Background
- Useful for evaluation of pleura, chest wall, and pulmonary parenchyma.
- Can differentiate between consolidation, atelectasis, and pleural effusion, findings that are often deemed as indeterminate opacities on chest x-ray. (Carmody 2011)
- Lung ultrasound can be at least as useful as chest x-ray in the pediatric population, offering a radiation-free alternative. (Yilmaz, et al. PMID: 28202294)
- Diagnoses are based on visualized artifacts: ribs create shadows, and normally ventilated lung with air only does not reflect ultrasound, as sound waves scatter when they encounter air. Therefore, we can only visualize lung when it is in fact abnormal! (Carmody 2011)
Indications
- When presented with a patient with undifferentiated dyspnea, chest pain, hypoxia, or as a component of your trauma assessment via the eFAST.
- For use in procedures such as thoracentesis.
Technique
- Probe choice is key as most views will otherwise be obstructed by ribs. The linear and phased array probes are often easiest for sneaking between ribs. Lower frequency probes will allow for deeper penetration into lung parenchyma.
- Jacob Avila (5 minute sono) has a great instructional video:
Evaluation
- There exist 11 common signs necessary for lung ultrasound interpretation. (Lichtenstein, et al. PMID: 24401163)
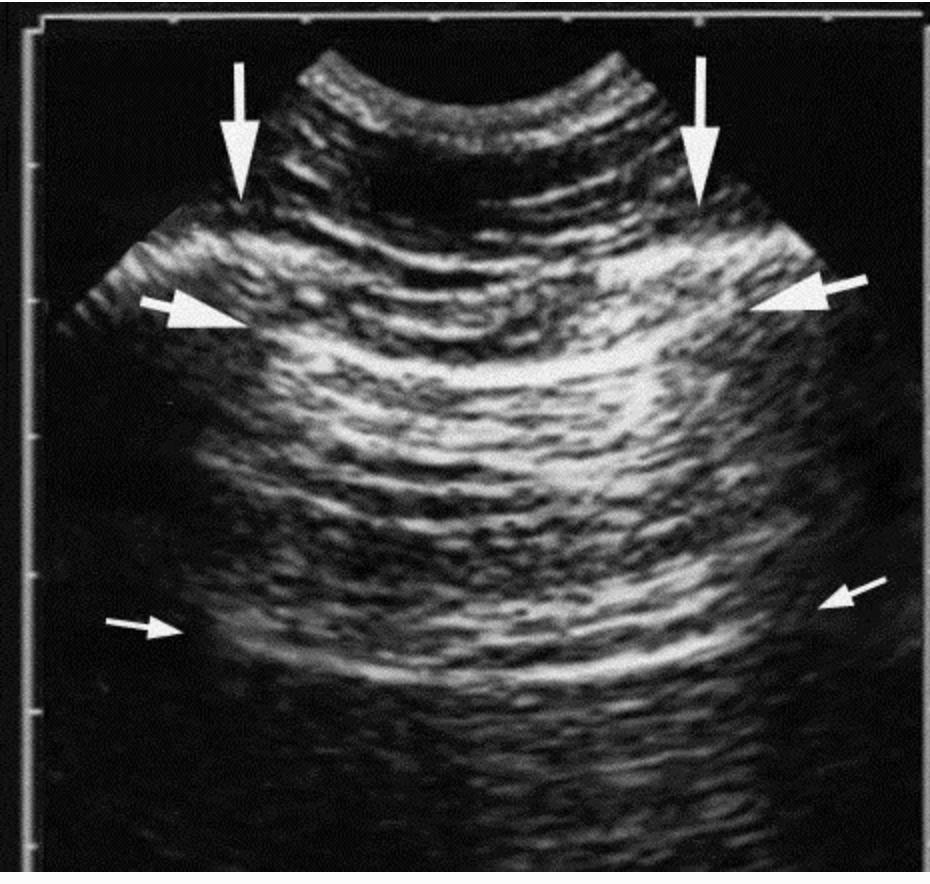
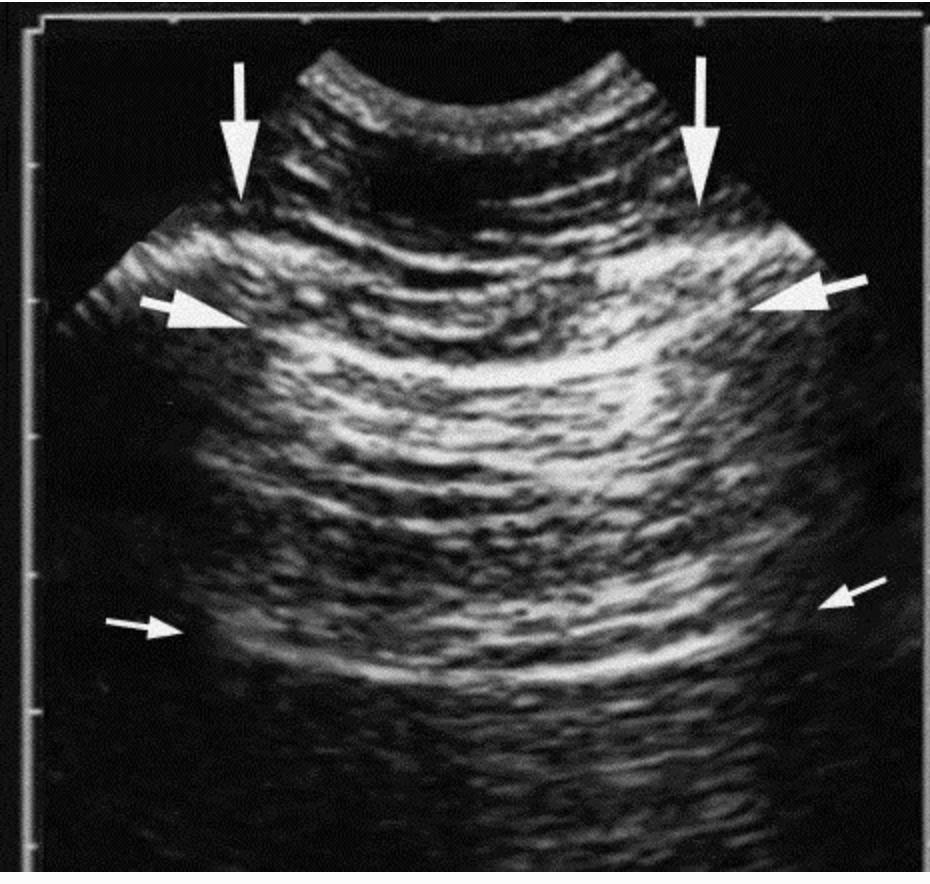
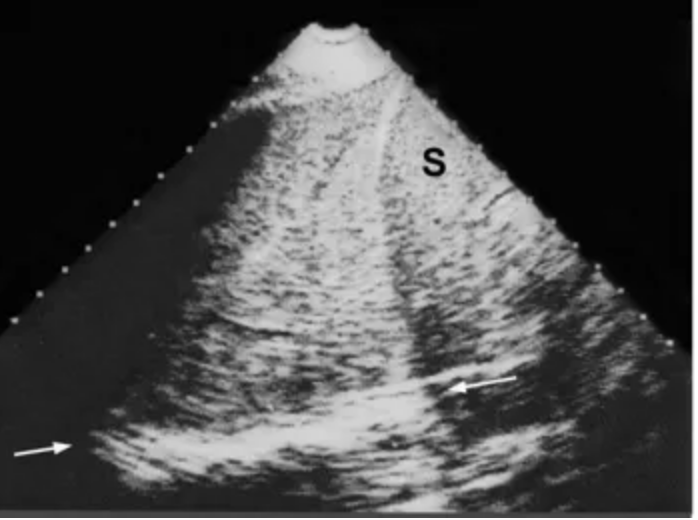
- The bat sign: view created by the pleural line and ribs on either side. This view represents a normal lung surface, where the bright lateral line is the visceral and parietal interface, and the dark “bat wings” are rib shadows.
