Background
- Epidemiology:
- Approximately 795,000 people have strokes every year in the US (CDC)
- Posterior circulation strokes account for approximately 20-25% of ischemic strokes (Merwick, 2014)
- Why is it important for ED providers?
- 3% of ED patients present with dizziness, vertigo, lightheadedness, or imbalance (Newman-Toker, 2008)
- We want to avoid ordering MRIs on every patient who presents with a chief complaint of “dizziness”
- In observational study, up to 35% of strokes/transient ischemic attacks were missed by ED physicians in patients who presented with chief complaints of “dizziness”, “vertigo”, or “imbalance” (Kerber, Brown, Lisabeth, Smith, & Morgenstern, 2006)
- Posterior circulation strokes had a higher risk of disability compared to anterior circulation strokes at 3 months according to one study (Kim et al., 2017)
- Half of posterior circulation TIAs present as a brief episode of dizziness (Edlow, 2018)
- Prompt diagnosis and treatment of posterior circulation TIAs can prevent future strokes (Edlow, 2018)
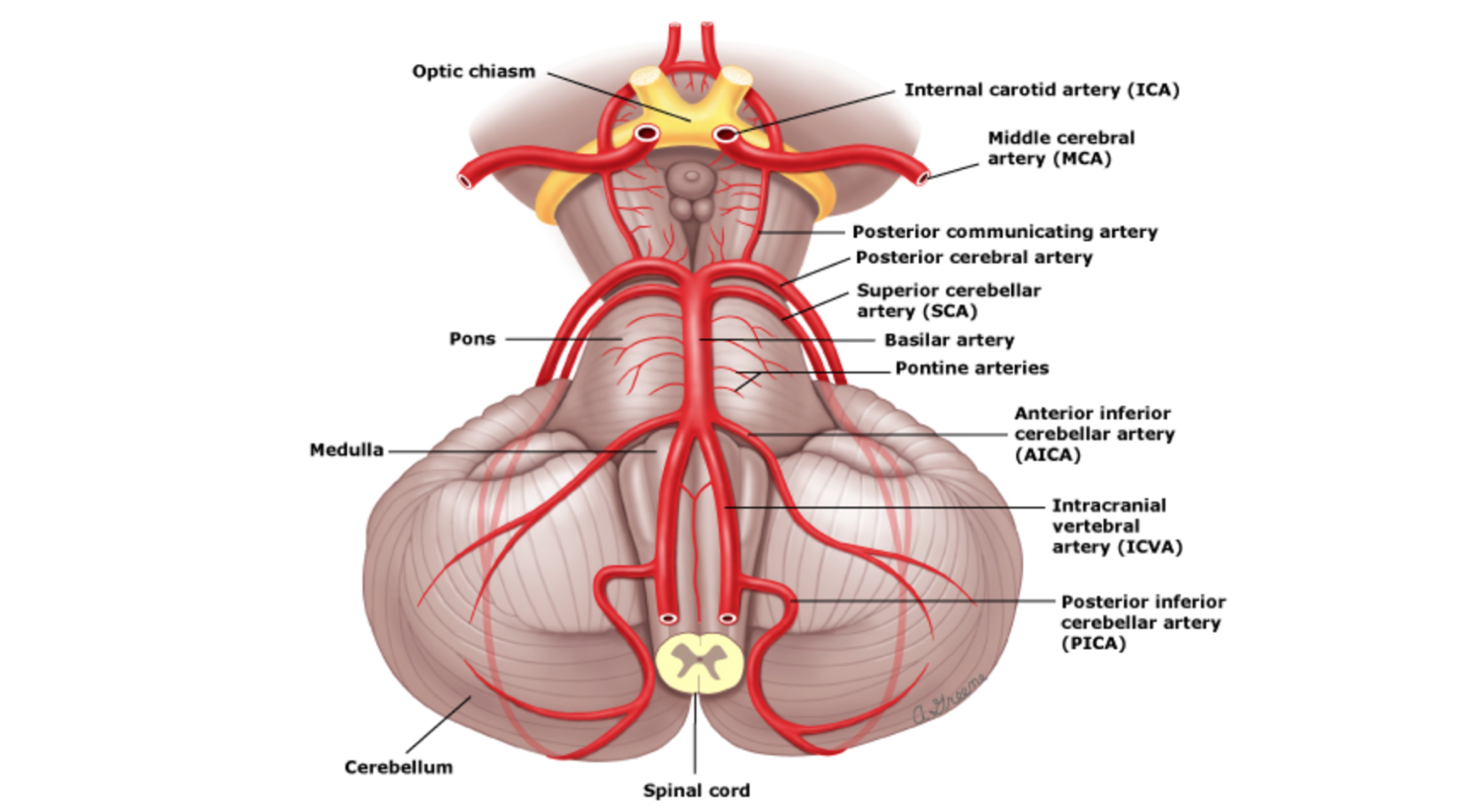
Anatomy of Posterior Circulation (Caplan and UpToDate)
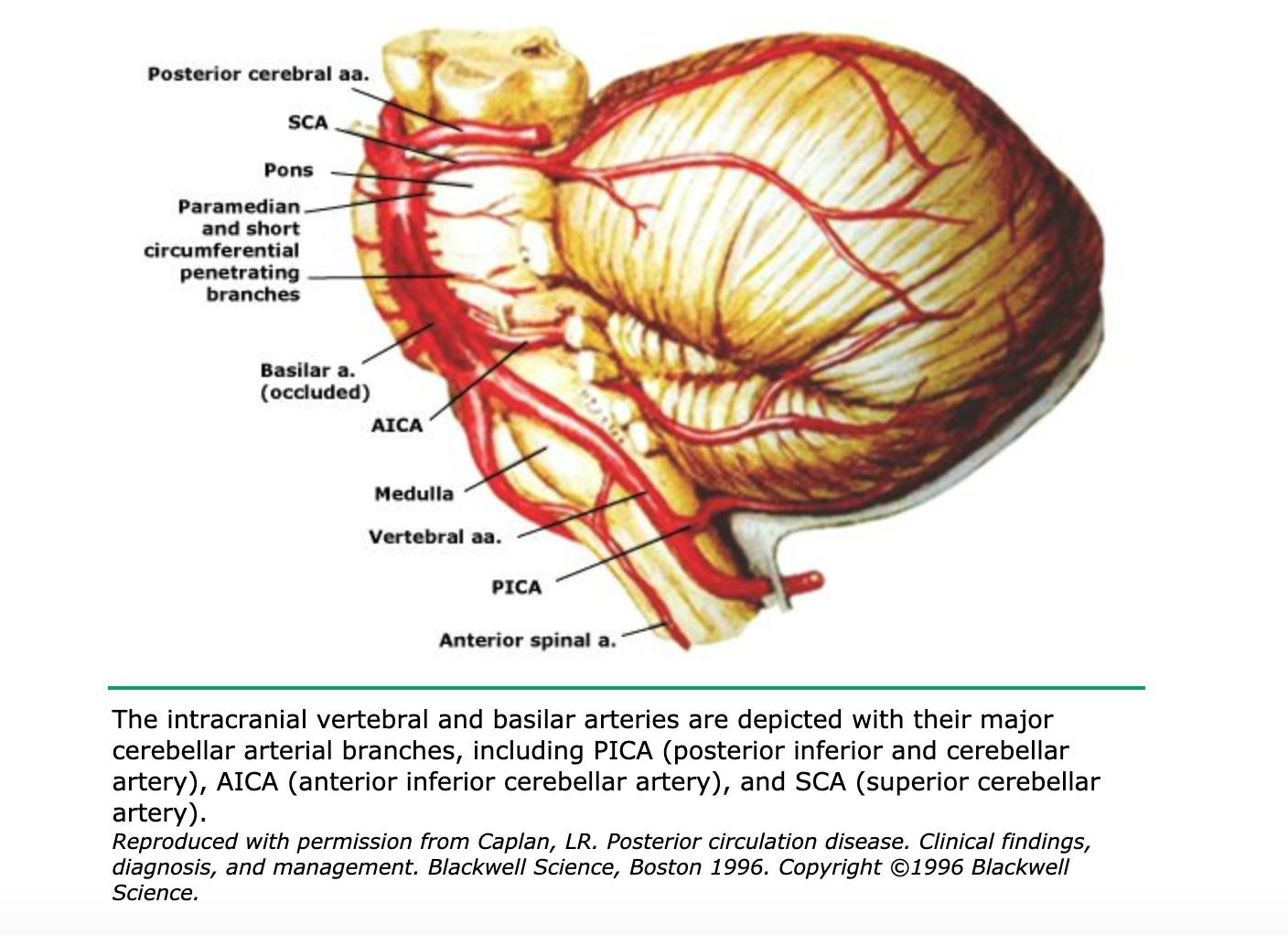
Major Cerebellar Artery Branches (Caplan and UpToDate)
Etiology
- Embolic stroke is most common ischemic cause (Caplan et al., 2004)
- Atherosclerotic plaque-related ischemia next most common
- Hemorrhagic rarer, presents similarly to ischemic
- Vertebral dissection also can cause posterior ischemic stroke; consider in younger patients with neck trauma and neck pain or any patient on anticoagulation (Arnold et al., 2006)
Types and Locations of Posterior Circulation Stroke
- 35% lobar, 49% deep cerebral, 6% brain stem, 10% cerebellar (Flaherty et al., 2005)
- Posterior Cerebral Artery Infarction (Distal Posterior Circulation)
- Basilar Artery Occlusion (Middle Posterior Circulation)
- Vertebrobasilar Infarction (Proximal Posterior)
- Cerebellar Infarction
Risk Factors
- Similar to risk factors of all types of cerebrovascular disease (Benjamin et al., 2019)
- Head trauma
- HTN
- DM
- Heart rhythm disorders
- Obesity
- Hyperglycemia
- HLD
- Renal dysfunction
- Behavioral: Smoking, sedentary lifestyle, unhealthy diet
- Nonmodifiable: family history/genetics
Presentation
- Can be very subtle
- Typical findings: ataxia, nystagmus, altered mental status, vertigo/dizziness, nausea/vomiting, headache, dysarthria, unilateral limb weakness, blurry vision (Tintinalli et al., 2016)
- Suggestive specific findings:
