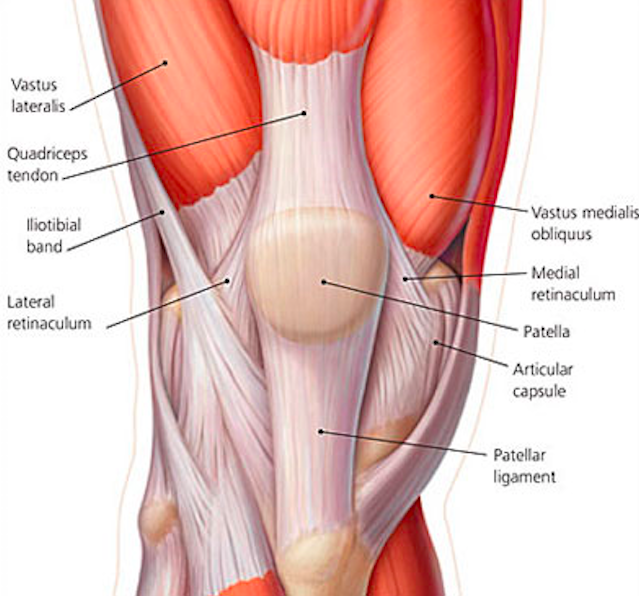
Quadriceps Tendon Anatomy
Background
Definition: Rupture of the tendon attaching the quadriceps muscles to the patella
Anatomy
- The quadriceps muscle is divided into four muscle bellies: vastus medialis, vastus intermedius, vastus lateralis and rectus femoris
- These join together into a single confluence which inserts onto the patella, known as the quadriceps tendon
Epidemiology (Uptodate, Wheeless)
- Location
- Tears usually occur just above the insertion on the patella
- Tears occur twice as often in nondominant leg
- Less common injury than patellar tendon tear
- M:F ratio of 8:1
- Risk factors include: advanced age, anabolic steroid use, renal failure, diabetes, rheumatoid arthritis, hyperparathyroidism, connective tissue disorders, steroid use, intraarticular injections
Presentation (Wheeless)
- Mechanism
- Eccentric loading of the leg while slightly bent, such as a change of direction while running or landing from a jump
- May also occur with a direct blow, particularly in younger patients
- Patients often report a “pop” or tearing sensation
- Patients may complain knee pain, swelling, and difficulty walking
-

Quadriceps Tendon Rupture Physical Exam (eorif.com)
Physical Exam
- Tenderness superior to patella at site of rupture
- Palpable defect superior to the patella
- Swelling of the knee
- Inability to extend the knee against resistance or inability to straight leg raise
- This may be preserved in partial tears

Patella Baja Lateral XRay (orthobullets.com)
Imaging
- Plain X-rays
- Necessary Views: AP and lateral
- Patella baja
- Patella located lower in relation to knee than normal
- Will see in complete tear as patellar tendon displaces patella distally
- May reveal associated patellar fracture
- Patella baja
- Necessary Views: AP and lateral
- Ultrasound can effectively be used to identify quadriceps tendon tears (Pasta)