- A-lines: the horizontal lines (smaller arrows) in figure one. A-lines are artifact, meaning they do not represent anything that is physically present. Instead, it is a consequence of the gas present in the lung beneath the pleural line, creating a reverberation artifact indicated by equidistant horizontal lines descending down the screen.(image: Lichtenstein, et al. PMID: 24401163)
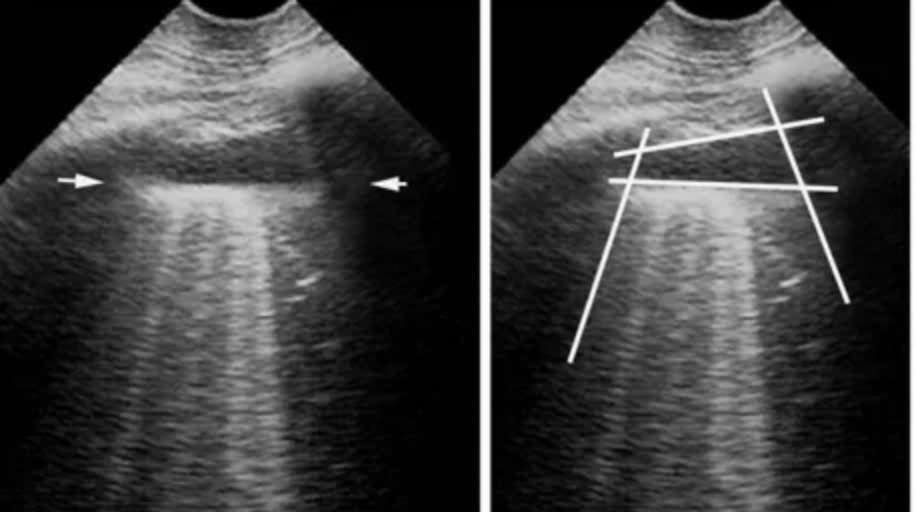
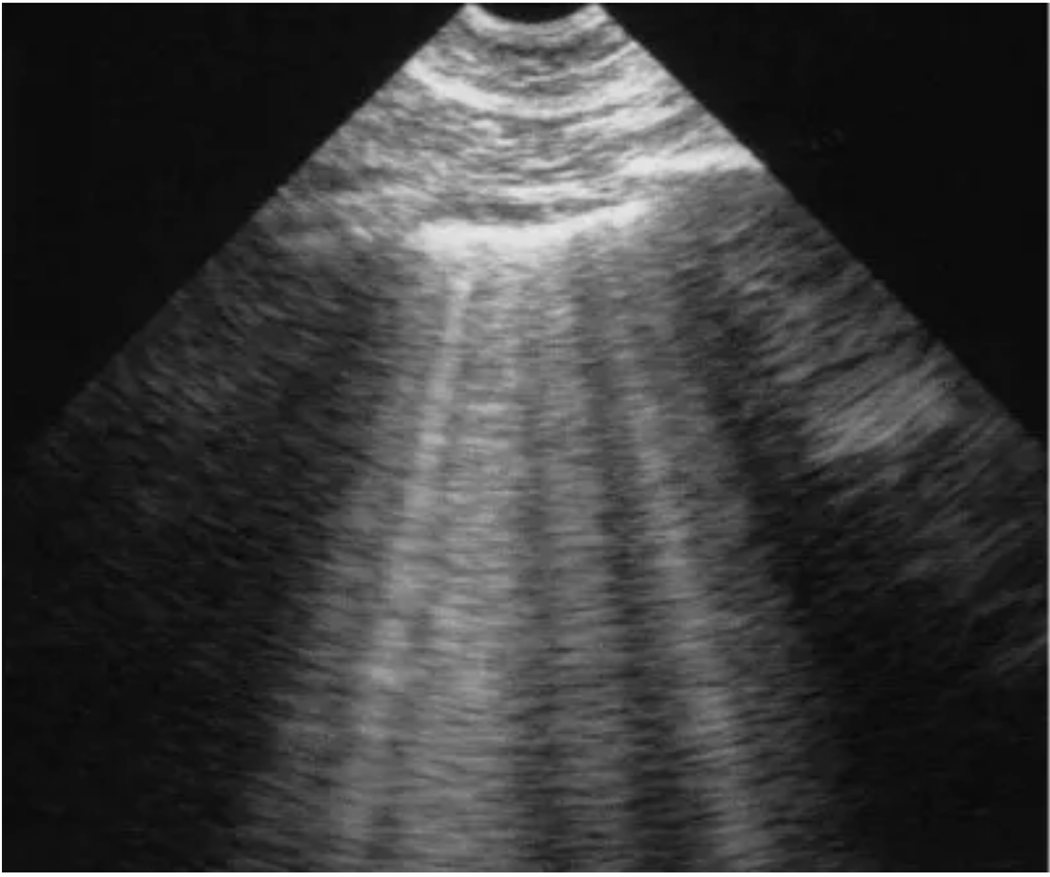
- The quad sign: a pleural effusion in a supine patient. Created by an anechoic pocket of fluid within four borders: two rib shadows, the pleural line and the lung line. As expected, the quad sign is often associated with b lines.(image: Lichtenstein, et al. PMID: 24401163)
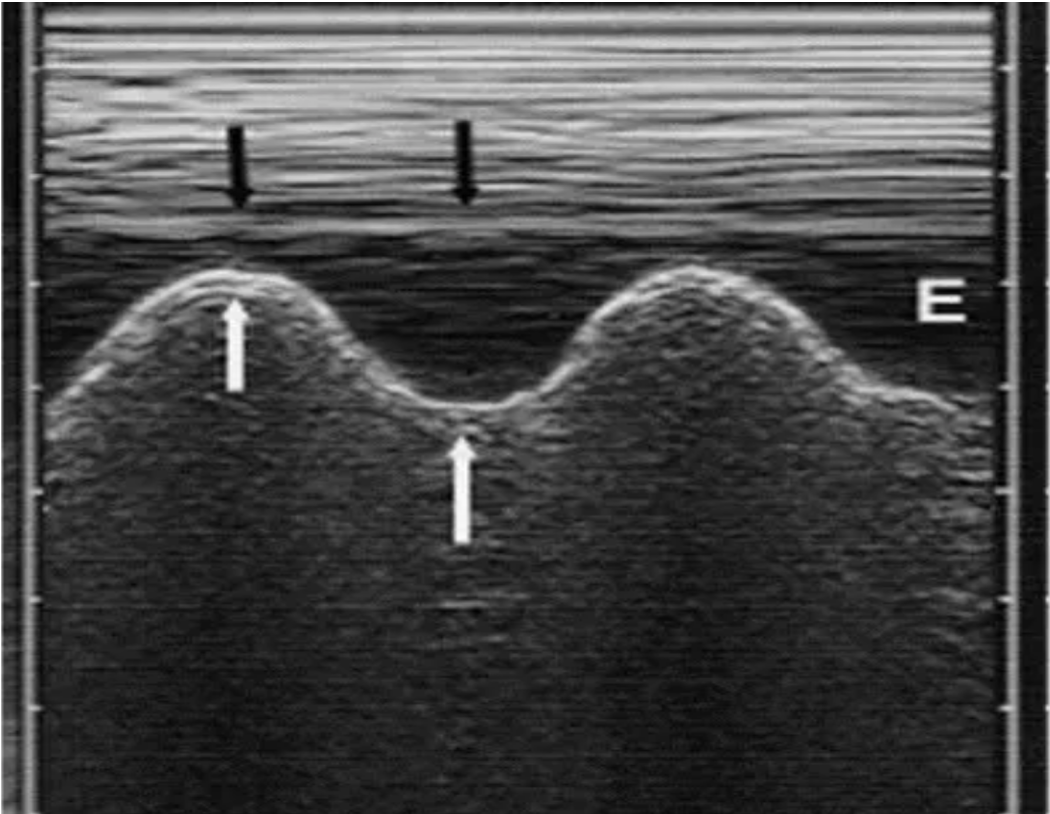
- The sinusoid sign: with a pleural effusion, effect seen when using M-mode during inspiration. As the lung line moves toward the pleural line, we see the image below. (image: Lichtenstein, et al. PMID: 24401163)
- Fractal line: represents consolidation. The boundary of the consolidation with normally aerated lung in the surrounding parenchyma is said to create a shredded, fractal-like boundary. This is only seen when a view captures aerated lung surrounding a consolidation.(image: Lichtenstein, et al. PMID: 24401163)