- Posterior cerebral artery – contralateral homonymous hemianopsia and unilateral cortical blindness (visual centers supplied by posterior cerebral artery)
- Basilar artery – dysphagia, dysarthria, sudden loss of consciousness, rarely Locked-in syndrome, ataxia
- Vertebrobasilar artery –Horner’s syndrome, ataxia
- Brainstem – Crossed neurological symptoms (e.g. ipsilateral cranial nerve deficit with contralateral motor weakness)
Differential Diagnosis
- Central Causes:
- Toxicologic etiology
- Traumatic brain injury
- Intracranial hemorrhage – Subarachnoid, Subdural, Epidural, intraparenchymal
- Common carotid dissection
- Vertebral artery dissection
- Infection – encephalitis, neurosyphilis, meningitis, TB
- Seizure
- Posterior Reversible Encephalopathy Syndrome
- Peripheral Causes:
- Peripheral infection including neuritis, labyrinthitis
- Benign paroxysmal peripheral vertigo
- Meniere’s disease
- Aminoglycoside toxicity
- Vestibular Schwannoma
- Acute Otitis Media
- Other Potential Causes of Dizziness:
- Wernicke’s Encephalopathy
- Electrolyte disturbances
- Cardiac dysrhythmias
- Acute Coronary Syndrome
- Anemia
- Hypoglycemia – Always get a fingerstick as part of triage for this chief complaint
- Uremia
- Hypo/hyperthyroidism
- Multiple sclerosis
- Medication/drug toxicity: Lithium, alcohol
Peripheral vs Central Vertigo (Tintinalli et al., 2016)
- Peripheral Vertigo:
- Sudden or insidious onset
- Intermittent symptoms
- Intense severity
- Headache uncommon
- Cranial nerves intact
- Symptoms worse with head movement
- Central Vertigo:
- Sudden onset
- Symptoms commonly persistent/ constant
- Poorly defined severity
- Headache possible
- Cranial nerves deficiency may be present
- Symptoms may be worse with head movement
Diagnosis
- Thorough history and physical exam
- History: onset, timing, severity, aggravating/alleviating symptoms
- NIHSS
- Physical exam: cranial nerve exam, visual fields, eye movements, gait (try to always walk the patient), finger to nose, pronator drift
- HINTS exam (see next section)
HINTS Exam
*See Dr. Newman Toker’s demonstration of the HINTS exam here
- Important distinction: Should never be doing Dix-Hallpike AND HINTS on same patient; these exams should be performed only on patients having active symptoms in the ED
- Dix-Hallpike used for intermittent, triggered, positional acute vestibular syndrome
- HINTS exam used for constant, non-episodic acute vestibular syndrome