- Accuracy is operator dependent
- Diagnosed by visualization of ruptured tendon and hematoma
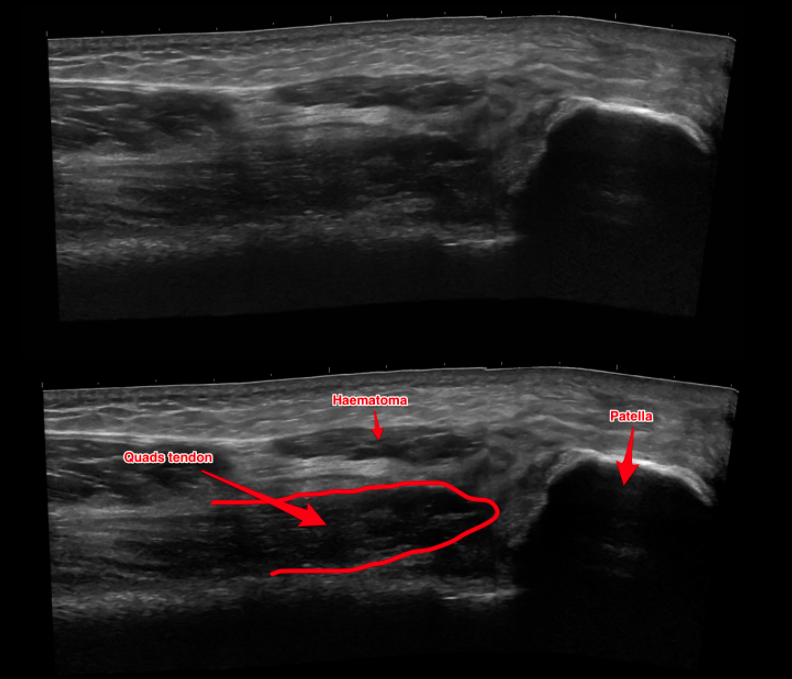
Quadriceps Tendon Rupture Ultrasound (theultrasoundsite.co.uk)
- MRI
- Gold standard to determine whether a tear is partial or complete
- Can determine presence of injury if physical exam, ultrasound, and X-ray inconclusive
- Rarely, if ever, necessary in the ED
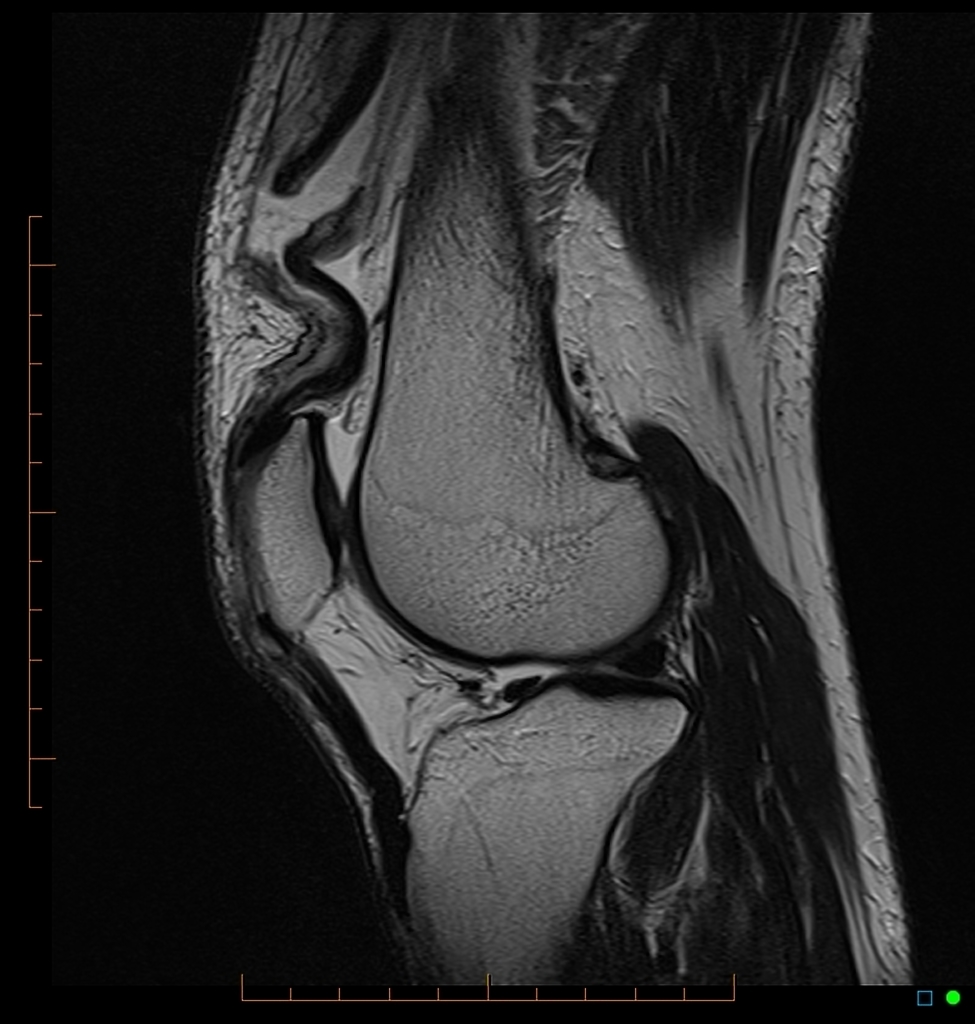
Quadriceps Tendon Rupture MRI (Case courtesy of Dr Chris O’Donnell, Radiopaedia.org. From the case rID: 43540)
ED Management
- Provide analgesia
- Place knee immobilizer and provide crutches
- Knee immobilization crucial for partial tears
- If patient allowed to bear weight on flexed leg, partial tear may progress to complete tear and become operative
- Patients with isolated quadriceps rupture may be discharged from the ED with supportive care measures (rest, ice, elevation, analgesia)
- Emergency orthopedics consultation typically not necessary
- Close follow up with orthopedics (within 1 week) is appropriate as operative management indicated for all complete tears
Prognosis (Wheeless)
- Non-operative management
- Preferred for partial tears so long as the knee extensor mechanism is preserved
- Generally 4-6 weeks of immobilization is recommended with gradual advancement of activities.
- Operative management
- Preferred for complete tears, and for partial tears where the extensor mechanism is not preserved
- Outcomes are much improved if surgery is performed within 1 week
- Surgery performed greater than 2 weeks after injury may result in significant contracture and shortening of the quadriceps tendon, making surgery more difficult and outcomes more poor
- Patients will likely suffer decreased range of motion, decreased extensor strength, and have increased risk of repeat injury