- Hepatization: if the lung in a single view is consolidated, it will appear “tissue-like,” also referred to as hepatization as its appearance is similar to that of the the liver.(Image: Lichtenstein, et al. PMID: 24401163)
- B-lines: indicate interstitial fluid. As ultrasound waves alternate between air and fluid in the interstitial space, the following lines occur as a result of reverberation artifact. Note that true B-lines obliterate A-lines, and also extend the entire length of the view from top to bottom of the visualized depth. It is commonly expected to see B-lines in the setting of an effusion. (image: Lichtenstein, et al. PMID: 24401163)
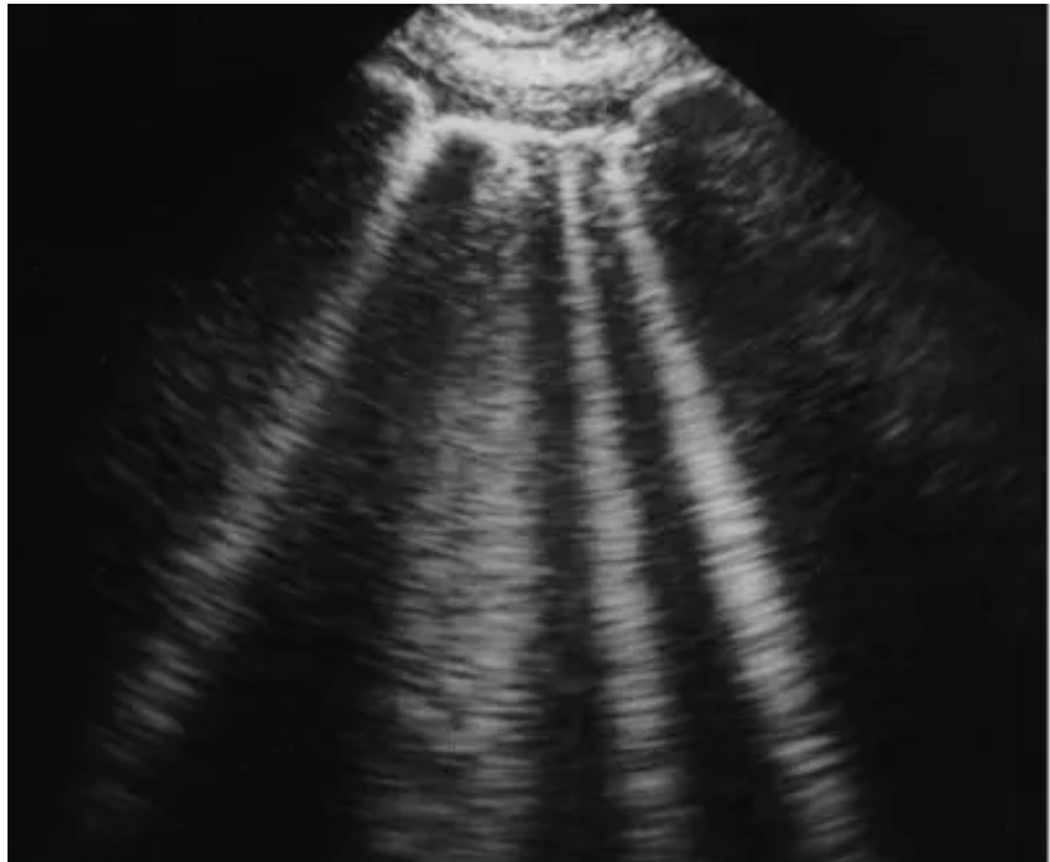
- Lung Rockets: indicate interstitial fluid, defined by 3 or more B-lines between 2 ribs (image: Lichtenstein, et al. PMID: 24401163)
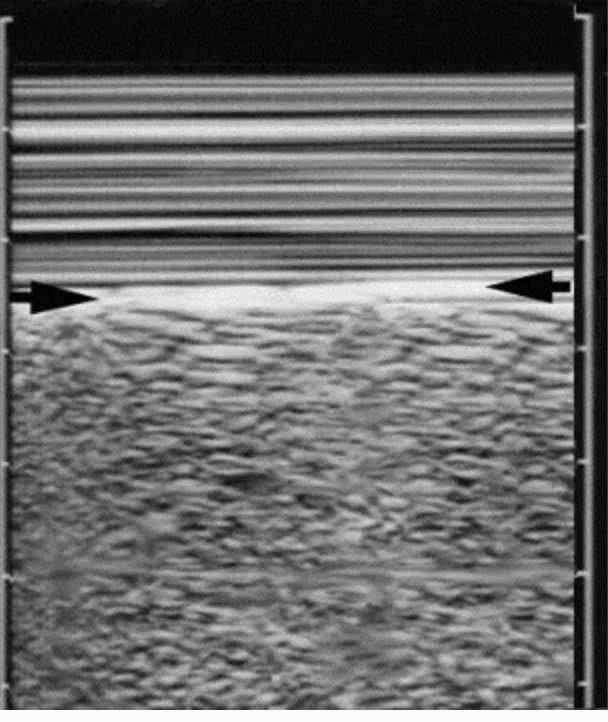
- Barcode or Stratosphere sign: lack of lung sliding using M-mode indicating a pneumothorax. (The presence of lung pleura sliding back and forth creating lung sliding has been found to have 100% negative predictive value for pneumothorax. (Lichtenstein et al., PMID: 7587439)