- HINTS exam is more sensitive and more specific for posterior stroke compared to DWI MRI (Kattah, Talkad, Wang, Hsieh, & Newman-Toker, 2009)
- 101 high risk patients with Acute vestibular syndrome had 100% sensitivity, and 96% specificity for posterior circulation stroke
- If any of the below have concerning findings, then exam is worrisome for central etiology of acute vestibular syndrome (Edlow, Gurley, & Newman-Toker, 2018)
- Head Impulse
- Rotate head 20-30 degrees then back to center with quick smooth movement (avoids rapid/violent neck movement)
- Peripheral: corrective saccade
- Central: Fixed on nose entire time (normal in non-vertiginous patient BUT worrisome in vertiginous patient)
- Nystagmus
- Don’t tell patient to focus on finger – fixation can suppress nystagmus – hold up a sheet of paper to one side of patient’s head and tell them to look at the paper
- Peripheral: unidirectional fast beating (same direction of fast beating despite patient’s gaze)
- Central: bidirectional, vertical
- Test of Skew
- Cover one eye, tell them to focus on nose, then quickly move hand to cover the other eye
- Peripheral: no corrective gaze
- Central: vertical/ diagonal corrective movement with eye immediately uncovered
- Head Impulse
Intepreting HINTS Video (courtesy of Jay Lin, MD)
Imaging
- American College of Radiology Appropriateness Criteria Recommendations 2016:
- New focal neurologic deficit <6 hours, suspected stroke – NCHCT (assess for large infarct or hemorrhage), MRI (more sensitive than CT for ischemic stroke); recommend NCHCT followed by MRI
- New focal neurologic deficit, >6 hours, suspected stroke – MRI (more sensitive than CT for ischemic stroke), more appropriate in this setting than CT
- Computed Tomography:
- NCHCT – easily obtained, fast, used for ruling out acute bleed/hemorrhage
- Retrospective study showed NCHCT with sensitivity of 47% compared to gold standard of DWI MRI (Hwang, Silva, Furie, & Greer, 2012)
- Prospective study showed NCHCT sensitivity of 16% in ischemic stroke and 26% in all stroke (Chalela et al., 2007)
- Consider CT Angiogram if concerned for dissection of vertebrobasilar arteries
- MRI:
- DWI MRI is gold standard for evaluation of acute stroke
- Sensitivity is decreased within the first 24 hours in comparison to anterior circulation strokes (Oppenheim et al., 2000)
- Always ask for thin cuts through the brainstem to increase diagnostic accuracy
Management
- Thrombolysis:
- Thrombolysis with Alteplase has been shown to benefit ischemic strokes within4.5 hours from onset of symptoms (Hacke et al., 2008)
