INTRODUCTION
- Potentially life-threatening infection of the retropharyngeal space
- Potential space from the base of the skull to the posterior mediastinum
- Retropharyngeal nodes become infected and develop into an abscess
- Retropharyngeal nodes more prominent in young children
- 50% RPA (not due to trauma) occur 6-12 months
- 96% RPA (not due to trauma) occur <6 years
- Risk Factors
- Preceding head and neck infection (otitis, pharyngitis, sinusitis)
- Penetrating trauma: e.g. from a fall with a foreign body in the mouth (toothbrush)
- Airway procedures (intubation, dental procedures, NG tube placement)
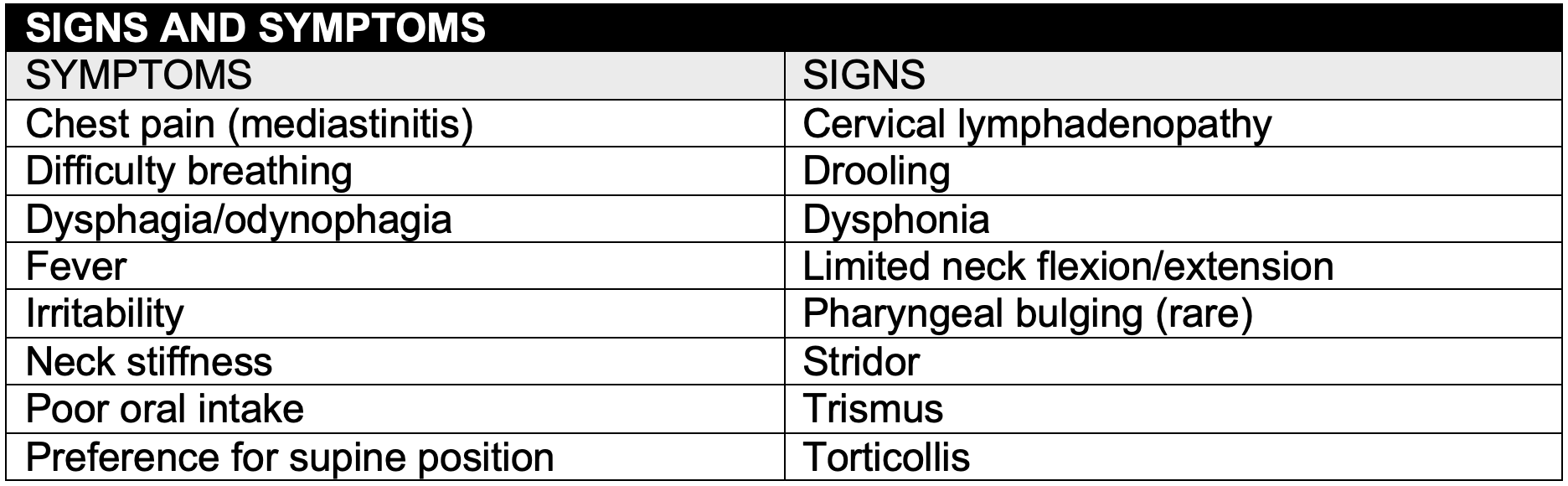
CLINICAL PRESENTATION
- History and physical examination findings are often nonspecific
- Presents with fever, toxic appearance and respiratory distress
- Symptom progression is less acute than epiglottitis
- Fever and neck stiffness may mimic meningitis
- Considered RPA with a severe sore throat and a normal pharyngeal exam
- Patients at risk for airway obstruction should be examined in the OR
LABORATORY TESTING
- Laboratory evaluation may reveal nonspecific elevation in the white blood cell count and acute phase reactants
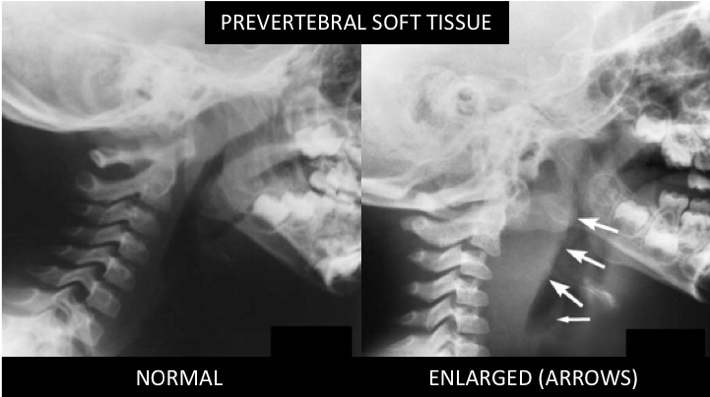
RADIOLOGIC EVALUATION
- Lateral neck soft tissue XRAY: Evaluation of prevertebral soft tissue
- Should be obtained in extension on inspiration: Flexion of the neck, expiration and crying may result in pseudo-enlargement
- Swelling of the prevertebral space
- <1/2 adjacent vertebra width C1-4 or C2 ≤7mm
- <1 adjacent vertebral width C5-8 or C6 ≤14mm (<15 yrs), ≤22mm (>15 yrs)
- Air or an air fluid level
- Loss of normal cervical lordosis due to muscle spasm and inflammation
- Evaluate for epiglottitis and foreign bodies
- Chest XRAY: Pneumonia/empyema and mediastinitis
- Neck CT with contrast: Guide need for operative intervention
- Nature: Cellulitis versus abscess
- Extent: Proximity to vasculature, lateral spread
- ID radiolucent foreign body
- Muscle relaxation due to sedation may precipitate complete airway obstruction
- Requires airway equipment, personnel trained in advanced airway management
MANAGEMENT
- Maintain in a position of comfort (e.g. sitting in their parent’s lap)
- Supportive care: Airway maintenance/monitoring, hydration, analgesia
- Consider: Dexamethasone, nebulized Epinephrine to reduce swelling
SURGERY
- Indications: Have not been definitively established
- Airway compromise
- Large abscess (>2 cm)
- Failed initial antibiotic therapy
ANTIBIOTICS
- Typically polymicrobial
- Gram positive: Group A Strep, Staph aureus (MSSA and MRSA)
- Respiratory anaerobes: Bacteroides, Fusobacterium, Peptostreptococcus
- Rare: Gram (-), Eikenella corrodens, Bartonella hensalae, Mycobacterium TB
- No comparative treatment studies
- Empiric therapy: Group A Strep, Staph aureus, respiratory anaerobes.
- Adjust base on culture and/or clinical response.
- Ampicillin/Sulbactam does not cover MRSA.
- Clindamycin covers MSSA but depending on local resistance does not cover MRSA and some group A Strep.
DISPOSITION
- Admit to PICU for airway monitoring if does not go directly to surgery
REFERENCES
Craig FW, Schunk JE. Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. Pediatrics. 2003 Jun;111(6 Pt 1):1394-8., PMID: 12777558
Page NC, Bauer EM, Lieu JE. Clinical features and treatment of retropharyngeal abscess in children. Otolaryngol Head Neck Surg. 2008 Mar;138(3):300-6., PMID: 18312875
