with osteoporosis or cancer.
- Sacral fractures are relatively rare
- ~ 5% occurring as isolated injuries
- Up to 45% occurring with concomitant pelvic ring injury (Rodrigues-Pinto 2017)

Sacral Nerve Roots (McGraw-Hill)
Physical Exam
- Inspect the skin for any signs of soft tissue trauma around the pelvis
- Assess for pelvic ring stability by internally and externally rotating the iliac wings (pelvic bone manipulation should only be performed in hemodynamically stable patients as manipulation can dislodge clots causing worsening bleeding)
- Palpate over the lumbosacral region for subcutaneous fluid mass
- Suggests a closed fascial degloving injury (Morel-Lavallee lesion) that is later prone to infection or extensive skin necrosis
- Vaginal exam in women to rule out through-and-through injury
- Perform a complete neurologic exam
- Up to 25% have an associated neurologic injury
- S1-S4 nerve roots run through the sacral foramina with S1 and S2 carrying a higher rate of injury
- Rectal exam: rectal tone, perianal wink
- Sensation to light touch and pinprick along S2-S5
- Bulbocavernosus and cremasteric reflexes
- Full lower extremity sensory and motor exam to rule out cauda equina syndrome
- Vascular exam: check distal pulses and ankle-brachial indexes given close proximity of sacrum with iliac vessels
Classification
- Denis Classification
- Zone 1: Fracture lateral to foramina.
- Most common (50%)
- Rare nerve root injury to L5 (5%)
- Zone 2: Fractures through the foramina.
- Can be stable or unstable
- More likely unstable if there is a shear component.
- Zone 3: Fractures medial to foramina into spinal canal
- Highest rate of neurologic deficit (60%)
- Bladder/bowel/sexual dysfunction common
- Zone 1: Fracture lateral to foramina.
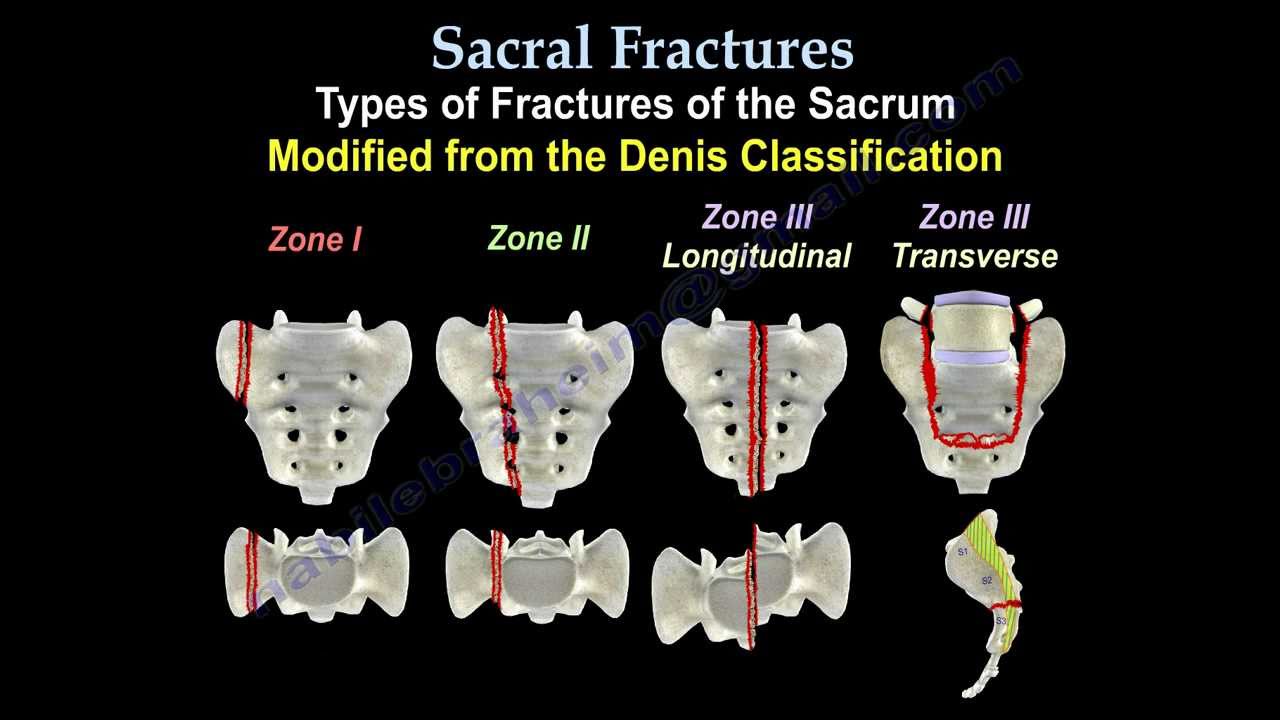
Sacral Fractures – Denis Classification (orthobullets.com)
- Transverse sacral fractures
- Most frequently associated with cauda equina syndrome, lumbosacral or sacral plexus dysfunction
- U-type sacral fractures
- Axial loading injury resulting in spino-pelvic dissociation
- High incidence of neurologic complications
Imaging
- X-Ray
- Often unremarkable. Only shows about 30% of sacral fractures
- Necessary views
- Inlet view best assesses sacral spinal canal and S1
- Outlet view is the true AP of sacrum
- CT: Diagnostic study of choice
- MRI can be obtained if neurologic deficit present
ED Management
- Provide analgesia
- If associated with an unstable pelvis, external fixator such as a pelvic binder is indicated to minimize blood loss
- Definitive treatment largely depends on associated injuries and degree of injury: can range from non-operative to surgical fixation with decompression in patients with neurologic injury
Prognosis
- Largely depends on the extent of the injury.
- Nondisplaced fractures (Zone I or II with stable pelvis) with no associated neurological deficit can be managed nonoperatively with bed rest then progressive weight bearing
- Unstable fractures or those with neurological deficit typically require surgical management. As high as 80% neurological improvement has been reported regardless of surgical v. non-operative management (Vaccaro 2004)
- Many patients may suffer from neurologic sequelae including bladder dysfunction, sexual dysfunction and chronic pain
Take Home Points
- The most common problem in patients with sacral fractures is failure to identify them early on
- Suspect sacral fractures in patients with pelvic ring injuries
- Perform a complete neurologic assessment as the presence of neurologic deficits will require advanced imaging and, likely, surgical intervention
- If you have a high suspicion, CT scan is the imaging modality of choice as plain X-ray will miss most fractures
Read More
Orthobullets: Sacral Fractures
References
Bydon M et al. Sacral fractures. Neurosurg focus. 2014; 37 (1): E12. 24981900
Rodrigues-Pinto R et al. Sacral Fractures and Associated Injuries. Global Spine J 2017; 7(7) :609-616. 28989838
Vaccaro AR et al. Diagnosis and management of sacral spine fractures. Instr Course Lect. 2004;53:375–385. 15116628