- It is uncommon that patients will be able to return to their former level of activity
- Failed repair, missed concomitant injuries, and infection are the most common complications of surgical repair
Take Home Points
- Missed quadriceps tendon tears can result in significant morbidity. Knee pain with limited ability to extend at the knee or straight leg raise should increase suspicion for this injury
- Quadriceps tendon rupture may result from direct trauma or from axial loading of slightly flexed leg while running or jumping
- For suspected quadriceps tendon rupture, knee X-rays should be obtained to evaluate for patellar fracture. Non-emergent MRI may be needed to differentiate between complete and partial tendon tears
- Patients may be discharged from the ED but will need close follow-up with an orthopedic surgeon to allow for timely surgical repair
Read More:
Orthobullets: Quadriceps Tendon Rupture
Wheeless’ Textbook of Orthopaedics: Rupture of the Quadriceps
References
Bianchi S et al. Ultrasound appearance of tendon tears. Part 2: lower extremity and myotendinous tears. Skeletal Radiol. 2006 Feb;35(2):63-77. PMD: 16382328
McKean J. Quadriceps Tendon Injuries. Link
Pasta G. Sonography of the quadriceps muscle: Examination technique, normal anatomy, and traumatic lesions. J Ultrasound. 2010 Jun; 13(2): 76–84. PMD: 23396806
Perfitt JS et al. Acute quadriceps tendon rupture: a pragmatic approach to diagnostic imaging. Eur J Orthop Surg Traumatol. 2014 Oct;24(7):1237-41. PMD: 23996080
Wheeless CR. Wheeless’ Textbook of Orthopaedics: Rupture of the Quadriceps. Link
Just happened to my husband during vacation in Cabo de San Lucas.
Pulled this info up on my cell phone and found it to be very helpful.
He had a complete tear by first exam and then confirmed by x-ray at local ER. Flew him back to US and had surgery within 72 hours by orthopedic trauma surgeon.
Hope for good outcome