Definition:
The International Headache Society (IHS) criteria for diagnosis of a post-dural puncture headache (PDPH) requires that the headache meet all four of the following criteria (IHS 2004):
- Occurs after dural puncture,
- Develops within 5 days of LP,
- Worsens within 15 minutes after sitting or standing and improves within 15 min after lying down and is associated with either neck stiffness, tinnitus, hypoacusia, photophobia, or nausea
- Either resolves spontaneously in 1 week or within 48 hours after effective treatment
Issues with Definition:
- As many as a 33% of patients with PDPH do not meet these criteria due to:
- lack of associated symptoms or
- headache lasting longer than 1 week (Amorin 2012)
- Criteria 4 requires resolution of the headache before definitive diagnosis making it impossible to apply these criteria in the ED
- Suspicion for PDPH after an LP should be high even in absence of all of the qualifying diagnostic criteria, especially in higher risk patients, which include women, pregnant patients and young adults (Amorin 2012)
- Remember to keep your differential broad: while headaches in the postpartum period are common, less than 20% are actually attributable to PDPH (Bezov 2010)
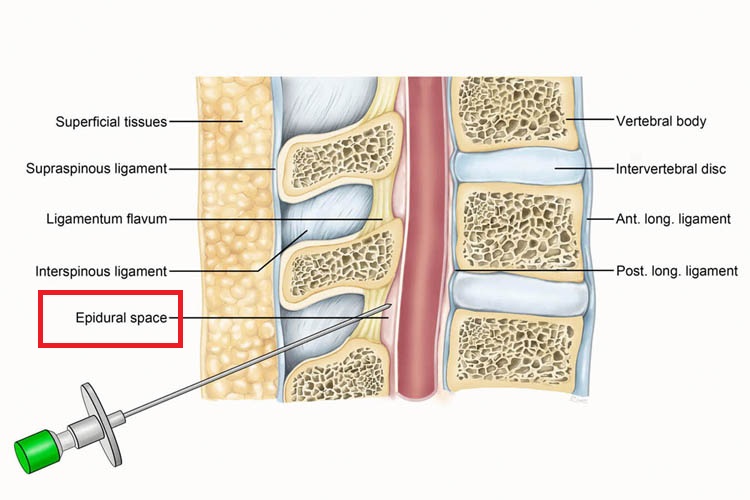
Spinal Anatomy (Kevinlimd.com)
Epidemiology:
- 10-30% of patients post-LP will develop a headache (Bezov 2010)
- Likely underreported
Pathophysiology: The pathophysiology leading to headache is thought to be persistent leakage of cerebral spinal fluid (CSF) from the puncture site causing low CSF pressure and volume (Bezov 2010).
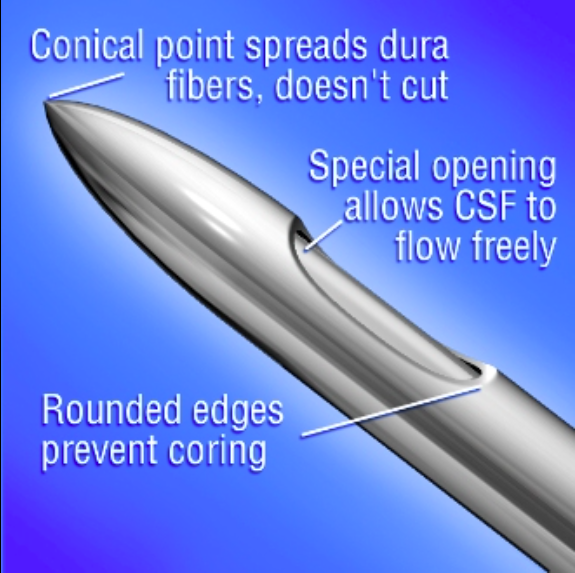
Non-Cutting Needle (sinoprochem.en.alibaba.com)
Prevention:
- There has been a large volume of research on methods thought to reduce the risk of PDPH (Arevalo-Rodriguez 2016, Strupp 1998, Lin 2002, Ahmed 2006).