- Posterior strokes often are outside the window for thrombolysis due to delayed or missed diagnosis
- If identified within the window for thrombolysis, thrombolysis for posterior circulation strokes was found to have no worsened risks and similar benefits as compared to patients who received thrombolysis for anterior circulation ischemic events (Forster et al., 2011)
- Thrombectomy:
- No great US studies; German study involving 139 patients showed that mechanical thrombectomy for posterior circulation stroke had no statistically different rates of mortality and had similar rates of recovery at discharge and 6 months out compared to anterior circulation strokes (Weber et al., 2019)
- Patients had statistically significant decreased risk of hemorrhage when compared to anterior circulation thrombectomy (Weber et al., 2019)
- Be wary of the complication of cerebellar edema leading to herniation or obstructive hydrocephalus – if more than one third of a cerebellar hemisphere is affected, get emergent neurosurgical evaluation, and monitor the patient’s airway closely
- Standard protocol for stroke patients if not receiving thrombolysis or thrombectomy:
- Head of bed > 30 degrees
- Oxygen saturation > 94%
- Anti-hypertensive medication so BP <220/120, OR <180/105 if patient is receiving thrombolysis; contact stroke team for further recommendations for blood pressure control
- Aspirin administration immediately once hemorrhage is ruled out
Take-Home Points
- Although posterior stroke symptoms account for a small part of all strokes, the diagnosis tends to be missed/overlooked with serious implications for patients
- Posterior stroke symptoms can be subtle and easy to miss
- Keep posterior circulation stroke as part of your differential for any dizzy patient
- Learn the HINTS exam and how to perform it properly; findings on HINTS exam can be confusing, so either study them well, or use an online resource if needed
- Treat posterior strokes with thrombolysis, thrombectomy, or conservative management depending on clinical picture
Special thanks to Dr. Jose Torres, MD (Assistant Professor, Department of Neurology, NYU Langone)
References
Dewey HM, Sturm J, Donnan GA, Macdonell RA, McNeil JJ, Thrift AG; North East Melbourne Stroke Incidence Study. Incidence and Outcome of Subtypes of Ischaemic Stroke: Initial Results from the North East Melbourne Stroke Incidence Study (NEMESIS). Cerebrovasc Dis2003;15:133-9.