- Seashore sign: indicating lung sliding on M-mode. While described as a sea above a sandy shore, the important takeaway is that there are 2 distinct patterns created by the motion of lung pleura against the relatively more static chest wall.(image: Lichtenstein, et al. PMID: 24401163)
- Lung point: indicates a pneumothorax at the point where the lung transitions from sliding to no longer sliding. The air creating a pneumothorax prohibits the lung from fully expanding and reaching the chest wall, hence there exists a point at which lung sliding is visible. The size of the pneumothorax can be estimated by identifying the location on the chest wall where the lung point is initially visible.
Common Pitfalls
- Mistaking artifact for pathology. This often happens with B-lines, where a single vertical hyperechoic line may be thought to represent interstitial fluid. Recall that true B-lines are thought only to occur if they are multiple in nature and extend the entire length of the view.
- Lack of practice. The location of the lung presents many obstacles in the form of ribs. Lack of familiarity with expected artifacts such as A-lines can make it much more difficult to interpret accurately if one lacks practice.
Take Home Points
- Lung ultrasound can be an incredibly useful adjunct to assess patients presenting with undifferentiated dyspnea, chest pain, hypoxia, or trauma.
- Practice increases proficiency as lung ultrasound is rich in artifact, and reliable views can be physically difficult due to obstructing ribs.
References
- Carmody, Kristin, et al. Handbook of Critical Care and Emergency Ultrasound. McGraw-Hill Professional, 2011.
- Yilmaz HL, Özkaya AK, Sarı Gökay S, Tolu Kendir Ö, Şenol H. Am J Emerg Med.2017 Jul;35(7):964-969. doi: 10.1016/j.ajem.2017.01.065. Epub 2017 Feb 1.
- http://5minsono.com/lung_scan/
- Lichtenstein, D.A. Lung ultrasound in the critically ill. Intensive Care4, 1 (2014) doi:10.1186/2110-5820-4-1
- Lichtenstein D, Menu Y: A bedside ultrasound sign ruling out pneumothorax in the critically ill: lung sliding.Chest 1995, 108: 1345–1348. 10.1378/chest.108.5.1345
Advanced Reading: The BLUE protocol, developed for rapid assessment of patients with acute respiratory failure. (Lichtenstein, et al. PMID: 24401163)