- Techniques with supportive evidence
- Use of higher gauge needle, (at least 22 gauge)
- Use of atraumatic needle
- Orienting the bevel in parallel with the fibers of the dura
- Replacing the stylet prior to removal
- Techniques where the evidence shows no benefit
- Having the patient lay flat post procedure
- Removing small volume of CSF
- Positioning on patient’s side during procedure
- Giving IVF after procedure
- Techniques that need more evidence
- Number of LP attempts
- Giving IVF prior to procedure
Treatment:
- Conservative therapy: NSAIDs, antiemetics, hydration (Swanson 2014)
- Pros: easy, cheap, low side effect profile
- Cons: low efficacy in PDPH, usually given in first 24 hours postponing definitive diagnosis
- Targeted therapy:

- Caffeine: administration of 500mg (0.5g/2mL) caffeine IV
- Pros: cheap
- Cons: mixed evidence (Busorto 2011), requires large doses
- Epidural blood patch
- Procedure: 20cc of the patient’s blood is drawn from a peripheral vein in sterile technique and then the blood is injected into the epidural space using a large bore needle
- Pros: superior to both placebo/sham treatment and conservative treatment (Boonmak 2010)
- Cons: invasive, requires consultation, backache (Boonmak 2010)
- Caffeine: administration of 500mg (0.5g/2mL) caffeine IV
Take Home Points:
- Post dural-puncture headache affects up to 30% of patients after lumbar puncture.
- Suspect PDPH in all patients who recently underwent an LP or epidural anesthesia regardless of whether they meet the IHS criteria.
- The best way to treat PDH is to prevent it from developing. Techniques proven to reduce risk include higher gauge needle use, atraumatic needle use, reduced LP attempts, and replacing stylet prior to removal.
- Patients with PDPH refractory to standard therapy should be considered for a blood patch.
REBEL EM: Post Lumbar Puncture Headaches
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24: 9–160. PMID: 14979299
Amorim JA et al. Post-dural (post-lumbar) puncture headache: risk factors and clinical features. Cephalalgia. 2012; 32(12):916-23. PMID: 22843225
Bezov D et al. Post-dural puncture headache: Part I diagnosis, epidemiology, etiology and pathophysiology. Headache. 2010;50:1144-1152. PMID: 20533959
Hammond ER et al. Needle type and the risk of post-lumbar puncture headache in the outpatient neurology clinic. J Neurol Sci. 2011;306(1-2):24-8. PMID: 21549395
Arevalo-Rodriguez I et al. Posture and fluids for preventing post-dural puncture headache. Cochrane Database of Systematic Reviews. 2016 Mar 7;3:CD009199. doi: 10.1002/14651858.CD009199.pub3. PMID: 26950232
Strupp M et al. Incidence of post-lumbar puncture syndrome reduced by reinserting the stylet: a randomized prospective study of 600 patients. J Neurol. 1998 Sep;245(9):589-92. PMID: 9758296
Lin W, Geiderman J. 2002. Myth: fluids, bed rest, and caffeine are effective in preventing and treating patients with post-lumbar puncture headache. West J Med. 2002 Jan;176(1):69-70. PMID: 11788546
Ahmed SV et al. Post lumbar puncture headache: diagnosis and management. Postgrad Med J. 2006 Nov; 82(973): 713–716. PMID: 17099089
Swanson JW. Post-lumbar puncture headache. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2014. Link
Basurto Ona X et al. Drug therapy for treating post-dural puncture headache. Cochrane Database Syst Rev. 2011 Aug 10;(8):CD007887. doi: 10.1002/14651858.CD007887.pub2. PMID: 21833962
Boonmak P, Boonmak S. Epidural blood patching for preventing and treating post-dural puncture headache. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD001791. doi: 10.1002/14651858.CD001791.pub2. PMID: 20091522
Hey
Great article, as with most stuff on this website. Replacing the stylet to reduced headache is one I’d not heard before so thanks for including this.
Just a note on the wording of your take home points: “Techniques proven to reduce risk include large guage needle use” implies larger needles would be associated with reduced headache. I assume this is just a typo and maybe “higher” Guage needle or would be less confusing term.
Thanks for all the great articles you guys post
Sam
Sam – excellent point. We’ve updated the post. Thanks!