Edlow, J. Managing Patients With Acute Episodic Dizziness. Ann Emerg Med. 2018;72;602-610.
Newman-Toker, D.E., Hsieh, Y.H., Camargo, C.A. Jr. et al. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin Proc. 2008; 83: 765–775.
Merwick A. Posterior circulation ischaemic stroke. BMJ 2014;348:g3175.
Caplan MD. Posterior circulation cerebrovascular syndromes. (2018, April 30). UpToDate. Retrieved October 31, 2019, from https://www.uptodate.com/contents/posterior-circulation-cerebrovascular-syndromes.
American College of Radiology. ACR Appropriateness Criteria. Available at https://acsearch.acr.org/list. Accessed <10/31/2019>.
Arnold, M., Bousser, M. G., Fahrni, G., Fischer, U., Georgiadis, D., Gandjour, J., . . . Baumgartner, R. W. (2006). Vertebral artery dissection: presenting findings and predictors of outcome. Stroke, 37(10), 2499-2503. doi:10.1161/01.STR.0000240493.88473.39
Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W., Carson, A. P., . . . Stroke Statistics, S. (2019). Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation, 139(10), e56-e528. doi:10.1161/CIR.0000000000000659
Caplan, L. R., Wityk, R. J., Glass, T. A., Tapia, J., Pazdera, L., Chang, H. M., . . . Pessin, M. S. (2004). New England Medical Center Posterior Circulation registry. Ann Neurol, 56(3), 389-398. doi:10.1002/ana.20204
Chalela, J. A., Kidwell, C. S., Nentwich, L. M., Luby, M., Butman, J. A., Demchuk, A. M., . . . Warach, S. (2007). Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet, 369(9558), 293-298. doi:10.1016/S0140-6736(07)60151-2
Edlow, J. A., Gurley, K. L., & Newman-Toker, D. E. (2018). A New Diagnostic Approach to the Adult Patient with Acute Dizziness. J Emerg Med, 54(4), 469-483. doi:10.1016/j.jemermed.2017.12.024
Flaherty, M. L., Woo, D., Haverbusch, M., Sekar, P., Khoury, J., Sauerbeck, L., . . . Broderick, J. P. (2005). Racial variations in location and risk of intracerebral hemorrhage. Stroke, 36(5), 934-937. doi:10.1161/01.STR.0000160756.72109.95
Forster, A., Gass, A., Kern, R., Griebe, M., Hennerici, M. G., & Szabo, K. (2011). Thrombolysis in posterior circulation stroke: stroke subtypes and patterns, complications and outcome. Cerebrovasc Dis, 32(4), 349-353. doi:10.1159/000330346
Hacke, W., Kaste, M., Bluhmki, E., Brozman, M., Davalos, A., Guidetti, D., . . . Investigators, E. (2008). Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med, 359(13), 1317-1329. doi:10.1056/NEJMoa0804656
Hwang, D. Y., Silva, G. S., Furie, K. L., & Greer, D. M. (2012). Comparative sensitivity of computed tomography vs. magnetic resonance imaging for detecting acute posterior fossa infarct. J Emerg Med, 42(5), 559-565. doi:10.1016/j.jemermed.2011.05.101
Kattah, J. C., Talkad, A. V., Wang, D. Z., Hsieh, Y. H., & Newman-Toker, D. E. (2009). HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke, 40(11), 3504-3510. doi:10.1161/STROKEAHA.109.551234
Kerber, K. A., Brown, D. L., Lisabeth, L. D., Smith, M. A., & Morgenstern, L. B. (2006). Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke, 37(10), 2484-2487. doi:10.1161/01.STR.0000240329.48263.0d
Kim, J. T., Park, M. S., Choi, K. H., Kim, B. J., Han, M. K., Park, T. H., . . . Cho, K. H. (2017). Clinical Outcomes of Posterior Versus Anterior Circulation Infarction With Low National Institutes of Health Stroke Scale Scores. Stroke, 48(1), 55-62. doi:10.1161/STROKEAHA.116.013432
Oppenheim, C., Stanescu, R., Dormont, D., Crozier, S., Marro, B., Samson, Y., . . . Marsault, C. (2000). False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR Am J Neuroradiol, 21(8), 1434-1440.
Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Cline, D., Meckler, G. D., & Yealy, D. M. (2016). Tintinalli’s emergency medicine : a comprehensive study guide (Eight edition. ed.). New York: McGraw-Hill Education.
Weber, R., Minnerup, J., Nordmeyer, H., Eyding, J., Krogias, C., Hadisurya, J., . . . investigators, R. (2019). Thrombectomy in posterior circulation stroke: differences in procedures and outcome compared to anterior circulation stroke in the prospective multicentre REVASK registry. Eur J Neurol, 26(2), 299-305. doi:10.1111/ene.13809
HINTS video: Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov;40(11):3504-10. https://vimeo.com/133033089

Hey Mukul, nice job on posterior circulation stroke!
A couple of points.
1. You should only perform HINTS on patients WITH spontaneous or gaze evoked nystagmus.
https://youtu.be/L4nOD8YdV-s
2. The head impulse test should be done abruptly and quickly, not smoothly.
https://youtu.be/XpghlvnrREI?t=665
3. The statement that “Half of posterior circulation TIAs present as a brief episode of dizziness” attributed to Edlow is not factually correct. The reference Edlow gave is Paul in the Lancet 2013.
I think most doctors would agree that “the patient presents with” means that they complain of a certain symptom or symptoms to a medical professional, and not just that they have it but don’t seek medical attention for it.
In Paul’s study, they identified posterior stroke patients and asked them to fill out a questionnaire about symptoms that had, and care they sought, before their stroke.
Only 16% said they had some kind of dizzy/vertigo spell before their stroke. And despite the UK having universal health care, and in Paul’s study there was an open access TIA service available for primary care and emergency doctors to refer to 7 days a week, less than 4% of the patients with posterior circulation stroke sought medical care for their little dizzy episode that occured before their stroke.
We can’t save those who don’t come to see us, and recommending that all patients with transient dizziness rush to the ED is not something most would recommend. Vestibular migraine is by far the most common cause of episodic isolated dizziness that is not BPPV. Suggesting that half the patients with a posterior circulation stroke “present” with dizziness before their stroke stroke will lead to over investigation and treatment of what usually is a benign process, such as vestibular migraine, which can be diagnosed by history. https://youtu.be/XPIyXiv0UKg
I should be coming out with a new video entitled “Is isolated transient vertigo ever a TIA?” in the next few weeks, where I will go over this topic in more detail.
Keep up the good work!
Peter
Great post Mukul… thank you.
I just have a question. Recently, I went thought the 2019 AHA/ASA stroke guidelines and the only thing mentioned on cerebellar stoke is about surgical decompression of posterior fossa strokes, but nothing on medical management. Do you of Dr Torres have any reference for lyrics on these type of strokes. Not just articles, but actual guidelines from any Organization.
Thanks
Great post Mukul… thank you.
I just have a question. Recently, I went thought the 2019 AHA/ASA stroke guidelines and the only thing mentioned on cerebellar stoke is about surgical decompression of posterior fossa strokes, but nothing on medical management. Do you of Dr Torres have any reference for lyrics on these type of strokes. Not just articles, but actual guidelines from any Organization.
Very good and useful to review in short with tons of information.
Thanks